Endocrinol Metab.
2017 Jun;32(2):248-256. 10.3803/EnM.2017.32.2.248.
Association between Body Weight Changes and Menstrual Irregularity: The Korea National Health and Nutrition Examination Survey 2010 to 2012
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. hwanx2@catholic.ac.kr
- 2Department of Medical Statistics, College of Medicine, The Catholic University of Korea, Seoul, Korea. ygpark@catholic.ac.kr
- 3Department of Obstetrics and Gynecology, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 4Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2384084
- DOI: http://doi.org/10.3803/EnM.2017.32.2.248
Abstract
- BACKGROUND
Menstrual irregularity is an indicator of endocrine disorders and reproductive health status. It is associated with various diseases and medical conditions, including obesity and underweight. We aimed to assess the association between body weight changes and menstrual irregularity in Korean women.
METHODS
A total of 4,621 women 19 to 54 years of age who participated in the 2010 to 2012 Korea National Health and Nutrition Examination Survey were included in this study. Self-reported questionnaires were used to collect medical information assessing menstrual health status and body weight changes. Odds ratios (ORs) and 95% confidence interval (CI) were calculated to evaluate the association between body weight changes and menstrual irregularity.
RESULTS
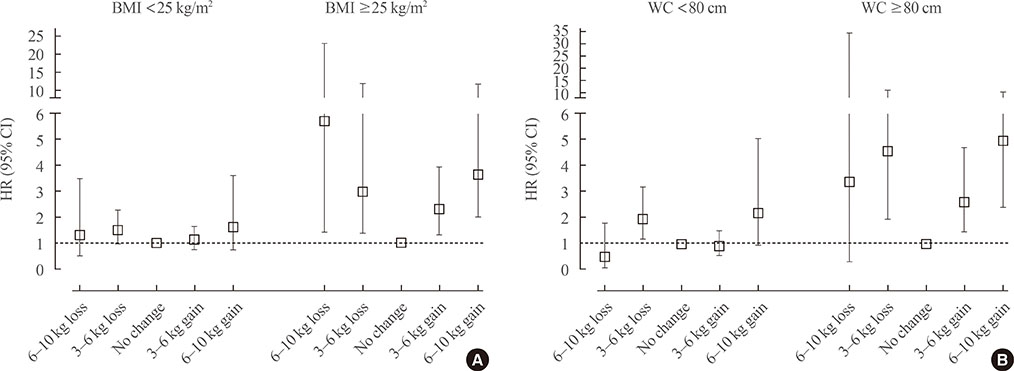
Significantly higher ORs (95% CI) were observed in the association between menstrual irregularity and both weight loss (OR, 1.74; 95% CI, 1.22 to 2.48) and weight gain (OR, 1.45; 95% CI, 1.13 to 1.86) after adjusting for age, body mass index, current smoking, heavy alcohol drinking, regular exercise, calorie intake, education, income, metabolic syndrome, age of menarche, parity, and stress perception. Of note, significant associations were only observed in subjects with obesity and abdominal obesity, but not in non-obese or non-abdominally obese subjects. U-shaped patterns were demonstrated in both obese and abdominally obese subjects, indicating that greater changes in body weight are associated with higher odds of menstrual irregularity.
CONCLUSION
We found a U-shaped pattern of association between body weight changes and menstrual irregularity among obese women in the general Korean population. This result indicates that not only proper weight management but also changes in body weight may influence the regulation of the menstrual cycle.
MeSH Terms
Figure
Reference
-
1. Rowland AS, Baird DD, Long S, Wegienka G, Harlow SD, Alavanja M, et al. Influence of medical conditions and lifestyle factors on the menstrual cycle. Epidemiology. 2002; 13:668–674.2. Palm-Fischbacher S, Ehlert U. Dispositional resilience as a moderator of the relationship between chronic stress and irregular menstrual cycle. J Psychosom Obstet Gynaecol. 2014; 35:42–50.3. Lee SS, Kim DH, Nam GE, Nam HY, Kim YE, Lee SH, et al. Association between metabolic syndrome and menstrual irregularity in middle-aged Korean women. Korean J Fam Med. 2016; 37:31–36.4. Kim MJ, Lim NK, Choi YM, Kim JJ, Hwang KR, Chae SJ, et al. Prevalence of metabolic syndrome is higher among non-obese PCOS women with hyperandrogenism and menstrual irregularity in Korea. PLoS One. 2014; 9:e99252.5. Gast GC, Grobbee DE, Smit HA, Bueno-de-Mesquita HB, Samsioe GN, van der Schouw YT. Menstrual cycle characteristics and risk of coronary heart disease and type 2 diabetes. Fertil Steril. 2010; 94:2379–2381.6. Solomon CG, Hu FB, Dunaif A, Rich-Edwards J, Willett WC, Hunter DJ, et al. Long or highly irregular menstrual cycles as a marker for risk of type 2 diabetes mellitus. JAMA. 2001; 286:2421–2426.7. Han K, Ko Y, Park YG, Park JB. Associations between the periodontal disease in women before menopause and menstrual cycle irregularity: the 2010-2012 Korea National Health and Nutrition Examination Survey. Medicine (Baltimore). 2016; 95:e2791.8. Karlson EW, Mandl LA, Hankinson SE, Grodstein F. Do breast-feeding and other reproductive factors influence future risk of rheumatoid arthritis? Results from the Nurses' Health Study. Arthritis Rheum. 2004; 50:3458–3467.9. Song JY, Kim MH, Paik JS, Kim HS, Na KS. Epidemiologic Survey Committee of the Korean Ophthalmologic Society. Association between menstrual irregularity and dry eye disease: a population-based study. Cornea. 2016; 35:193–198.10. Delara M, Woodgate RL. Psychological distress and its correlates among university students: a cross-sectional study. J Pediatr Adolesc Gynecol. 2015; 28:240–244.11. Nagma S, Kapoor G, Bharti R, Batra A, Batra A, Aggarwal A, et al. To evaluate the effect of perceived stress on menstrual function. J Clin Diagn Res. 2015; 9:QC01–QC03.12. Kaplan JR, Manuck SB. Ovarian dysfunction, stress, and disease: a primate continuum. ILAR J. 2004; 45:89–115.13. Yavangi M, Amirzargar MA, Amirzargar N, Dadashpour M. Does Ramadan fasting has any effects on menstrual cycles? Iran J Reprod Med. 2013; 11:145–150.14. Chen EC, Brzyski RG. Exercise and reproductive dysfunction. Fertil Steril. 1999; 71:1–6.15. Seth B, Arora S, Singh R. Association of obesity with hormonal imbalance in infertility: a cross-sectional study in north Indian women. Indian J Clin Biochem. 2013; 28:342–347.16. Yilmaz N, Kilic S, Kanat-Pektas M, Gulerman C, Mollamahmutoglu L. The relationship between obesity and fecundity. J Womens Health (Larchmt). 2009; 18:633–636.17. Lee DH, Jung KY, Park KS, Kim KM, Moon JH, Lim S, et al. Characterization of patients with type 2 diabetes according to body mass index: Korea National Health and Nutrition Examination Survey from 2007 to 2011. Endocrinol Metab (Seoul). 2015; 30:514–521.18. Lim JS, Choi YJ, Kim SK, Huh BW, Lee EJ, Huh KB. Optimal waist circumference cutoff value based on insulin resistance and visceral obesity in Koreans with type 2 diabetes. Diabetes Metab J. 2015; 39:253–263.19. Yoon YS, Oh SW. Optimal waist circumference cutoff values for the diagnosis of abdominal obesity in Korean adults. Endocrinol Metab (Seoul). 2014; 29:418–426.20. Seif MW, Diamond K, Nickkho-Amiry M. Obesity and menstrual disorders. Best Pract Res Clin Obstet Gynaecol. 2015; 29:516–527.21. Wei S, Schmidt MD, Dwyer T, Norman RJ, Venn AJ. Obesity and menstrual irregularity: associations with SHBG, testosterone, and insulin. Obesity (Silver Spring). 2009; 17:1070–1076.22. Kuokkanen S, Polotsky AJ, Chosich J, Bradford AP, Jasinska A, Phang T, et al. Corpus luteum as a novel target of weight changes that contribute to impaired female reproductive physiology and function. Syst Biol Reprod Med. 2016; 62:227–242.23. Butzow TL, Lehtovirta M, Siegberg R, Hovatta O, Koistinen R, Seppala M, et al. The decrease in luteinizing hormone secretion in response to weight reduction is inversely related to the severity of insulin resistance in overweight women. J Clin Endocrinol Metab. 2000; 85:3271–3275.24. Frisch RE. The right weight: body fat, menarche and fertility. Proc Nutr Soc. 1994; 53:113–129.25. Stracciolini A, Quinn BJ, Geminiani E, Kinney S, McCrystal T, Owen M, et al. Body mass index and menstrual patterns in dancers. Clin Pediatr (Phila). 2016; 04. 18. [Epub]. DOI: 10.1177/0009922816642202.26. Prentice P, Viner RM. Pubertal timing and adult obesity and cardiometabolic risk in women and men: a systematic review and meta-analysis. Int J Obes (Lond). 2013; 37:1036–1043.27. Lim SW, Ahn JH, Lee JA, Kim DH, Seo JH, Lim JS. Early menarche is associated with metabolic syndrome and insulin resistance in premenopausal Korean women. Eur J Pediatr. 2016; 175:97–104.28. Day FR, Elks CE, Murray A, Ong KK, Perry JR. Puberty timing associated with diabetes, cardiovascular disease and also diverse health outcomes in men and women: the UK Biobank study. Sci Rep. 2015; 5:11208.29. Chang PJ, Chen PC, Hsieh CJ, Chiu LT. Risk factors on the menstrual cycle of healthy Taiwanese college nursing students. Aust N Z J Obstet Gynaecol. 2009; 49:689–694.30. Edozien LC. Mind over matter: psychological factors and the menstrual cycle. Curr Opin Obstet Gynecol. 2006; 18:452–456.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association between Awareness of Nutrition Labels and Menstrual Cycle Irregularity in Korean Women: The Fifth Korea National Health and Nutrition Examination Survey (2010~2012)
- Association between Metabolic Syndrome and Menstrual Irregularity in Middle-Aged Korean Women
- Body Weight Perception, Mental Health, and Weight Control Behavior in Normal Weight Adolescents: Based on the Korea National Health and Nutrition Examination Survey 2013-2015
- Association of Breastfeeding Duration with Menopausal Age and Menstrual Period: Analysis based on the Korea National Health and Nutrition Examination Survey 2016–2018
- Effects of the difference between actual body condition and body image perception on nutrient intake, weight control and mental health in Korean adults: Based on the 5th Korea National Health and Nutrition Examination Survey