World J Mens Health.
2017 Aug;35(2):100-106. 10.5534/wjmh.2017.35.2.100.
Evaluation of Impact of Voiding Posture on Uroflowmetry Parameters in Men
- Affiliations
-
- 1Department of Urology, King George's Medical University, Lucknow, India. drashokkumarsokhal@gmail.com
- KMID: 2388445
- DOI: http://doi.org/10.5534/wjmh.2017.35.2.100
Abstract
- PURPOSE
To evaluate the impact of voiding position on uroflowmetry parameters and to assess its potential clinical implications.
MATERIALS AND METHODS
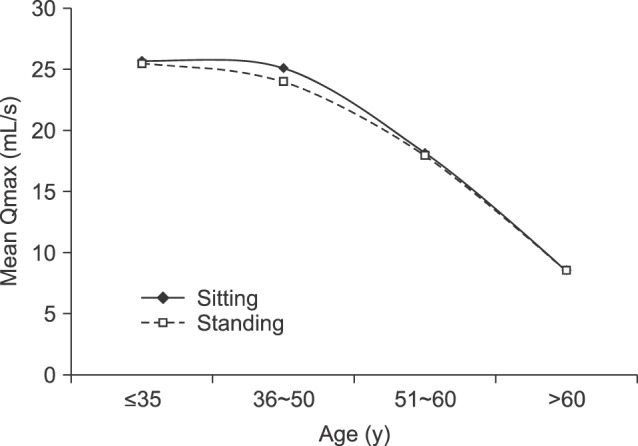
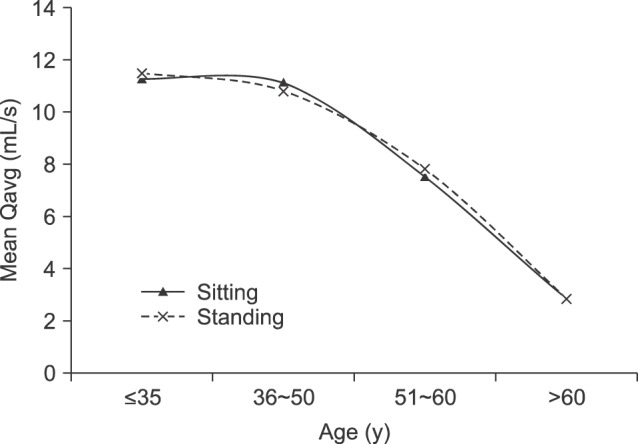
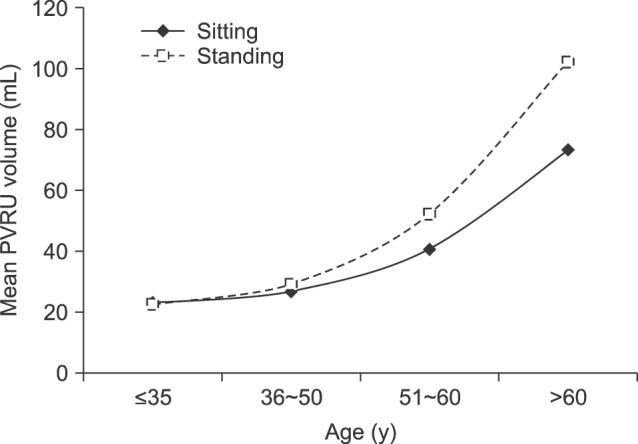
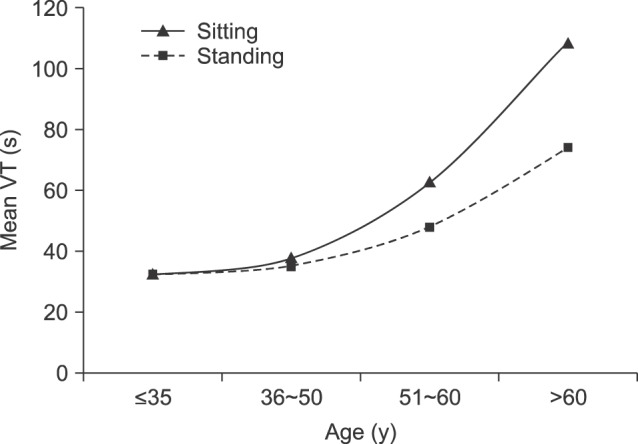
We conducted a prospective study from 2013 to 2015 and included men between 18 and 77 years old who were either healthy volunteers with an International Prostate Symptom Score (IPSS) ≤7 or men with benign prostate enlargement that were on alpha-blocker medication and had an IPSS <10. Participants underwent uroflowmetry and post-void residual urine (PVRU) measurements twice, once in a sitting position and once in a standing position. The participants were divided into 4 groups based on age (35 years or younger, 36 to 50 years, 51 to 60 years, and older than 60 years).
RESULTS
A total of 740 men with a mean age of 40.35 years were evaluated. There was no significant difference in uroflowmetry parameters until the age of 50 years between the voiding positions. However, in those older than 50 years, PVRU volume was significantly lower in the sitting position than the standing position, whereas voiding time was significantly higher in the sitting position than the standing position. Other uroflowmetry parameters, including maximal and average urine flow rates, were non-significant.
CONCLUSIONS
The voiding position plays an important role in the uroflowmetry parameters of elderly men. Voiding in the sitting position was found to be optimal for elderly men, whereas the role of the voiding position in healthy young men could not be determined. More research is needed to further study this issue.
MeSH Terms
Figure
Reference
-
1. Eryildirim B, Tarhan F, Kuyumcuoğlu U, Erbay E, Pembegül N. Position-related changes in uroflowmetric parameters in healthy young men. Neurourol Urodyn. 2006; 25:249–251. PMID: 16496389.2. Yamanishi T, Yasuda K, Sakakibara R, Hattori T, Minamide M, Yuki T, et al. Variation in urinary flow according to voiding position in normal males. Neurourol Urodyn. 1999; 18:553–557. PMID: 10529703.
Article3. Riehmann M, Bayer WH, Drinka PJ, Schultz S, Krause P, Rhodes PR, et al. Position-related changes in voiding dynamics in men. Urology. 1998; 52:625–630. PMID: 9763082.
Article4. Gupta NP, Kumar A, Kumar R. Does position affect uroflowmetry parameters in women? Urol Int. 2008; 80:37–40. PMID: 18204231.
Article5. El-Bahnasawy MS, Fadl FA. Uroflowmetric differences between standing and sitting positions for men used to void in the sitting position. Urology. 2008; 71:465–468. PMID: 18342188.
Article6. Moore KH, Richmond DH, Sutherst JR, Imrie AH, Hutton JL. Crouching over the toilet seat: prevalence among British gynaecological outpatients and its effect upon micturition. Br J Obstet Gynaecol. 1991; 98:569–572. PMID: 1873247.
Article7. Amjadi M, Madaen SK, Pour-Moazen H. Uroflowmetry findings in patients with bladder outlet obstruction symptoms in standing and crouching positions. Urol J. 2006; 3:49–53. PMID: 17590853.8. Aghamir SM, Mohseni M, Arasteh S. The effect of voiding position on uroflowmetry findings of healthy men and patients with benign prostatic hyperplasia. Urol J. 2005; 2:216–221. PMID: 17602433.9. Choudhury S, Agarwal MM, Mandal AK, Mavuduru R, Mete UK, Kumar S, et al. Which voiding position is associated with lowest flow rates in healthy adult men? role of natural voiding position. Neurourol Urodyn. 2010; 29:413–417. PMID: 19634168.
Article10. Unsal A, Cimentepe E. Voiding position does not affect uroflowmetric parameters and post-void residual urine volume in healthy volunteers. Scand J Urol Nephrol. 2004; 38:469–471. PMID: 15841779.11. Unsal A, Cimentepe E. Effect of voiding position on uroflowmetric parameters and post-void residual urine volume in patients with benign prostatic hyperplasia. Scand J Urol Nephrol. 2004; 38:240–242. PMID: 15204379.12. Yazici CM, Turker P, Dogan C. Effect of voiding position on uroflowmetric parameters in healthy and obstructed male patients. Urol J. 2014; 10:1106–1113. PMID: 24469658.13. de Jong Y, Pinckaers JH, ten Brinck RM, Lycklama à, Dekkers OM. Urinating standing versus sitting: position is of influence in men with prostate enlargement. A systematic review and meta-analysis. PLoS One. 2014; 9:e101320. PMID: 25051345.
Article14. Nordling J. The aging bladder: a significant but underestimated role in the development of lower urinary tract symptoms. Exp Gerontol. 2002; 37:991–999. PMID: 12213549.15. Moyad MA, Lowe FC. Educating patients about lifestyle modifications for prostate health. Am J Med. 2008; 121:S34–S42.
Article16. Norg RJC, Portegijs PJM, van Schayck CP, van de Beek C, Knottnerus JA. Please be seated? Position-related differences in voiding in men with lower urinary tract symptoms. In : Norg RJC, editor. A general practitioner's approach to lower urinary tract symptoms [Internet]. Maastricht: Maastricht University;2008. p. 55–69. cited 2008 Jan 1. Available from: http://arno.unimaas.nl/show.cgi?fid=21523.17. Roehrborn CG, Kaplan SA, Lee MW, Slawin KM, McVary KT, Kusek JW, et al. Baseline post void residual urine volume as a predictor of urinary outcomes in men with BPH in the MTOPS study. J Urol. 2005; 173:443. abstract 1638.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Urofolwmetry in the Female Voiding Difficulties
- A Novel Mobile Acoustic Uroflowmetry: Comparison With Contemporary Uroflowmetry
- Prostatodynia: Characteristics of Uroflowmetries
- The effect of posture and repetition on urodynamic parameters: A prospective randomized study
- Usefulness of Voiding Symptom Score and Uroflowmetry as the Screening Methods for Patients with Prostatitis Syndrome