Yonsei Med J.
2014 Mar;55(2):508-516.
Low-Dose Dexmedetomidine Reduces Emergence Agitation after Desflurane Anaesthesia in Children Undergoing Strabismus Surgery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Anesthesia and Pain Research Institute, Yonsei University College of Medicine, Seoul, Korea. koobn@yuhs.ac
Abstract
- PURPOSE
Emergence agitation (EA) is frequently observed in children undergoing general anaesthesia. This study tested whether the addition of an intra-operative low-dose infusion of dexmedetomidine to fentanyl treatment reduced the incidence of emergence delirium following desflurane anesthesia in children undergoing strabismus surgery.
MATERIALS AND METHODS
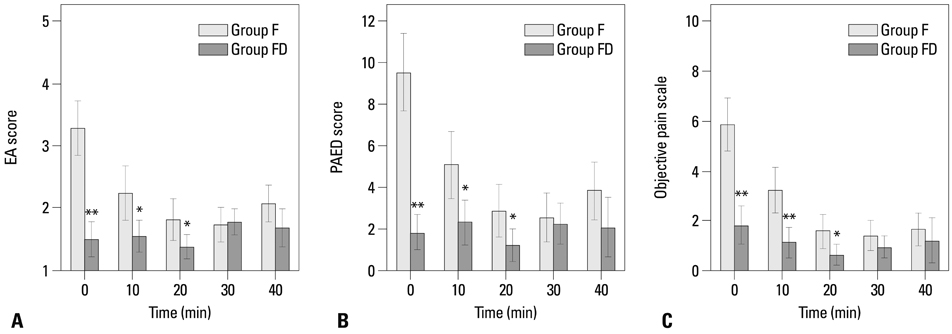
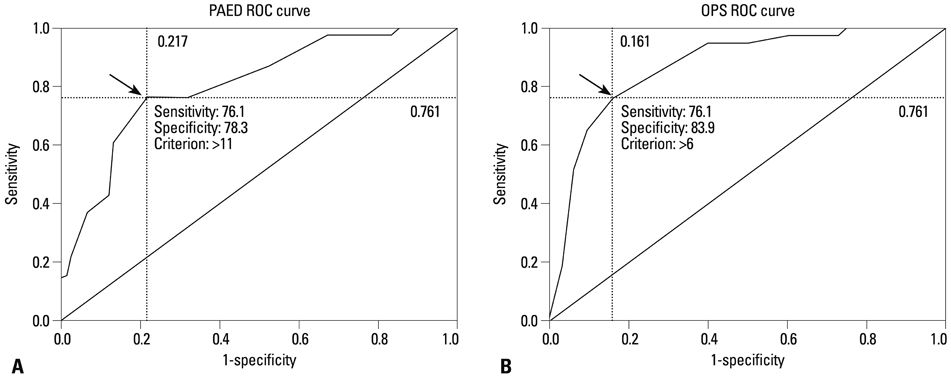
A total of 96 children (1-5 years old) undergoing strabismus surgery were enrolled. Anaesthesia was induced with propofol and maintained with desflurane. After induction, fentanyl (1 microg/kg) was administered to all children. During surgery, patients were infused with 0.2 microg/(kg.h)-1 dexmedetomidine (Group FD, n=47) or normal saline (Group F, n=47). Postoperative objective pain score (OPS), Paediatric Agitation and Emergence Delirium (PAED) score, and EA score were documented every 10 minutes in the post-anaesthesia care unit.
RESULTS
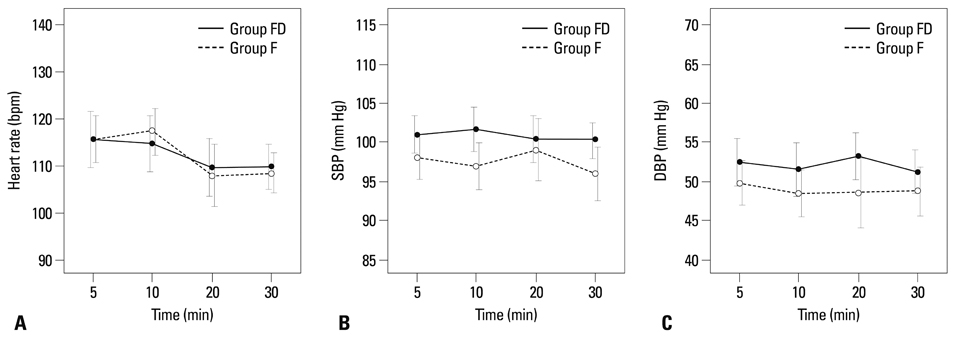
There were no significant differences between the two groups in demographic characteristics and haemodynamic changes. The mean values of maximum EA, maximum PAED, and maximum OPS score were significantly lower in Group FD than in Group F at 0, 10, and 20 minutes after arrival at the post-anaesthesia care unit (p<0.001). The frequency of fentanyl rescue was lower in Group FD than in Group F (p<0.001). The incidence of severe EA was significantly lower in Group FD than in Group F (12.8% vs. 74.5%, p<0.001).
CONCLUSION
Intra-operative low-dose infusion of dexmedetomidine in addition to fentanyl reduces EA following desflurane anaesthesia in children undergoing strabismus surgeries.
MeSH Terms
Figure
Reference
-
1. Voepel-Lewis T, Malviya S, Tait AR. A prospective cohort study of emergence agitation in the pediatric postanesthesia care unit. Anesth Analg. 2003; 96:1625–1630.
Article2. Grundmann U, Uth M, Eichner A, Wilhelm W, Larsen R. Total in travenous anaesthesia with propofol and remifentanil in paediatric patients: a comparison with a desflurane-nitrous oxide inhalation anaesthesia. Acta Anaesthesiol Scand. 1998; 42:845–850.
Article3. Dexter F, Macario A, Manberg PJ, Lubarsky DA. Computer simulation to determine how rapid anesthetic recovery protocols to decrease the time for emergence or increase the phase I postanesthesia care unit bypass rate affect staffing of an ambulatory surgery center. Anesth Analg. 1999; 88:1053–1063.
Article4. Vlajkovic GP, Sindjelic RP. Emergence delirium in children: many questions, few answers. Anesth Analg. 2007; 104:84–91.
Article5. Finley GA, McGrath PJ, Forward SP, McNeill G, Fitzgerald P. Parents' management of children's pain following 'minor' surgery. Pain. 1996; 64:83–87.
Article6. Mizrak A, Erbagci I, Arici T, Ozcan I, Ganidagli S, Tatar G, et al. Ketamine versus propofol for strabismus surgery in children. Clin Ophthalmol. 2010; 4:673–679.7. Mizrak A, Erbagci I, Arici T, Avci N, Ganidagli S, Oner U. Dexmedetomidine use during strabismus surgery in agitated children. Med Princ Pract. 2011; 20:427–432.
Article8. Jung HJ, Kim JB, Im KS, Oh SH, Lee JM. Effect of ketamine versus thiopental sodium anesthetic induction and a small dose of fentanyl on emergence agitation after sevoflurane anesthesia in children undergoing brief ophthalmic surgery. Korean J Anesthesiol. 2010; 58:148–152.
Article9. Aouad MT, Yazbeck-Karam VG, Nasr VG, El-Khatib MF, Kanazi GE, Bleik JH. A single dose of propofol at the end of surgery for the prevention of emergence agitation in children undergoing strabismus surgery during sevoflurane anesthesia. Anesthesiology. 2007; 107:733–738.
Article10. White PF, Tang J, Wender RH, Yumul R, Stokes OJ, Sloninsky A, et al. Desflurane versus sevoflurane for maintenance of outpatient anesthesia: the effect on early versus late recovery and perioperative coughing. Anesth Analg. 2009; 109:387–393.
Article11. Welborn LG, Hannallah RS, Norden JM, Ruttimann UE, Callan CM. Comparison of emergence and recovery characteristics of sevoflurane, desflurane, and halothane in pediatric ambulatory patients. Anesth Analg. 1996; 83:917–920.
Article12. Wachtel RE, Dexter F, Epstein RH, Ledolter J. Meta-analysis of desflurane and propofol average times and variability in times to extubation and following commands. Can J Anaesth. 2011; 58:714–724.
Article13. Davis PJ, Cohen IT, McGowan FX Jr, Latta K. Recovery characteristics of desflurane versus halothane for maintenance of anesthesia in pediatric ambulatory patients. Anesthesiology. 1994; 80:298–302.
Article14. Shukry M, Clyde MC, Kalarickal PL, Ramadhyani U. Does dexmedetomidine prevent emergence delirium in children after sevoflurane-based general anesthesia? Paediatr Anaesth. 2005; 15:1098–1104.
Article15. Singh R, Kharbanda M, Sood N, Mahajan V, Chatterji C. Comparative evaluation of incidence of emergence agitation and post-operative recovery profile in paediatric patients after isoflurane, sevoflurane and desflurane anaesthesia. Indian J Anaesth. 2012; 56:156–161.
Article16. Isik B, Arslan M, Tunga AD, Kurtipek O. Dexmedetomidine decreases emergence agitation in pediatric patients after sevoflurane anesthesia without surgery. Paediatr Anaesth. 2006; 16:748–753.
Article17. Weldon BC, Watcha MF, White PF. Oral midazolam in children: effect of time and adjunctive therapy. Anesth Analg. 1992; 75:51–55.18. Hannallah RS, Broadman LM, Belman AB, Abramowitz MD, Epstein BS. Comparison of caudal and ilioinguinal/iliohypogastric nerve blocks for control of post-orchiopexy pain in pediatric ambulatory surgery. Anesthesiology. 1987; 66:832–834.
Article19. Sikich N, Lerman J. Development and psychometric evaluation of the pediatric anesthesia emergence delirium scale. Anesthesiology. 2004; 100:1138–1145.
Article20. Cole JW, Murray DJ, McAllister JD, Hirshberg GE. Emergence behaviour in children: defining the incidence of excitement and agitation following anaesthesia. Paediatr Anaesth. 2002; 12:442–447.
Article21. Chung F, Chan VW, Ong D. A post-anesthetic discharge scoring system for home readiness after ambulatory surgery. J Clin Anesth. 1995; 7:500–506.
Article22. Patel A, Davidson M, Tran MC, Quraishi H, Schoenberg C, Sant M, et al. Dexmedetomidine infusion for analgesia and prevention of emergence agitation in children with obstructive sleep apnea syndrome undergoing tonsillectomy and adenoidectomy. Anesth Analg. 2010; 111:1004–1010.
Article23. Cohen IT, Finkel JC, Hannallah RS, Hummer KA, Patel KM. The effect of fentanyl on the emergence characteristics after desflurane or sevoflurane anesthesia in children. Anesth Analg. 2002; 94:1178–1181.
Article24. Demirbilek S, Togal T, Cicek M, Aslan U, Sizanli E, Ersoy MO. Effects of fentanyl on the incidence of emergence agitation in children receiving desflurane or sevoflurane anaesthesia. Eur J Anaesthesiol. 2004; 21:538–542.
Article25. Dahmani S, Stany I, Brasher C, Lejeune C, Bruneau B, Wood C, et al. Pharmacological prevention of sevoflurane- and desflurane-related emergence agitation in children: a meta-analysis of published studies. Br J Anaesth. 2010; 104:216–223.
Article26. Kim MS, Moon BE, Kim H, Lee JR. Comparison of propofol and fentanyl administered at the end of anaesthesia for prevention of emergence agitation after sevoflurane anaesthesia in children. Br J Anaesth. 2013; 110:274–280.
Article27. Davis PJ, Greenberg JA, Gendelman M, Fertal K. Recovery characteristics of sevoflurane and halothane in preschool-aged children undergoing bilateral myringotomy and pressure equalization tube insertion. Anesth Analg. 1999; 88:34–38.
Article28. Cravero JP, Beach M, Thyr B, Whalen K. The effect of small dose fentanyl on the emergence characteristics of pediatric patients after sevoflurane anesthesia without surgery. Anesth Analg. 2003; 97:364–367.
Article29. Finkel JC, Cohen IT, Hannallah RS, Patel KM, Kim MS, Hummer KA, et al. The effect of intranasal fentanyl on the emergence characteristics after sevoflurane anesthesia in children undergoing surgery for bilateral myringotomy tube placement. Anesth Analg. 2001; 92:1164–1168.
Article30. Messerer B, Gutmann A, Weinberg A, Sandner-Kiesling A. Implementation of a standardized pain management in a pediatric surgery unit. Pediatr Surg Int. 2010; 26:879–889.
Article31. Bong CL, Ng AS. Evaluation of emergence delirium in Asian children using the Pediatric Anesthesia Emergence Delirium Scale. Paediatr Anaesth. 2009; 19:593–600.
Article32. Blankespoor RJ, Janssen NJ, Wolters AM, Van Os J, Schieveld JN. Post-hoc revision of the pediatric anesthesia emergence delirium rating scale: clinical improvement of a bedside-tool? Minerva Anestesiol. 2012; 78:896–900.33. Janssen NJ, Tan EY, Staal M, Janssen EP, Leroy PL, Lousberg R, et al. On the utility of diagnostic instruments for pediatric delirium in critical illness: an evaluation of the Pediatric Anesthesia Emergence Delirium Scale, the Delirium Rating Scale 88, and the Delirium Rating Scale-Revised R-98. Intensive Care Med. 2011; 37:1331–1337.
Article34. Chen J, Li W, Hu X, Wang D. Emergence agitation after cataract surgery in children: a comparison of midazolam, propofol and ketamine. Paediatr Anaesth. 2010; 20:873–879.
Article35. Erdil F, Demirbilek S, Begec Z, Ozturk E, Ulger MH, Ersoy MO. The effects of dexmedetomidine and fentanyl on emergence characteristics after adenoidectomy in children. Anaesth Intensive Care. 2009; 37:571–576.
Article36. Saadawy I, Boker A, Elshahawy MA, Almazrooa A, Melibary S, Abdellatif AA, et al. Effect of dexmedetomidine on the characteristics of bupivacaine in a caudal block in pediatrics. Acta Anaesthesiol Scand. 2009; 53:251–256.
Article37. Akin A, Bayram A, Esmaoglu A, Tosun Z, Aksu R, Altuntas R, et al. Dexmedetomidine vs midazolam for premedication of pediatric patients undergoing anesthesia. Paediatr Anaesth. 2012; 22:871–876.
Article38. Tufanogullari B, White PF, Peixoto MP, Kianpour D, Lacour T, Griffin J, et al. Dexmedetomidine infusion during laparoscopic bariatric surgery: the effect on recovery outcome variables. Anesth Analg. 2008; 106:1741–1748.
Article39. Bhana N, Goa KL, McClellan KJ. Dexmedetomidine. Drugs. 2000; 59:263–268.
Article40. Deutsch E, Tobias JD. Hemodynamic and respiratory changes following dexmedetomidine administration during general anesthesia: sevoflurane vs desflurane. Paediatr Anaesth. 2007; 17:438–444.
Article41. Braun U, Feise J, Mühlendyck H. Is there a cholinergic and an adrenergic phase of the oculocardiac reflex during strabismus surgery? Acta Anaesthesiol Scand. 1993; 37:390–395.
Article42. Guler G, Akin A, Tosun Z, Ors S, Esmaoglu A, Boyaci A. Single-dose dexmedetomidine reduces agitation and provides smooth extubation after pediatric adenotonsillectomy. Paediatr Anaesth. 2005; 15:762–766.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Nalbuphine on Emergence Agitation and Recovery after Desflurane Anesthesia in Children for Strabismus Surgery
- Optimal dose of fentanyl for the prevention of emergence agitation after desflurane anesthesia in children undergoing tonsillectomy
- Comparison of Thiopental Sodium and Ketamine Induction on Emergence Agitation after Desflurane Anesthesia in Children undergoing a Tonsillectomy
- Effect of Dexmedetomidine on Sevoflurane Requirements and Emergence Agitation in Children Undergoing Ambulatory Surgery
- Effects of propofol and nalbuphine on emergence agitation after sevoflurane anesthesia in children for strabismus surgery