J Korean Acad Prosthodont.
2017 Jul;55(3):251-257. 10.4047/jkap.2017.55.3.251.
Influence of internal connection length on screw loosening in internal connection implants
- Affiliations
-
- 1Department of Prosthodontics, Yonsei University College of Denistry, Seoul, Republic of Korea. jaehoon115@yuhs.ac, hsm5@yuhs.ac
- 2Oral Science Research Center, BK21 PLUS Project, Yonsei University College of Dentistry, Seoul, Republic of Korea.
- 3Department of Periodontology, Dental Research Institute, Seoul National University School of Dentistry, Seoul, Republic of Korea.
- 4Department of Conservative Dentistry, School of Dentistry, Pusan National University, Yangsan, Republic of Korea.
- 5Department of Prosthodontics, Gangnam Severance Dental Hospital, College of Dentistry, Yonsei University, Seoul, Republic of Korea.
- KMID: 2387196
- DOI: http://doi.org/10.4047/jkap.2017.55.3.251
Abstract
- PURPOSE
The purpose of this study was to evaluate whether the internal abutment length affected screw stability in an internal connection implant.
MATERIALS AND METHODS
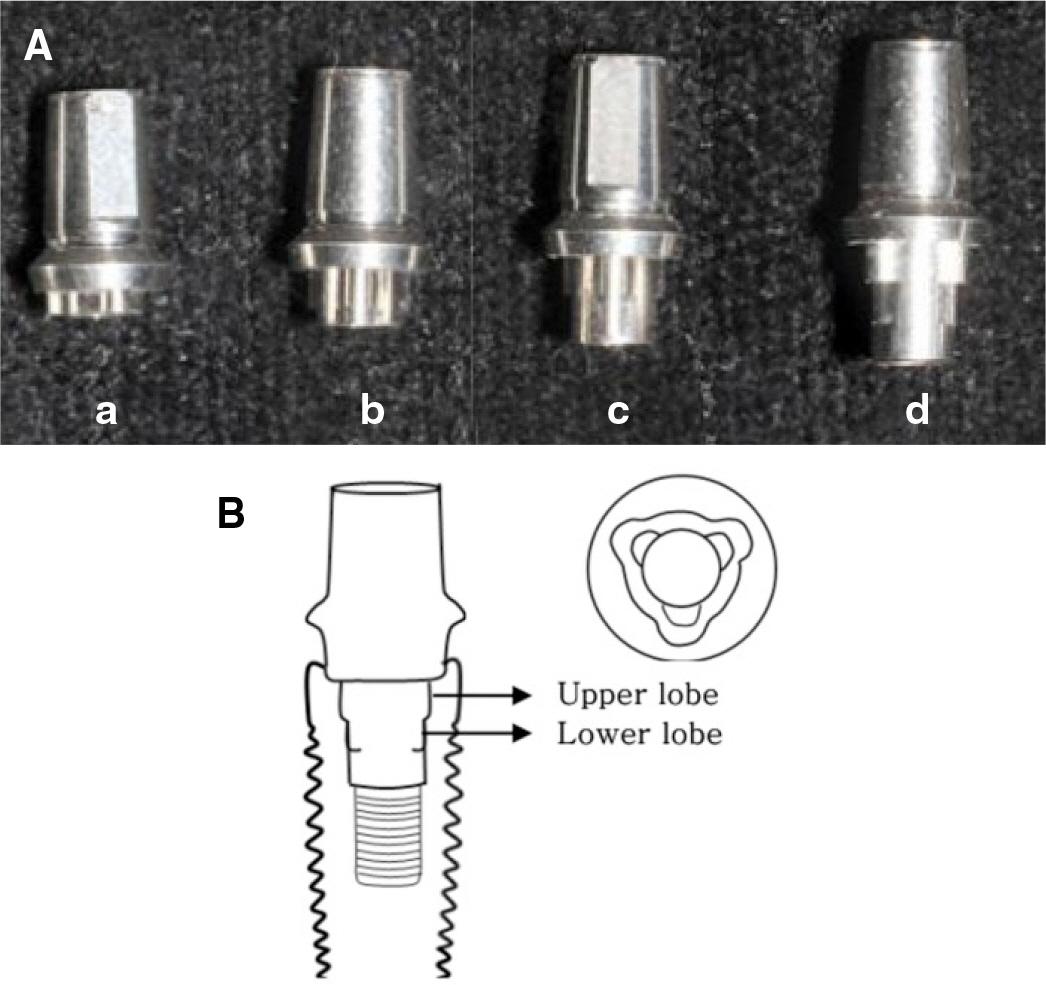
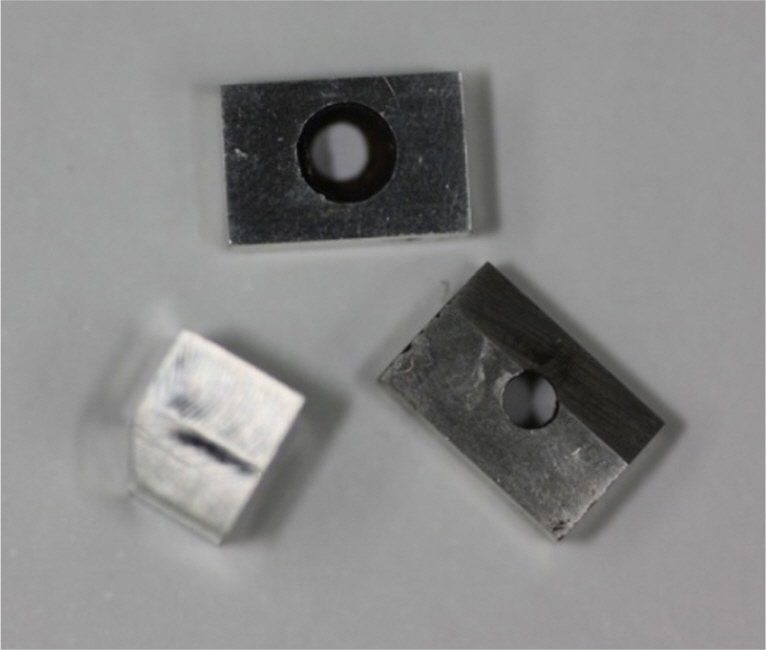
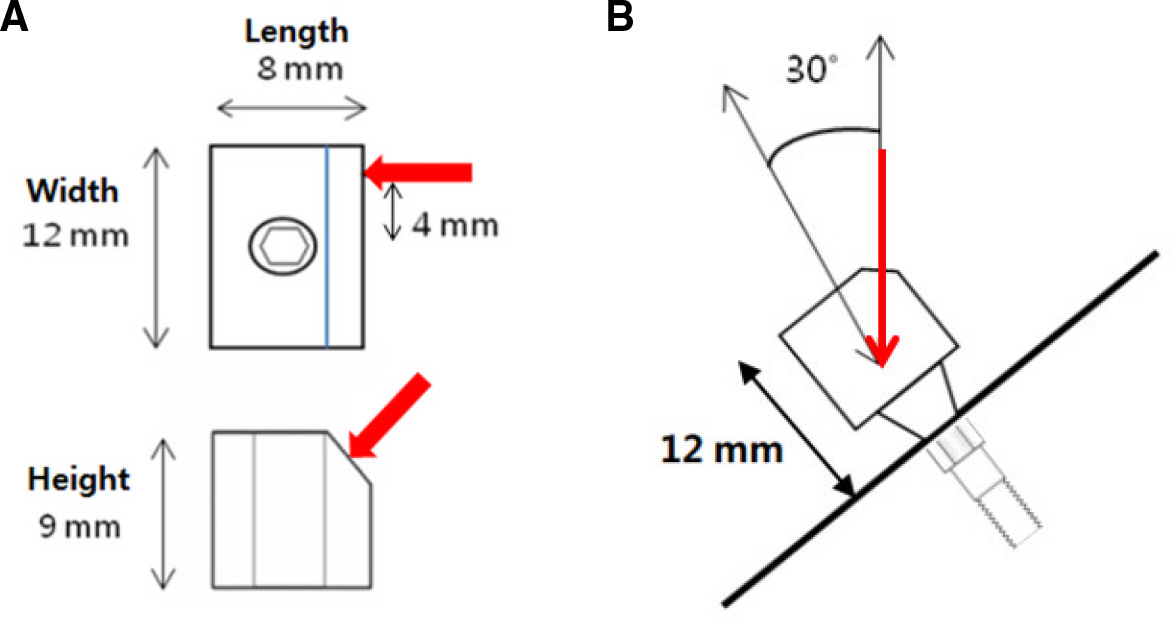
Twenty long internal connection implants (Replus system, 4.7 × 11.5 mm) were selected for this investigation. Abutments were assigned to four groups depending on the length of the internal connection (abutments with internal lengths of 1, 2, 3, and 4 mm, respectively). Each implant fixture specimen was embedded in resin medium and connected to an abutment with an abutment screw. A load of 100 N, applied at an angle of 30° to the long axis of the implant, was repeated for 1.0 × 10ⶠcycles. Reverse torque values (RTV) were recorded before and after loading, and the change in RTV was calculated. Data were analyzed with the Kruskal-Wallis test.
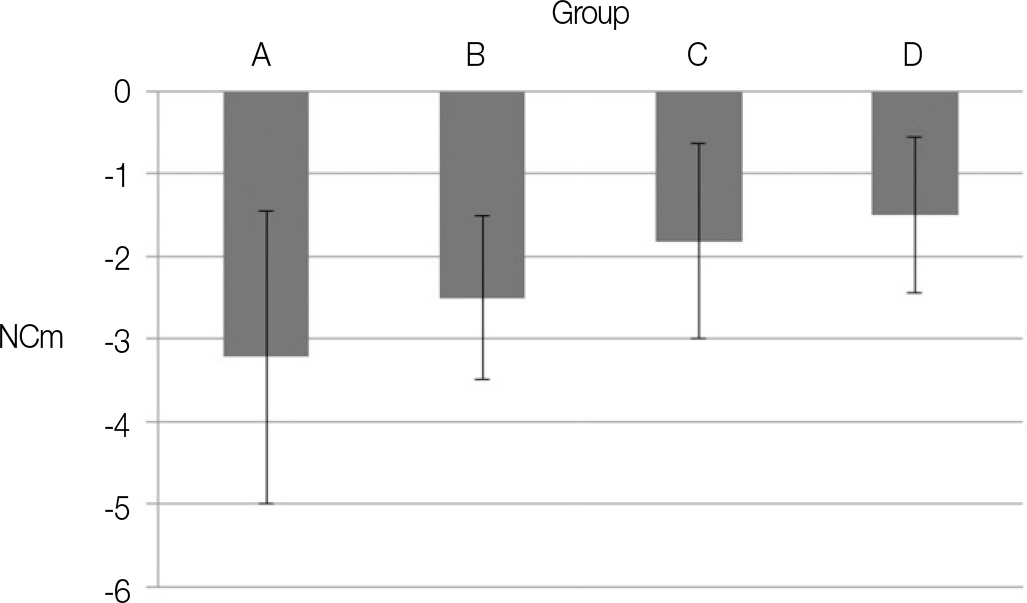
RESULTS
The change in RTV was not significantly different among the groups (P>.05). Screw loosening and fractures were not observed in any groups, and joint stability was maintained.
CONCLUSION
The internal length of the abutment may not significantly affect the degree of screw loosening.
Figure
Reference
-
1.Goodacre CJ., Kan JY., Rungcharassaeng K. Clinical complications of osseointegrated implants. J Prosthet Dent. 1999. 81:537–52.
Article2.Pjetursson BE., Brägger U., Lang NP., Zwahlen M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin Oral Implants Res. 2007. 18:97–113.
Article3.Jemt T., Laney WR., Harris D., Henry PJ., Krogh PH Jr., Polizzi G., Zarb GA., Herrmann I. Osseointegrated implants for single tooth replacement: a 1-year report from a multicenter prospective study. Int J Oral Maxillofac Implants. 1991. 6:29–36.4.Becker W., Becker BE. Replacement of maxillary and mandibular molars with single endosseous implant restorations: a retrospective study. J Prosthet Dent. 1995. 74:51–5.
Article5.McGlumphy EA., Mendel DA., Holloway JA. Implant screw mechanics. Dent Clin North Am. 1998. 42:71–89.6.Winkler S., Ring K., Ring JD., Boberick KG. Implant screw mechanics and the settling effect: overview. J Oral Implantol. 2003. 29:242–5.7.Sakaguchi RL., Borgersen SE. Nonlinear contact analysis of preload in dental implant screws. Int J Oral Maxillofac Implants. 1995. 10:295–302.8.Haack JE., Sakaguchi RL., Sun T., Coffey JP. Elongation and preload stress in dental implant abutment screws. Int J Oral Maxillofac Implants. 1995. 10:529–36.9.Siamos G., Winkler S., Boberick KG. Relationship between implant preload and screw loosening on implant-supported prostheses. J Oral Implantol. 2002. 28:67–73.10.Cavazos E., Bell FA. Preventing loosening of implant abutment screws. J Prosthet Dent. 1996. 75:566–9.
Article11.Aboyoussef H., Weiner S., Ehrenberg D. Effect of an antirotation resistance form on screw loosening for single implant-supported crowns. J Prosthet Dent. 2000. 83:450–5.
Article12.Binon PP. The spline implant: design, engineering, and evaluation. Int J Prosthodont. 1996. 9:419–33.13.Wiskott HW., Jaquet R., Scherrer SS., Belser UC. Resistance of internal-connection implant connectors under rotational fatigue loading. Int J Oral Maxillofac Implants. 2007. 22:249–57.14.Dixon DL., Breeding LC., Sadler JP., McKay ML. Comparison of screw loosening, rotation, and deflection among three implant designs. J Prosthet Dent. 1995. 74:270–8.
Article15.Ohrnell LO., Hirsch JM., Ericsson I., Brånemark PI. Single-tooth rehabilitation using osseointegration. A modified surgical and prosthodontic approach. Quintessence Int. 1988. 19:871–6.16.Cibirka RM., Nelson SK., Lang BR., Rueggeberg FA. Examination of the implant-abutment interface after fatigue testing. J Prosthet Dent. 2001. 85:268–75.
Article17.Bambini F., Lo Muzio L., Procaccini M. Retrospective analysis of the influence of abutment structure design on the success of implant unit. A 3-year controlled follow-up study. Clin Oral Implants Res. 2001. 12:319–24.18.McGlumphy EA., Robinson DM., Mendel DA. Implant superstructures: a comparison of ultimate failure force. Int J Oral Maxillofac Implants. 1992. 7:35–9.19.Steinebrunner L., Wolfart S., Ludwig K., Kern M. Implant-abutment interface design affects fatigue and fracture strength of implants. Clin Oral Implants Res. 2008. 19:1276–84.
Article20.Khraisat A., Hashimoto A., Nomura S., Miyakawa O. Effect of lateral cyclic loading on abutment screw loosening of an external hexagon implant system. J Prosthet Dent. 2004. 91:326–34.
Article21.Wiskott HW., Nicholls JI., Belser UC. Stress fatigue: basic principles and prosthodontic implications. Int J Prosthodont. 1995. 8:105–16.22.Tsuge T., Hagiwara Y. Influence of lateral-oblique cyclic loading on abutment screw loosening of internal and external hexagon implants. Dent Mater J. 2009. 28:373–81.
Article23.Gibbs CH., Mahan PE., Mauderli A., Lundeen HC., Walsh EK. Limits of human bite strength. J Prosthet Dent. 1986. 56:226–9.
Article24.Lang LA., Wang RF., May KB. The influence of abutment screw tightening on screw joint configuration. J Prosthet Dent. 2002. 87:74–9.
Article25.Piermatti J., Yousef H., Luke A., Mahevich R., Weiner S. An in vitro analysis of implant screw torque loss with external hex and internal connection implant systems. Implant Dent. 2006. 15:427–35.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The influence of implant fixture-abutment connection design on screw loosening
- Screw loosening and changes in removal torque relative to abutment screw length in a dental implant with external abutment connection after oblique cyclic loading
- Effect of casting procedure on screw loosening of UCLA abutment in two implant-abutment connection systems
- The assessment of abutment screw stability between the external and internal hexagonal joint under cyclic loading
- The effect of a titanium socket with a zirconia abutment on screw loosening after thermocycling in an internally connected implant: a preliminary study