J Korean Ophthalmol Soc.
2017 Aug;58(8):981-985. 10.3341/jkos.2017.58.8.981.
Two Cases of Corneal Neovascularization Improved by Electrocauterization and Subconjunctival Bevacizumab Injection
- Affiliations
-
- 1Department of Ophthalmology, Dankook University College of Medicine, Cheonan, Korea. perfectcure@hanmail.net
- KMID: 2388188
- DOI: http://doi.org/10.3341/jkos.2017.58.8.981
Abstract
- PURPOSE
To report an experience of improving symptoms through treatment with electrocauterization and subconjunctival bevacizumab injection in two patients with keratitis accompanied by corneal neovascularization and opacity.
CASE SUMMARY
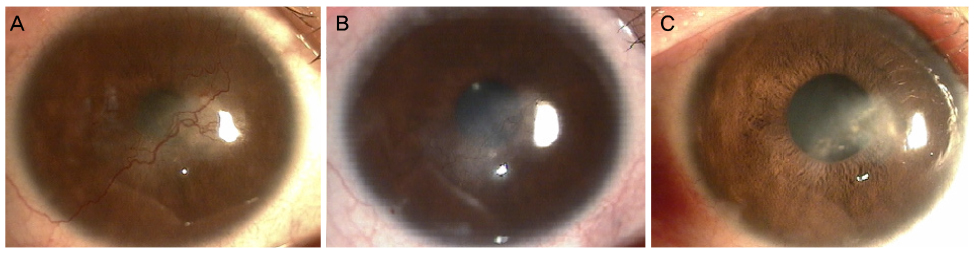
(Case 1) A 20-year-old woman visited our institution complaining of binocular blurred vision and congestion for the previous 3 years. Her best corrected visual acuity (BCVA) was 0.07 in the right eye and 0.4 in the left eye (Han Chun-suk visual acuity chart, decimal). The diagnosis was bilateral rosacea keratitis. Antibiotics, steroid eye drops and oral antibiotics were administered, but no improvement was observed. Electrocauterization was performed at the origin of the neovascularization of the cornea and bevacizumab was injected at the peripheral subconjunctiva in the right eye. Thereafter the corneal neovascularization did not recur, corneal opacity was reduced, and BCVA improved to 0.5. (Case 2) A 19-year-old woman visited complaining of left eye congestion for the previous 3 years. Her BCVA was 1.0 in the right eye and 0.08 in the left eye.The diagnosis was phlyctenular keratitis of the left eye. Antibiotics, steroid eye drops and oral antibiotics were administered, but no improvement was observed. Therefore, electrocauterization and subconjunctival bevacizumab injection were performed in the cornea of the left eye, after which corneal neovascularization and opacity decreased.
CONCLUSIONS
In these cases, we report improvement of symptoms after treatment with electrocauterization and subconjunctival bevacizumab injection after failed treatment of palpebral sanitation, antibiotic and steroid.
MeSH Terms
-
Anti-Bacterial Agents
Bevacizumab*
Cornea
Corneal Neovascularization*
Corneal Opacity
Diagnosis
Electrocoagulation
Estrogens, Conjugated (USP)
Female
Humans
Keratitis
Ophthalmic Solutions
Rosacea
Sanitation
Telescopes
Visual Acuity
Young Adult
Anti-Bacterial Agents
Bevacizumab
Estrogens, Conjugated (USP)
Ophthalmic Solutions
Figure
Reference
-
1. Isner JM, Asahara T. Angiogenesis and vasculogenesis as therapeutic strategies for postnatal neovascularization. J Clin Invest. 1999; 103:1231–1236.2. Folkman J. Angiogenesis in cancer, vascular, rheumatoid and other disease. Nat Med. 1995; 1:27–31.3. Burger PC, Chandler DB, Klintworth GK. Experimental corneal neovascularization: biomicroscopic, angiographic, and morphologic correlation. Cornea. 1985-1986; 4:35–41.4. Cursiefen C, Küchle M, Naumann GO. Angiogenesis in corneal diseases: histopathologic evaluation of 254 human corneal buttons with neovascularization. Cornea. 1998; 17:611–613.5. Chang JH, Gabison EE, Kato T, Azar DT. Corneal neovascularization. Curr Opin Ophthalmol. 2001; 12:242–249.6. Borrie P. Rosacea with special reference to its ocular manifestations. Br J Dermatol. 1953; 65:458–463.7. Starr PA, Macdonald A. Oculocutaneous aspects of rosacea. Proc R Soc Med. 1969; 62:9–11.8. Jung JY, Kim JS. Comparison of optic disc appearance in anterior ischemic optic neuropathy and optic neuritis. J Korean Ophthalmol Soc. 2003; 44:157–161.9. Abu el Asrar AM, Geboes K, Maudgal PC, et al. Immunocytological study of phlyctenular eye disease. Int Ophthalmol. 1987; 10:33–39.10. Culbertson WW, Huang AJ, Mandelbaum SH, et al. Effective treatment of phlyctenular keratoconjunctivitis with oral tetracycline. Ophthalmology. 1993; 100:1358–1366.11. Chen J, Liu W, Liu Z, et al. Expression of vascular endothelial growth factor and its receptors (flt-1) in morbid human corneas and investigation of its clinic importance. Yan Ke Xue Bao. 2002; 18:203–207.12. Bahar I, Kaiserman I, McAllum P, et al. Subconjunctival bevacizumab injection for corneal neovascularization. Cornea. 2008; 27:142–147.13. Gohto Y, Obana A, Kaneda K, Miki T. Photodynamic effect of a new photosensitizer ATX-S10 on corneal neovascularization. Exp Eye Res. 1998; 67:313–322.14. Gerten G. Bevacizumab (avastin) and argon laser to treat neovascularization in corneal transplant surgery. Cornea. 2008; 27:1195–1199.15. Pillai CT, Dua HS, Hossain P. Fine needle diathermy occlusion of corneal vessels. Invest Ophthalmol Vis Sci. 2000; 41:2148–2153.16. Bock F, Köenig Y, Dietrich T, et al. Inhibition of angiogenesis in the anterior chamber of the eye. Ophthalmologe. 2007; 104:336–344.17. Cursiefen C, Chen L, Saint-Geniez M, et al. Nonvascular VEGF receptor 3 expression by corneal epithelium maintains avascularity and vision. Proc Natl Acad Sci U S A. 2006; 103:11405–11410.18. Phillips K, Arffa R, Cintron C, et al. Effects of prednisolone and medroxyprogesterone on corneal wound healing, ulceration, and neovascularization. Arch Ophthalmol. 1983; 101:640–643.19. Baer JC, Foster CS. Corneal laser photocoagulation for treatment of neovascularization. Efficacy of 577 nm yellow dye laser. Ophthalmology. 1992; 99:173–179.20. Primbs GB, Casey R, Wamser K, et al. Photodynamic therapy for corneal neovascularization. Ophthalmic Surg Lasers. 1998; 29:832–838.21. Cursiefen C, Chen L, Borges LP, et al. VEGF-A stimulates lymphangiogenesis and hemangiogenesis in inflammatory neovascularization via macrophage recruitment. J Clin Invest. 2004; 113:1040–1050.22. Amano S, Rohan R, Kuroki M, et al. Requirement for vascular endothelial growth factor in wound- and inflammation-related corneal neovascularization. Invest Ophthalmol Vis Sci. 1998; 39:18–22.23. Zheng M, Deshpande S, Lee S, et al. Contribution of vascular endothelial growth factor in the neovascularization process during the pathogenesis of herpetic stromal keratitis. J Virol. 2001; 75:9828–9835.24. Chu HS, Hu FR, Yang CM, et al. Subconjunctival injection of bevacizumab in the treatment of corneal neovascularization associated with lipid deposition. Cornea. 2011; 30:60–66.25. Zaki AA, Farid SF. Subconjunctival bevacizumab for corneal neovascularization. Acta Ophthalmol. 2010; 88:868–871.26. Mimura T, Amano S, Usui T, et al. Expression of vascular endothelial growth factor C and vascular endothelial growth factor receptor 3 in corneal lymphangiogenesis. Exp Eye Res. 2001; 72:71–78.27. Singh D, Singh K. Transciliary filtration using the fugo blade TM. Ann Ophthalmol. 2002; 34:183–187.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bi-weekly Subconjunctival Injection of Bevacizumab for Corneal Neovascularization after Burn Injury
- Ranibizumab Injection for Corneal Neovascularization Refractory to Bevacizumab Treatment
- Regression of Iris Neovascularization after Subconjunctival Injection of Bevacizumab
- The Effects of a Subtenoncapsular Injection of Bevacizumab for Ocular Surface Disease With Corneal Neovascularization
- The Effect of Bevacizumab on Corneal Neovascularization in Rabbits