J Korean Neurosurg Soc.
2017 Jul;60(4):441-447. 10.3340/jkns.2015.0708.014.
Inter- and Intra-Observer Variability of the Volume of Cervical Ossification of the Posterior Longitudinal Ligament Using Medical Image Processing Software
- Affiliations
-
- 1Department of Neurosurgery, Yonsei University College of Medicine, Seoul, Korea.
- 2Spine and Joint Research Institute, Guro Cham Teun Teun Hospital, Seoul, Korea.
- 3Department of Neurosurgery, Kangbuk Samsung Hospital, Sungkyunkwan University College of Medicine, Seoul, Korea. nsdrshin@gmail.com
- KMID: 2387882
- DOI: http://doi.org/10.3340/jkns.2015.0708.014
Abstract
OBJECTIVE
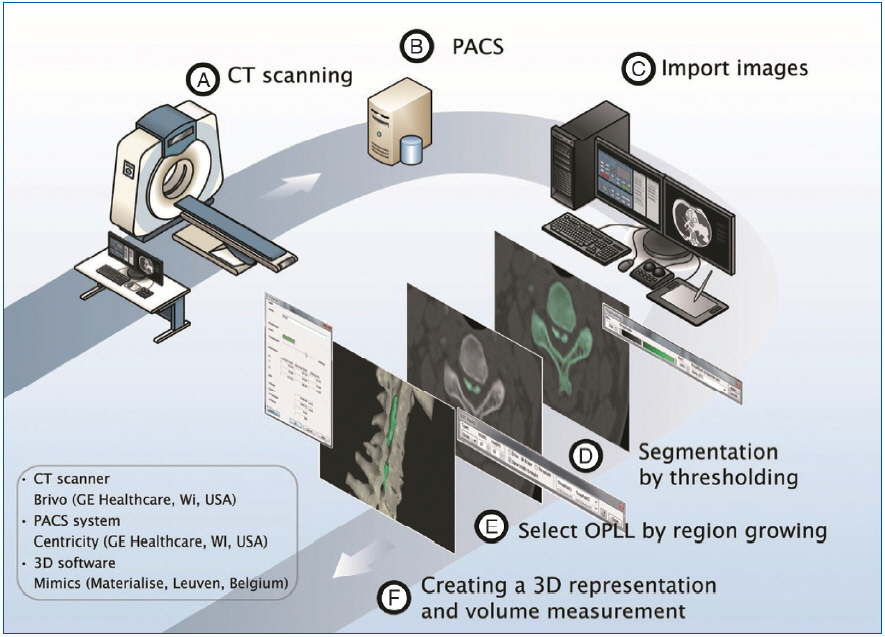
Computed tomography (CT)-based method of three dimensional (3D) analysis (MIMICS®, Materialise, Leuven, Belgium) is reported as very useful software for evaluation of OPLL, but its reliability and reproducibility are obscure. This study was conducted to evaluate the accuracy of MIMICS® system, and inter- and intra-observer reliability in the measurement of OPLL.
METHODS
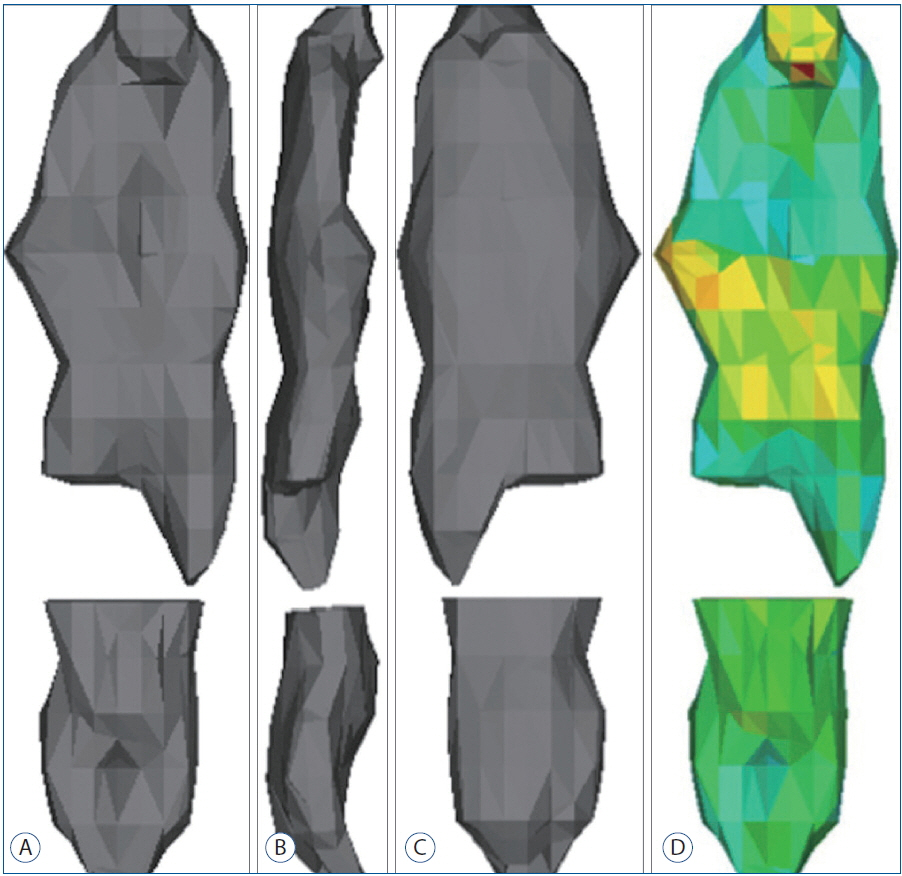
Three neurosurgeons independently analyzed the randomly selected 10 OPLL cases with medical image processing software (MIMICS®) which create 3D model with Digital Imaging and Communication in Medicine (DICOM) data from CT images after brief explanation was given to examiners before the image construction steps. To assess the reliability of inter- and intra-examiner intraclass correlation coefficient (ICC), 3 examiners measured 4 parameters (volume, length, width, and length) in 10 cases 2 times with 1-week interval.
RESULTS
The inter-examiner ICCs among 3 examiners were 0.996 (95% confidence interval [CI], 0.987-0.999) for volume measurement, 0.973 (95% CI, 0.907-0.978) for thickness, 0.969 (95% CI, 0.895-0.993) for width, and 0.995 (95% CI, 0.983-0.999) for length. The intra-examiner ICCs were 0.994 (range, 0.991-0.996) for volume, 0.996 (range, 0.944-0.998) for length, 0.930 (range, 0.873-0.947) for width, and 0.987 (range, 0.985-0.995) for length.
CONCLUSION
The medical image processing software (MIMICS®) provided detailed quantification OPLL volume with minimal error of inter- and intra-observer reliability in the measurement of OPLL.
Figure
Reference
-
References
1. Bakay L, Cares HL, Smith RJ. Ossification in the region of the posterior longitudinal ligament as a cause of cervical myelopathy. J Neurol Neurosurg Psychiatry. 33:263–268. 1970.
Article2. Chang H, Kong CG, Won HY, Kim JH, Park JB. Inter- and intra-observer variability of a cervical OPLL classification using reconstructed CT images. Clin Orthop Surg. 2:8–12. 2010.
Article3. Chiba K, Kato Y, Tsuzuki N, Nagata K, Toyama Y, Iwasaki M, et al. Computer-assisted measurement of the size of ossification in patients with ossification of the posterior longitudinal ligament in the cervical spine. J Orthop Sci. 10:451–456. 2005.
Article4. Chiba K, Ogawa Y, Ishii K, Takaishi H, Nakamura M, Maruiwa H, et al. Long-term results of expansive open-door laminoplasty for cervical myelopathy--average 14-year follow-up study. Spine (Phila Pa 1976). 31:2998–3005. 2006.
Article5. Chiba K, Yamamoto I, Hirabayashi H, Iwasaki M, Goto H, Yonenobu K, et al. Multicenter study investigating the postoperative progression of ossification of the posterior longitudinal ligament in the cervical spine: a new computer-assisted measurement. J Neurosurg Spine. 3:17–23. 2005.
Article6. Choi JH, Shin JJ, Kim TH, Shin HS, Hwang YS, Park SK. Does intra-medullary signal intensity on MRI affect the surgical outcomes of patients with ossification of posterior longitudinal ligament? J Korean Neurosurg Soc. 56:121–129. 2014.
Article7. Fujimori T, Iwasaki M, Nagamoto Y, Ishii T, Sakaura H, Kashii M, et al. Three-dimensional measurement of growth of ossification of the posterior longitudinal ligament. J Neurosurg Spine. 16:289–295. 2012.
Article8. Han IH, Suh SH, Kuh SU, Chin DK, Kim KS. Types and prevalence of coexisting spine lesions on whole spine sagittal MR images in surgical degenerative spinal diseases. Yonsei Med J. 51:414–420. 2010.
Article9. Hori T, Kawaguchi Y, Kimura T. How does the ossification area of the posterior longitudinal ligament progress after cervical laminoplasty? Spine (Phila Pa 1976). 31:2807–2812. 2006.
Article10. Iwasaki M, Okuda S, Miyauchi A, Sakaura H, Mukai Y, Yonenobu K, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: Part 2: Advantages of anterior decompression and fusion over laminoplasty. Spine (Phila Pa 1976). 32:654–660. 2007.
Article11. Izumi T, Hirano T, Watanabe K, Sano A, Ito T, Endo N. Three-dimensional evaluation of volume change in ossification of the posterior longitudinal ligament of the cervical spine using computed tomography. Eur Spine J. 22:2569–2574. 2013.
Article12. Jayakumar PN, Kolluri VR, Vasudev MK, Srikanth SG. Ossification of the posterior longitudinal ligament of the cervical spine in Asian Indians--a multiracial comparison. Clin Neurol Neurosurg. 98:142–148. 1996.
Article13. Kawaguchi Y, Kanamori M, Ishihara H, Nakamura H, Sugimori K, Tsuji H, et al. Progression of ossification of the posterior longitudinal ligament following en bloc cervical laminoplasty. J Bone Joint Surg Am. 83-A:1798–1802. 2001.
Article14. Lee T, Chacha PB, Khoo J. Ossification of posterior longitudinal ligament of the cervical spine in non-Japanese Asians. Surg Neurol. 35:40–44. 1991.
Article15. Matsunaga S, Kukita M, Hayashi K, Shinkura R, Koriyama C, Sakou T, et al. Pathogenesis of myelopathy in patients with ossification of the posterior longitudinal ligament. J Neurosurg. 96(2 Suppl):168–172. 2002.
Article16. Matsunaga S, Nakamura K, Seichi A, Yokoyama T, Toh S, Ichimura S, et al. Radiographic predictors for the development of myelopathy in patients with ossification of the posterior longitudinal ligament: a multicenter cohort study. Spine (Phila Pa 1976). 33:2648–2650. 2008.
Article17. Morio Y, Nagashima H, Teshima R, Nawata K. Radiological pathogenesis of cervical myelopathy in 60 consecutive patients with cervical ossification of the posterior longitudinal ligament. Spinal Cord. 37:853–857. 1999.
Article18. Nagata K, Sato K. Diagnostic imaging of cervical ossification of the posterior longitudinal ligament. Yonenobu K, Nakamura K, Toyama Y, editors. OPLL: Ossification of the Posterior Longitudinal Ligament. ed 2. Tokyo: Springer;2006. p. 127–143.
Article19. Ogata N, Kawaguchi H. Ossitication of the posterior longitudinal ligament of spine (OPLL). Clin Calcium. 14:42–48. 2004.20. Seichi A. Updates on ossification of posterior longitudinal ligament. Image diagnosis of ossification of posterior longitudinal ligament and associated diseases. Clin Calcium. 19:1426–1434. 2009.21. Takatsu T, Ishida Y, Suzuki K, Inoue H. Radiological study of cervical ossification of the posterior longitudinal ligament. J Spinal Disord. 12:271–273. 1999.
Article22. Tsuyama N. Ossification of the posterior longitudinal ligament of the spine. Clin Orthop Relat Res. (184):71–84. 1984.
Article23. Yonenobu K, Tsuzuki N, Nagata K, Toyama Y, Kato Y, Iwasaki M. Computer-assisted measurement of ossified lesion in ossification of the posterior longitudinal ligament of the cervical spine. Bone. 16:283–286. 2002.24. Zhong ZM, Chen JT. Phenotypic characterization of ligamentum flavum cells from patients with ossification of ligamentum flavum. Yonsei Med J. 50:375–379. 2009.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ossification of the Posterior Longitudinal Ligament: 2 cases report
- Inter- and Intra-observer Variability of a Cervical OPLL Classification Using Reconstructed CT Images
- Dysphagia Caused by Ossification of the Cervical Anterior Longitudinal Ligament
- A Case of Diffuse Idiopathic Skeletal Hyperostosis ( DISH ) Associated with Ossification of the Posterior Longuitudinal Ligament ( OPLL
- Does Ossification of the Posterior Longitudinal Ligament Progress after Fusion?