Investig Clin Urol.
2017 Sep;58(5):359-364. 10.4111/icu.2017.58.5.359.
Can men with prostates sized 80 mL or larger be managed conservatively?
- Affiliations
-
- 1Department of Urology, Singapore General Hospital, Singapore. foo.keong.tatt@sgh.com.sg
- KMID: 2388053
- DOI: http://doi.org/10.4111/icu.2017.58.5.359
Abstract
- PURPOSE
To analyze the long-term clinical outcomes of men with large prostate sizes of 80 mL and greater who were managed conservatively.
MATERIALS AND METHODS
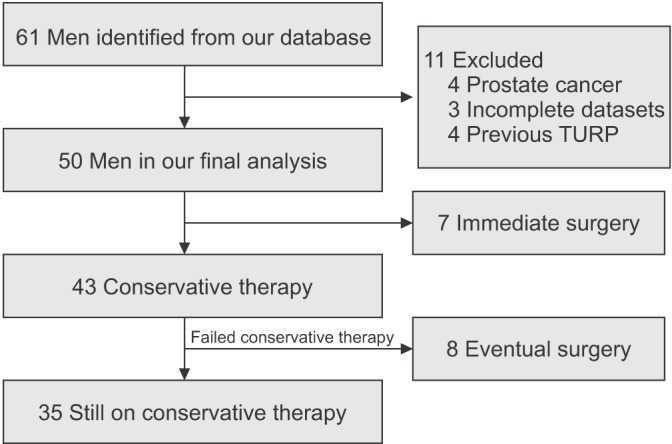
We retrospectively analyzed men with prostate sizes of 80 mL and greater from our electronic hospital database. Clinical parameters such as age, International Prostate Symptom Score (IPSS), quality of life (QoL) scoring, serum prostate-specific antigen (PSA), uroflowmetry variables, and transabdominal ultrasound findings were evaluated. These parameters were compared at entry to our study and at the patient's latest follow-up visit.
RESULTS
For the 50 men included in our analysis, mean age was 68 years, median PSA was 9.9 ng/mL, and median prostate volume was 94 mL. Seven men underwent upfront prostate surgery, whereas the other 43 were managed conservatively, predominantly with pharmacotherapy (98%). Only serum PSA, QoL scores, and postvoid residual urine demonstrated a significant reduction at the end of a median follow-up period of 62 months. Fourteen men (33%) were considered to have progressed clinically, with 8 experiencing retention of urine and 6 having symptomatic deterioration. Of the 35 men who were still receiving conservative treatment at the end of the follow-up period, 24 men (69%) had a peak flow rate of 10 mL/s or greater, a QoL score of 3 or less, and mild to moderate (IPSS, 0-19) symptoms.
CONCLUSIONS
Although the incidence of clinical progression in men with prostate sizes of 80 mL and greater is high, there is still a role for conservative management with pharmacotherapy.
MeSH Terms
Figure
Reference
-
1. Arrighi HM, Metter EJ, Guess HA, Fozzard JL. Natural history of benign prostatic hyperplasia and risk of prostatectomy. The Baltimore Longitudinal Study of Aging. Urology. 1991; 38(1 Suppl):4–8. PMID: 1714657.2. Rhodes T, Girman CJ, Jacobsen SJ, Roberts RO, Guess HA, Lieber MM. Longitudinal prostate growth rates during 5 years in randomly selected community men 40 to 79 years old. J Urol. 1999; 161:1174–1179. PMID: 10081864.
Article3. Steele GS, Sullivan MP, Sleep DJ, Yalla SV. Combination of symptom score, flow rate and prostate volume for predicting bladder outflow obstruction in men with lower urinary tract symptoms. J Urol. 2000; 164:344–348. PMID: 10893581.
Article4. Yalla SV, Sullivan MP, Lecamwasam HS, DuBeau CE, Vickers MA, Cravalho EG. Correlation of American Urological Association symptom index with obstructive and nonobstructive prostatism. J Urol. 1995; 153(3 Pt 1):674–679. PMID: 7532231.
Article5. Kuntz RM, Lehrich K, Ahyai SA. Holmium laser enucleation of the prostate versus open prostatectomy for prostates greater than 100 grams: 5-year follow-up results of a randomised clinical trial. Eur Urol. 2008; 53:160–166. PMID: 17869409.
Article6. Naspro R, Suardi N, Salonia A, Scattoni V, Guazzoni G, Colombo R, et al. Holmium laser enucleation of the prostate versus open prostatectomy for prostates >70 g: 24-month follow-up. Eur Urol. 2006; 50:563–568. PMID: 16713070.7. Zhang Y, Du CJ, Xu G, Chen JM, Jing X. Transurethral holmium laser enucleation for prostate adenoma greater than 100 g. Zhonghua Nan Ke Xue. 2007; 13:1091–1093. PMID: 18284057.8. Yuen JS, Ngiap JT, Cheng CW, Foo KT. Effects of bladder volume on transabdominal ultrasound measurements of intravesical prostatic protrusion and volume. Int J Urol. 2002; 9:225–229. PMID: 12010318.
Article9. Wang D, Foo KT. Staging of benign prostate hyperplasia is helpful in patients with lower urinary tract symptoms suggestive of benign prostate hyperplasia. Ann Acad Med Singapore. 2010; 39:798–802. PMID: 21063641.10. Lieber MM, Rhodes T, Jacobson DJ, McGree ME, Girman CJ, Jacobsen SJ, et al. Natural history of benign prostatic enlargement: long-term longitudinal population-based study of prostate volume doubling times. BJU Int. 2010; 105:214–219. PMID: 19594737.
Article11. Rhodes T, Girman CJ, Jacobsen DJ, Roberts RO, Lerber MM, Jacobsen SJ. Longitudinal prostate volume in a community-based sample: 7 year followup in the Olmsted County Study of Urinary Symptoms and Health Status among Men [abstract]. J Urol. 2000; 163(Suppl 4):249. Abstract No. 1105. PMID: 10604369.12. Marberger MJ, Andersen JT, Nickel JC, Malice MP, Gabriel M, Pappas F, et al. Prostate volume and serum prostate-specific antigen as predictors of acute urinary retention. Combined experience from three large multinational placebo-controlled trials. Eur Urol. 2000; 38:563–568. PMID: 11096237.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Prostate Size on Cancer Detection Rate of Traditional Sextant Prostate Biopsy
- Midline Cysts in the Prostate: Incidence in Healthy Men on Transrectal Ultrasonography (TRUS)
- The Role of Digital Rectal Examination Prostate Volume Category in the Early Detection of Prostate Cancer: Its Correlation with the Magnetic Resonance Imaging Prostate Volume
- Dichotomous Estimation of Prostate Volume: A Diagnostic Study of the Accuracy of the Digital Rectal Examination
- Normal PSA Values according to Age in Healthy Men without Prostatic Disease