J Korean Ophthalmol Soc.
2017 Jul;58(7):788-796. 10.3341/jkos.2017.58.7.788.
Correlation Analysis of Tear Film Lipid Layer Thickness and Ocular Surface Disease Index
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, The Catholic University of Korea, Seoul, Korea. Sara514@catholic.ac.kr
- 2Department of Ophthalmology, The Catholic University of Korea Yeouido St. Mary's Hospital, Seoul, Korea.
- KMID: 2387152
- DOI: http://doi.org/10.3341/jkos.2017.58.7.788
Abstract
- PURPOSE
To analyze the relationship between ocular surface disease index and tear film lipid layer thickness (LLT) using a LipiView II® (LipiView® Ocular Surface Interferometer, TearScience®, Morrisville, NC, USA) interferometer.
METHODS
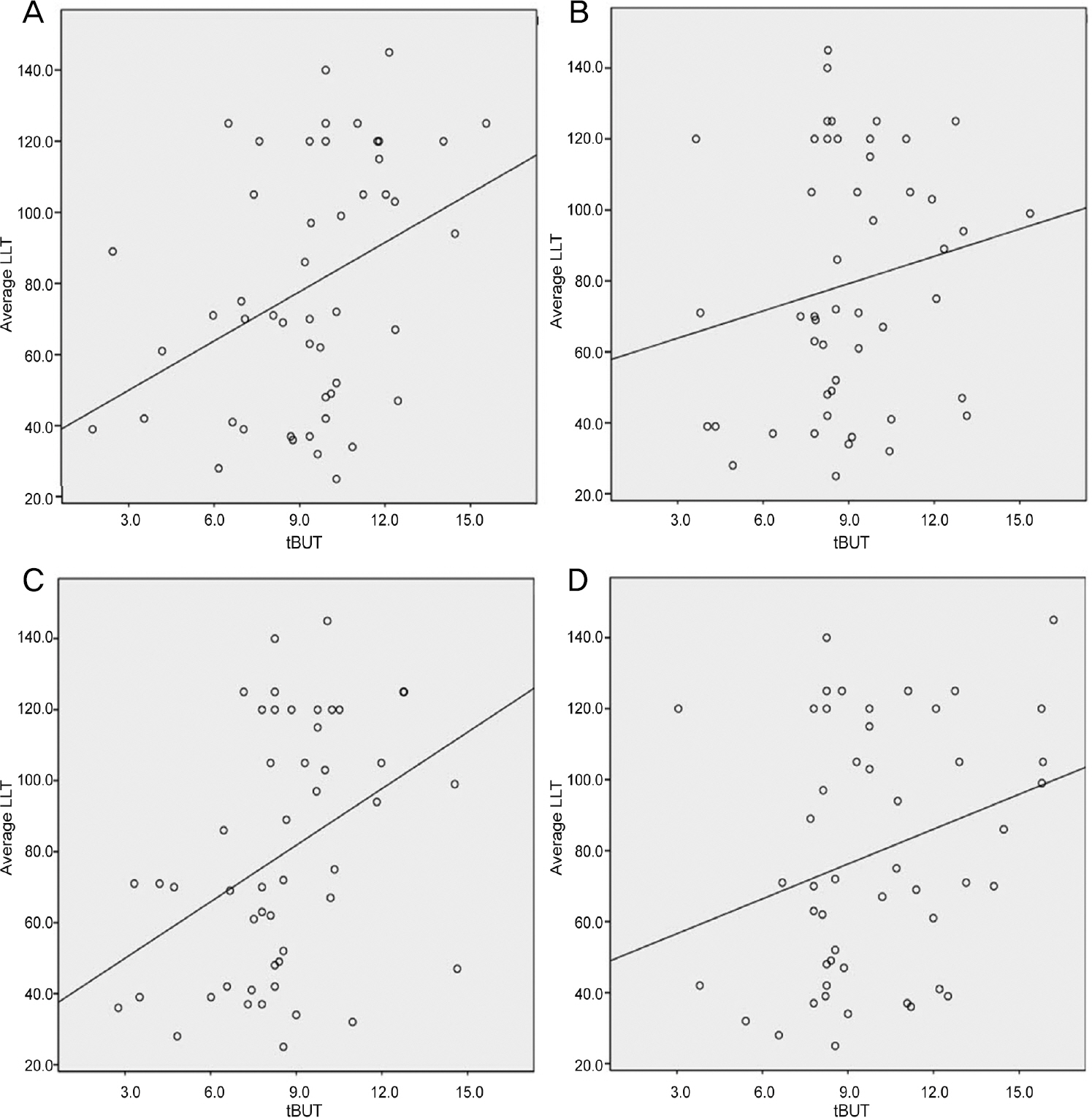
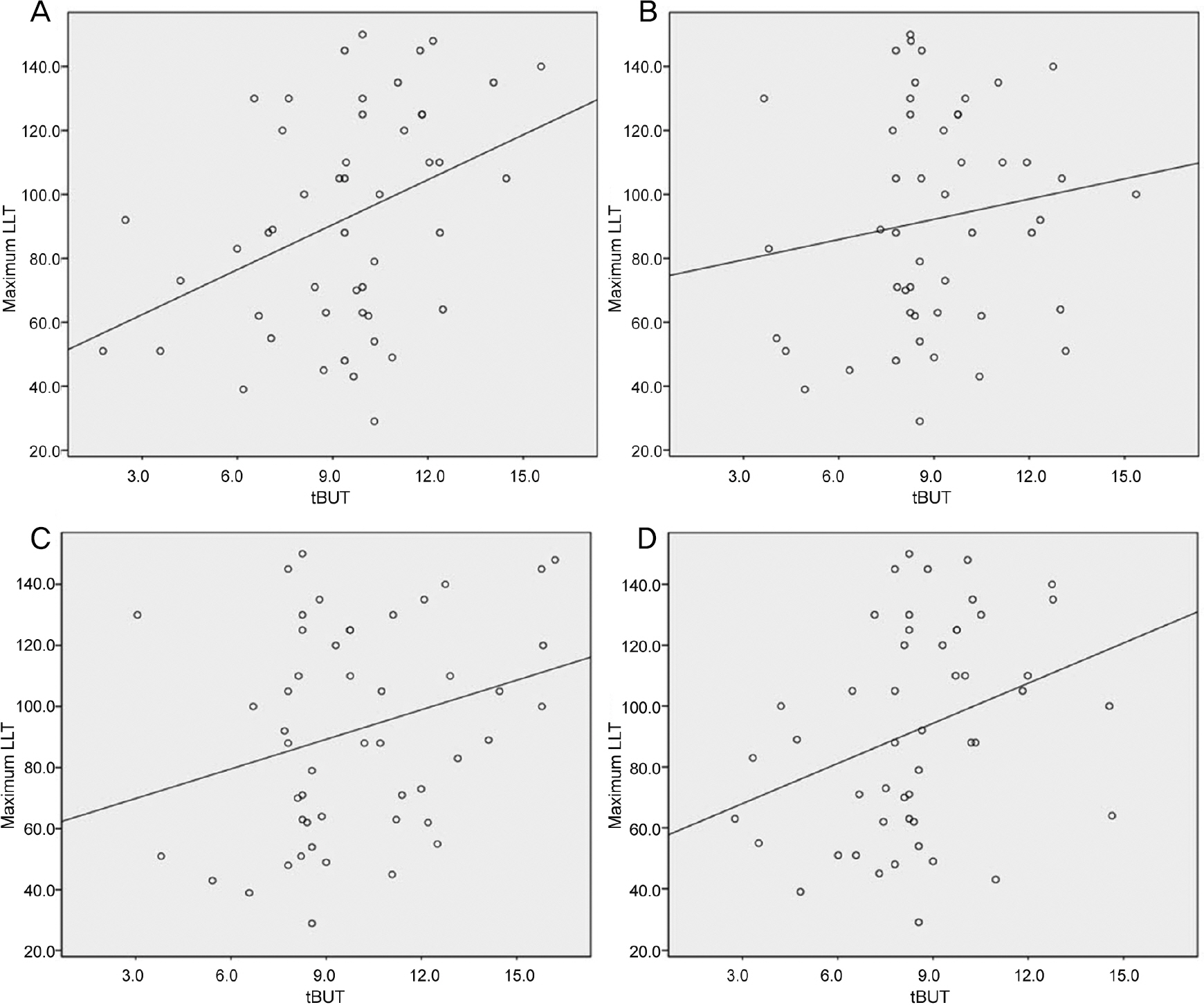
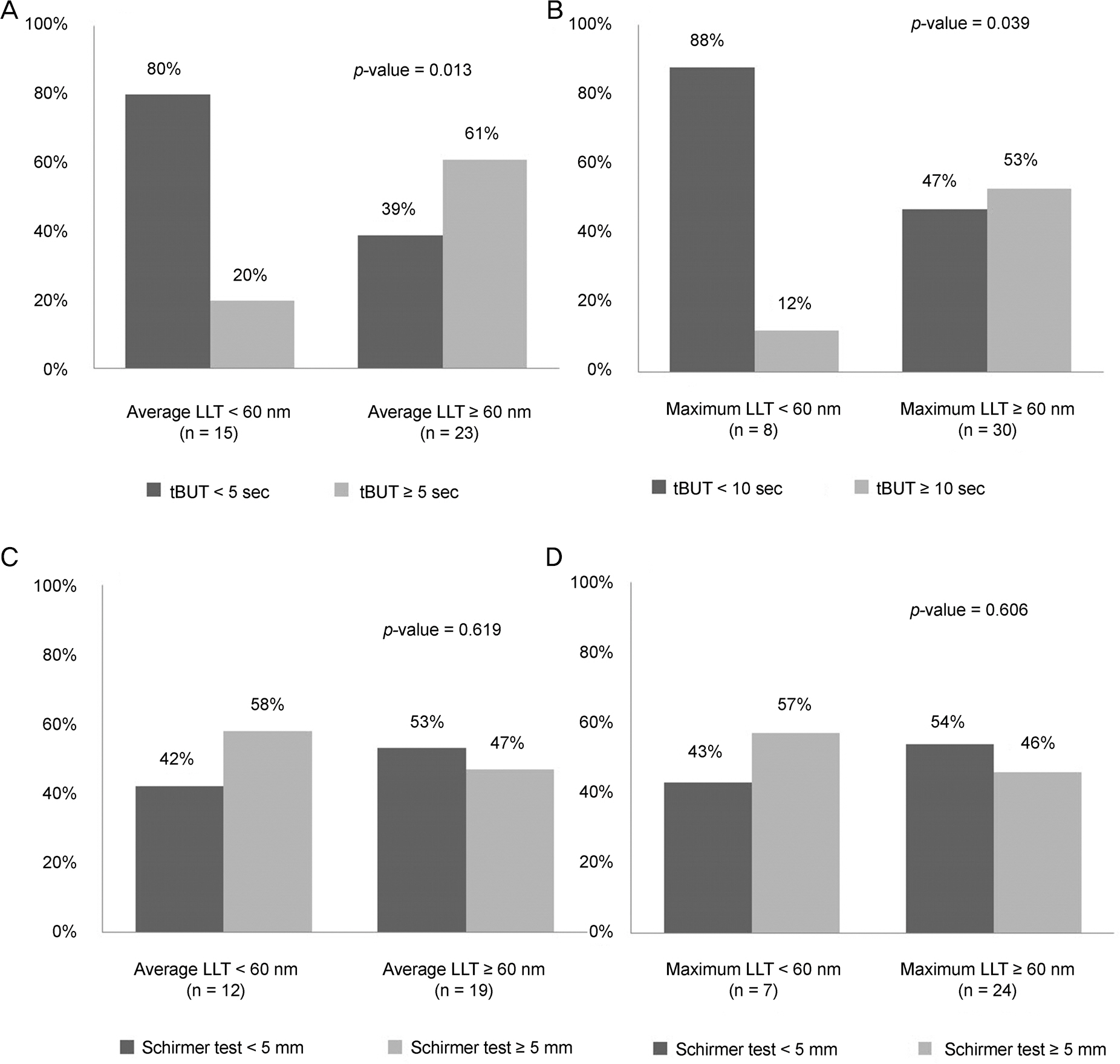
Forty-nine patients diagnosed with dry eye syndrome were recruited for this prospective study. Patients completed ocular surface disease index questionnaires. We performed slit lamp examination, Schirmer test, corneal and conjunctival fluorescein staining, measured tear film break-up time, and graded meibomian gland dysfunction. Tear LLT, blinking time, and dynamic meibomian imaging were analyzed using a LipiView II® ocular interferometer. To control for missing data, we analyzed four sets of imputated data via the multiple imputation method and performed Pearson correlation analysis. Patients were assigned to one of two LLT categories (LLT < 60 or LLT ≥ 60) and Chi-square test was performed.
RESULTS
Among ocular surface disease parameters, tear film break-up time (tBUT) had a statistically significant correlation with average and maximum LLT (average LLT; p = 0.008, 0.035, 0.006, 0.049, maximum LLT; p = 0.006, 0.042, 0.020, 0.049, Pearson correlation analysis with multiple imputation) but there was no significant correlation with minimum LLT (minimum LLT; p = 0.048, 0.090, 0.079, 0.039). Of the patients with a relatively thick average LLT or maximum LLT (LLT ≥ 60 nm), 80% and 88% had a tBUT < 10, respectively. Conversely, 39% and 47% of patients with relatively thin average LLT (LLT < 60 nm) had a tBUT < 10 (average LLT; p = 0.013, maximum LLT; p = 0.039).
CONCLUSIONS
Average LLT and maximum LLT were significantly correlated with tBUT. Patients with a relatively thin average or maximum LLT tended to have a shorter tBUT. Based on these results, measuring tear film LLT using a LipiView II® interferometer may be useful in the diagnosis and follow-up of patients with evaporative dry eye.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Shine WE, McCulley JP. The role of cholesterol in chronic blepharitis. Invest Ophthalmol Vis Sci. 1991; 32:2272–80.2. Shine WE, McCulley JP. Role of wax ester fatty alcohols in chronic blepharitis. Invest Ophthalmol Vis Sci. 1993; 34:3515–21.3. Shine WE, McCulley JP. Keratoconjunctivitis sicca associated with meibomian secretion polar lipid abnormality. Arch Ophthalmol. 1998; 116:849–52.
Article4. Shine WE, McCulley JP. Polar lipids in human meibomian gland secretions. Curr Eye Res. 2003; 26:89–94.
Article5. Bron AJ, Tiffany JM. The contribution of meibomian disease to dry eye. Ocul Surf. 2004; 2:149–65.
Article6. Foulks GN, Bron AJ. Meibomian gland dysfunction: a clinical scheme for description, diagnosis, classification, and grading. Ocul Surf. 2003; 1:107–26.
Article7. Geerling G, Tauber J, Baudouin C. . The international work-shop on meibomian gland dysfunction: report of the subcommittee on management and treatment of meibomian gland dysfunction. Invest Ophthalmol Vis Sci. 2011; 52:2050–64.
Article8. Tomlinson A, Bron AJ, Korb DR. . The international workshop on meibomian gland dysfunction: report of the diagnosis sub- committee. Invest Ophthalmol Vis Sci. 2011; 52:2006–49.9. Greiner JV, Glonek T, Korb DR. . Volume of the human and rab-bit meibomian gland system. Adv Exp Med Biol. 1998; 438:339–43.
Article10. Chew CK, Jansweijer C, Tiffany JM. . An instrument for quan-tifying meibomian lipid on the lid margin: the Meibometer. Curr Eye Res. 1993; 12:247–54.
Article11. Blackie CA, Solomon JD, Scaffidi RC. . The relationship be-tween dry eye symptoms and lipid layer thickness. Cornea. 2009; 28:789–94.
Article12. Finis D, Pischel N, Schrader S, Geerling G. Evaluation of lipid lay-er thickness measurement of the tear film as a diagnostic tool for Meibomian gland dysfunction. Cornea. 2013; 32:1549–53.
Article13. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007; 5:75–92.14. Jeon SJ, Baek JW, Doh SH, Chung SK. Tear meniscus evaluation using optical coherence tomography in meibomein gland dysfunction patients. J Korean Ophthalmol Soc. 2015; 56:1684–91.
Article15. Arita R, Itoh K, Inoue K, Amano S. Noncontact infrared meibog-raphy to document age-related changes of the meibomian glands in a normal population. Ophthalmology. 2008; 115:911–5.
Article16. Mathers WD. Ocular evaporation in meibomian gland dysfunction and dry eye. Ophthalmology. 1993; 100:347–51.
Article17. Mathers WD, Lane JA. Meibomian gland lipids, evaporation, and tear film stability. Adv Exp Med Biol. 1998; 438:349–60.
Article18. Craig JP, Tomlinson A. Importance of the lipid layer in human tear film stability and evaporation. Optom Vis Sci. 1997; 74:8–13.
Article19. Eom Y, Lee JS, Kang SY. . Correlation between quantitative measurements of tear film lipid layer thickness and meibomian gland loss in patients with obstructive meibomian gland dysfunction and normal controls. Am J Ophthalmol. 2013; 155:1104–10.e2..
Article20. Goto E, Dogru M, Fukagawa K. . Successful tear lipid layer treatment for refractory dry eye in office workers by low-dose lipid application on the full-length eyelid margin. Am J Ophthalmol. 2006; 142:264–70.
Article21. Isreb MA, Greiner JV, Korb DR. . Correlation of lipid layer thickness measurements with fluorescein tear film break-up time and Schirmer's test. Eye (Lond). 2003; 17:79–83.
Article22. Nichols JJ, Nichols KK, Puent B. . Evaluation of tear film inter-ference patterns and measures of tear break-up time. Optom Vis Sci. 2002; 79:363–9.
Article23. Korb DR, Blackie CA. Meibomian gland diagnostic expressibility: correlation with dry eye symptoms and gland location. Cornea. 2008; 27:1142–7.
Article24. Mishima S, Maurice DM. The oily layer of the tear film and evapo-ration from the corneal surface. Exp Eye Res. 1961; 1:39–45.
Article25. Nichols KK, Nichols JJ, Lynn Mitchell G. The relation between tear film tests in patients with dry eye disease. Ophthalmic Physiol Opt. 2003; 23:553–60.
Article26. Bron AJ, Tiffany JM, Gouveia SM. . Functional aspects of the tear film lipid layer. Exp Eye Res. 2004; 78:347–60.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lipid Layer Thickness in Precorneal Tear Film
- Characteristics of Tear Lipid Layer Patterns on Tearscopy and Lipid Layer Thickness
- The Effects of Warm Compression on Eyelid Temperature and Lipid Layer Thickness of Tear Film
- The Effect of Eyeliner Tattoo on Meibomian Gland Dysfunction and the Ocular Surface
- Efficacy of Intense Pulsed Light Treatment in Patients with Sjögren’s Syndrome Associated with Meibomian Gland Dysfunction