Kosin Med J.
2017 Jun;32(1):90-98. 10.7180/kmj.2017.32.1.90.
A Case of Steroid Resistant Minimal Change Disease Associated with Portal Vein Thrombosis Treated by Combined Immunosuppressive Agents
- Affiliations
-
- 1Department of Internal Medicine, Dong-A University College of Medicine, Busan, Korea. anws@dau.ac.kr
- 2Department of Pathology, Dong-A University College of Medicine, Busan, Korea.
- KMID: 2384837
- DOI: http://doi.org/10.7180/kmj.2017.32.1.90
Abstract
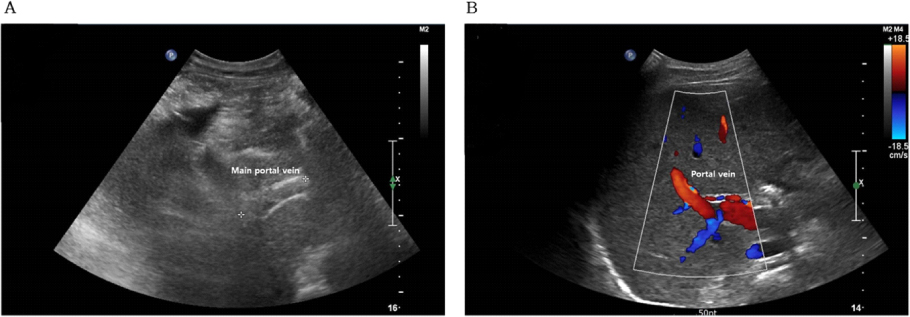
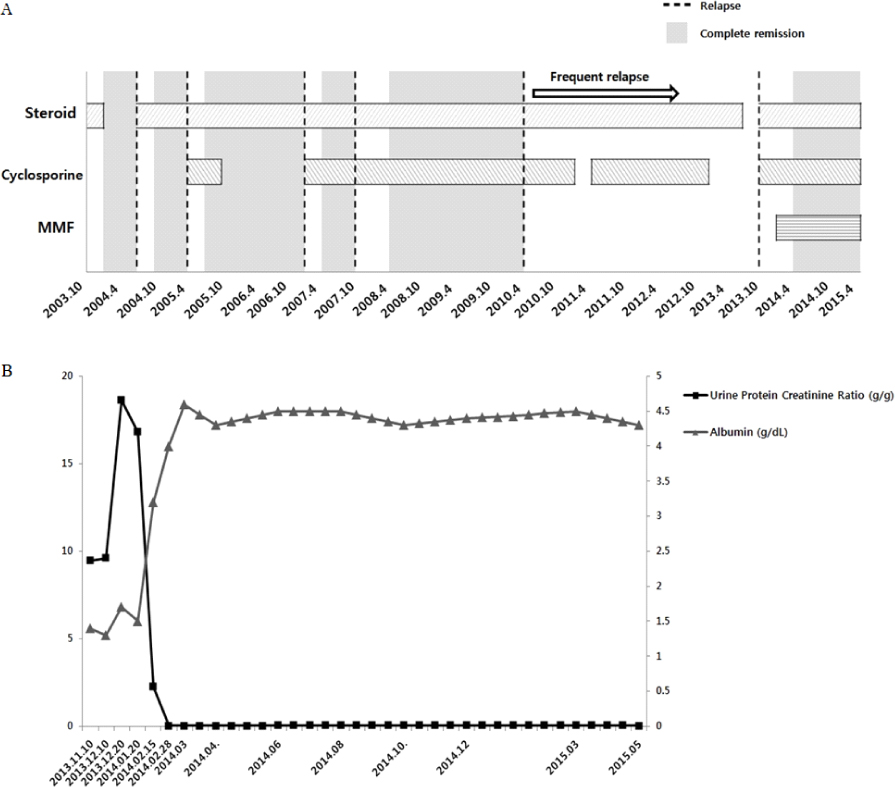
- Minimal change disease (MCD) is a common cause of nephrotic syndrome and relatively well responds with steroid treatment. However, nearly half of patients with MCD experience recurrence of nephrotic syndrome. Thromboembolic events including renal vein thrombosis may occur in patients with MCD, but portal vein thrombosis rarely occurs. We experienced a case of frequent relapse/steroid dependent MCD with nephrotic syndrome progressed to steroid resistance associated with portal vein thrombosis. This patient showed complete remission of MCD and resolution of portal vein thrombosis after treatment with corticosteroid, cyclosporine, mycophenolate mofetil, and anticoagulant.
MeSH Terms
Figure
Reference
-
1. Singhal R, Brimble KS. Thromboembolic complications in the nephrotic syndrome: pathophysiology and clinical management. Thromb Res. 2006; 118:397–407.
Article2. Mahmoodi BK, ten Kate MK, Waanders F, Veeger NJ, Brouwer JL, Vogt L, et al. High absolute risks and predictors of venous and arterial thromboembolic events in patients with nephrotic syndrome: results from a large retrospective cohort study. Circulation. 2008; 117:224–230.
Article3. Hogan J, Radhakrishnan J. The treatment of minimal change disease in adults. J Am Soc Nephrol. 2013; 24:702–711.
Article4. Nakayama M, Katafuchi R, Yanase T, Ikeda K, Tanaka H, Fujimi S. Steroid responsiveness and frequency of relapse in adult-onset minimal change nephrotic syndrome. Am J Kidney Dis. 2002; 39:503–512.
Article5. Waldman M, Crew RJ, Valeri A, Busch J, Stokes B, Markowitz G, et al. Adult minimal-change disease: clinical characteristics, treatment, and outcomes. Clin J Am Soc Nephrol. 2007; 2:445–453.
Article6. Korbet SM, Schwartz MM, Lewis EJ. Minimal-change glomerulopathy of adulthood. Am J Nephrol. 1988; 8:291–297.
Article7. Zhao M, Chen X, Chen Y, Liu Z, Liu Y, Lu F, et al. Clinical observations of mycophenolate mofetil therapy in refractory primary nephrotic syndrome. Nephrology (Carlton). 2003; 8:105–109.
Article8. Ponticelli C, Edefonti A, Ghio L, Rizzoni G, Rinaldi S, Gusmano R, et al. Cyclosporine versus cyclophosphamide for patients with steroid-dependent and frequently relapsing idiopathic nephrotic syndrome: a multicenter randomized controlled trial. Nephrol Dial Transplant. 1993; 8:1326–1332.9. Eguchi A, Takei T, Yoshida T, Tsuchiya K, Nitta K. Combined cyclosporine and prednisolone therapy in adult patients with the first relapse of minimal-change nephrotic syndrome. Nephrol Dial Transplant. 2010; 25:124–129.
Article10. Mak SK, Short CD, Mallick NP. Long-term outcome of adult-onset minimal-change nephropathy. Nephrol Dial Transplant. 1996; 11:2192–2202.
Article11. Shigidi MM. The treatment of relapse in adults with minimal change nephrotic syndrome: myths and facts. Saudi J Kidney Dis Transpl. 2011; 22:10–17.12. Day CJ, Cockwell P, Lipkin GW, Savage CO, Howie AJ, Adu D. Mycophenolate mofetil in the treatment of resistant idiopathic nephrotic syndrome. Nephrol Dial Transplant. 2002; 17:2011–2013.
Article13. Fujinaga S, Ohtomo Y, Umino D, Takemoto M, Shimizu T, Yamashiro Y, et al. A prospective study on the use of mycophenolate mofetil in children with cyclosporine-dependent nephrotic syndrome. Pediatr Nephrol. 2007; 22:71–76.
Article14. Kerlin BA, Ayoob R, Smoyer WE. Epidemiology and pathophysiology of nephrotic syndrome-associated thromboembolic disease. Clin J Am Soc Nephrol. 2012; 7:513–520.
Article15. Eneman B, Levtchenko E, van den Heuvel B, Van Geet C, Freson K. Platelet abnormalities in nephrotic syndrome. Pediatr Nephrol. 2016; 31:1267–1279.
Article16. Suri D, Ahluwalia J, Saxena AK, Sodhi KS, Singh P, Mittal BR, et al. Thromboembolic complications in childhood nephrotic syndrome: a clinical profile. Clin Exp Nephrol. 2014; 18:803–813.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Portal Vein Thrombosis in Minimal Change Disease
- Acute Appendicitis with Superior Mesenteric Vein Thrombosis and Portal Vein Thrombosis
- Portal Vein Thrombosis in Liver Cirrhosis: A case report
- Radiologic Findings of Neonatal Cerebral Infarction related with Portal Vein Thrombosis: Case Report
- Nephrotic syndrome complicated with portal, splenic, and superior mesenteric vein thrombosis