J Korean Ophthalmol Soc.
2017 Jul;58(7):866-869. 10.3341/jkos.2017.58.7.866.
A Case of Penetrating Keratoplasty and Cataract Surgery for Improving Visual Acuity in Peter's Anomaly
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, College of Medicine, The Catholic University of Korea, Seoul, Korea. drna@catholic.ac.kr
- KMID: 2387163
- DOI: http://doi.org/10.3341/jkos.2017.58.7.866
Abstract
- PURPOSE
To report a case of penetrating keratoplasty and cataract surgery for improving visual acuity in an adult with Peters' anomaly.
CASE SUMMARY
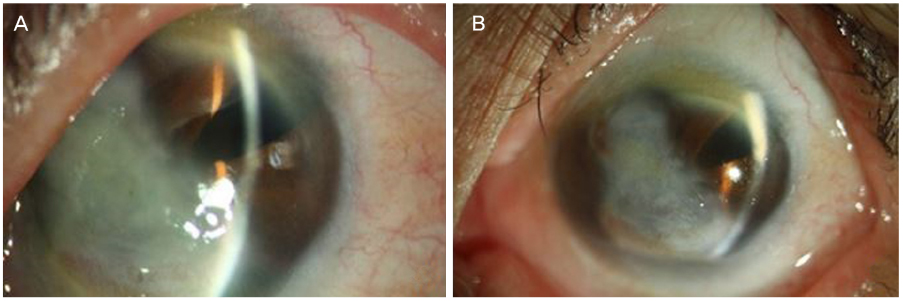
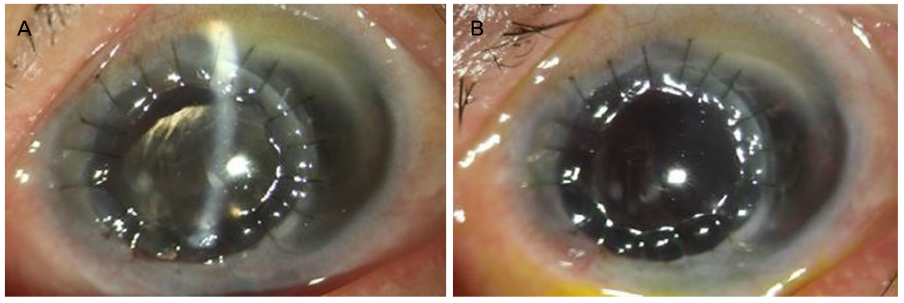
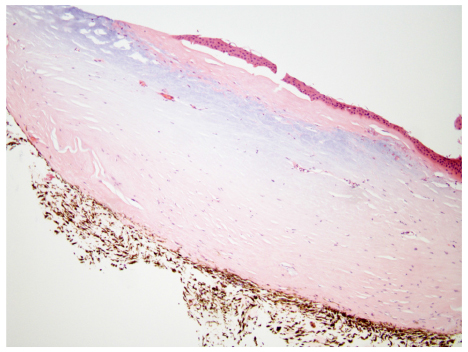
A 70-year-old female patient presented with decreased visual acuity for a few years. The patient had a history of Peters' anomaly in both eyes and evisceration surgery of the right eye 4 years prior to presentation. The patient's visual acuity was measured as finger count 20 cm at the time of visitation due to Peters' anomaly and brunescent cataract. In the slit lamp examination, irregular margin corneal opacity with anterior synechiae was observed in the center of the cornea, while the peripheral cornea was relatively normal. Penetrating keratoplasty and cataract surgery were performed, and visual acuity improved by 0.04 at 1 week, 0.04 at 1 month, and 0.16 at 4 months after surgery. Visual acuity was measured using a Snellen chart, and the intraocular pressure was maintained within the normal range of 17-20 mmHg.
CONCLUSIONS
If peripheral corneal invasion is not severe in adults with Peters' anomaly, penetrating keratoplasty and cataract surgery can be performed for the purpose of improving visual acuity.
Keyword
MeSH Terms
Figure
Reference
-
1. Shigeyasu C, Yamada M, Mizuno Y, et al. Clinical features of anterior segment dysgenesis associated with congenital corneal opacities. Cornea. 2012; 31:293–298.2. Kurilec JM, Zaidman GW. Incidence of Peters anomaly and congenital corneal opacities interfering with vision in the United States. Cornea. 2014; 33:848–850.3. Yoshikawa H, Sotozono C, Ikeda Y, et al. Long-term clinical course in eyes with Peters anomaly. Cornea. 2017; 36:448–451.4. Zaidman GW, Flanagan JK, Furey CC. Long-term visual prognosis in children after corneal transplant surgery for Peters anomaly type I. Am J Ophthalmol. 2007; 144:104–108.5. Kim YW, Choi HJ, Kim MK, et al. Clinical outcomes of penetrating keratoplasty in patients five years or younger. J Korean Ophthalmol Soc. 2013; 54:704–708.6. Rubin SE, Marcus CH. Glaucoma in childhood. Ophthalmol Clin North Am. 1996; 9:215–228.7. Stone DL, Kenyon KR, Green WR, Ryan SJ. Congenital central corneal leukoma (Peters' anomaly). Am J Ophthalmol. 1976; 81:173–193.8. Yang LL, Lambert SR, Drews-Botsch C, Stulting RD. Long-term visual outcome of penetrating keratoplasty in infants and children with Peters anomaly. J AAPOS. 2009; 13:175–180.9. Yang LL, Lambert SR, Lynn MJ, Stulting RD. Long-term results of corneal graft survival in infants and children with peters anomaly. Ophthalmology. 1999; 106:833–848.