Korean J Crit Care Med.
2017 May;32(2):124-132. 10.4266/kjccm.2017.00199.
Epidemiology and Clinical Characteristics of Rapid Response Team Activations
- Affiliations
-
- 1Division of Pulmonology and Critical Care Medicine, Department of Internal Medicine, Daejeon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Daejeon, Korea.
- 2Division of Pulmonology and Critical Care Medicine, Department of Internal Medicine, Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea.
- 3St. Mary's Advanced Life Support Team, Department of Nursing, Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 4St. Mary's Advanced Life Support Team, Division of Pulmonology, Allergy and Critical Care Medicine, Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. cmcksc@gmail.com
- KMID: 2384037
- DOI: http://doi.org/10.4266/kjccm.2017.00199
Abstract
- BACKGROUND
To ensure patient safety and improvements in the quality of hospital care, rapid response teams (RRTs) have been implemented in many countries, including Korea. The goal of an RRT is early identification and response to clinical deterioration in patients. However, there are differences in RRT systems among hospitals and limited data are available.
METHODS
In Seoul St. Mary's Hospital, the St. Mary's Advanced Life Support Team was implemented in June 2013. We retrospectively reviewed the RRT activation records of 287 cases from June 2013 to December 2016.
RESULTS
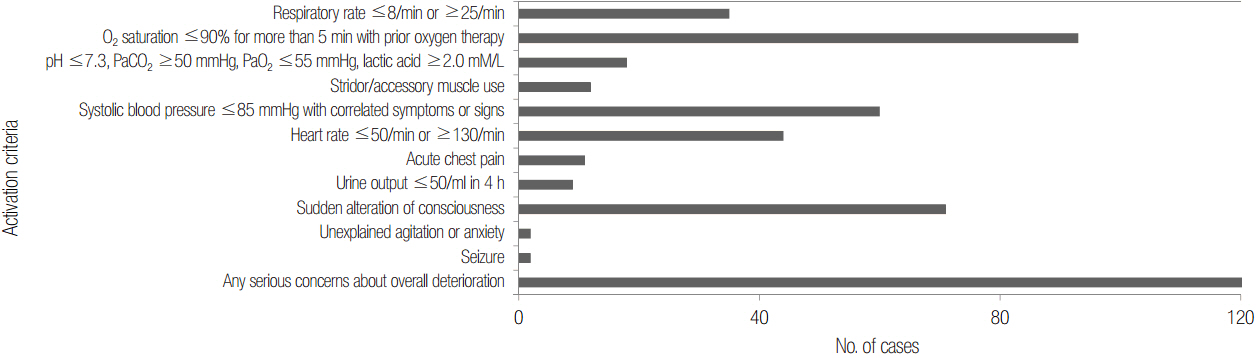
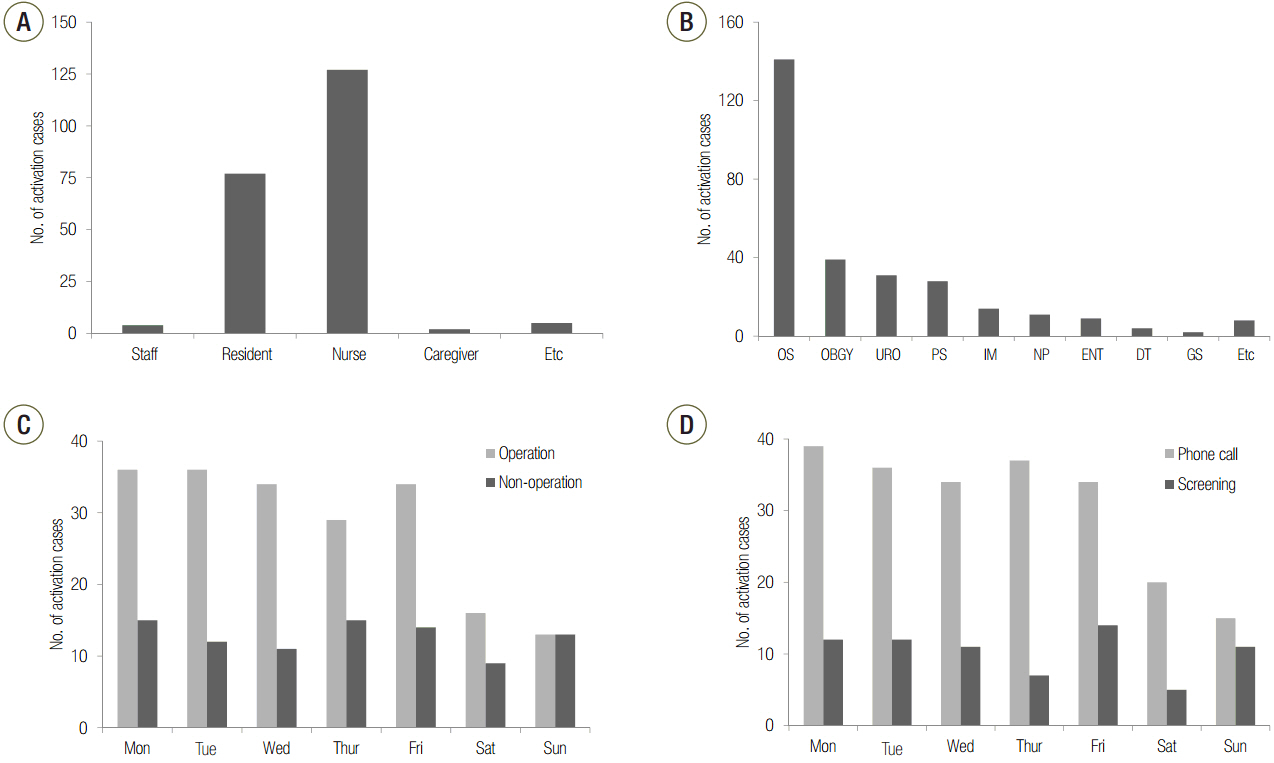
The median response time and median modified early warning score were 8.6 minutes (interquartile range, 5.6 to 11.6 minutes) and 5.0 points (interquartile range, 4.0 to 7.0 points), respectively. Residents (35.8%) and nurses (59.1%) were the main activators of the RRT. Interestingly, postoperative patients account for a large percentage of the RRT activation cases (69.3%). The survival rate was 83.6% and survival was mainly associated with malignancy, Acute Physiology and Chronic Health Evaluation-II score, and the time from admission to RRT activation. RRT activation with screening showed a better outcome compared to activation via a phone call in terms of the intensive care unit admission rate and length of hospital stay after RRT activation.
CONCLUSIONS
Malignancy was the most important factor related to survival. In addition, RRT activation with patient screening showed a better outcome compared to activation via a phone call. Further studies are needed to determine the effective screening criteria and improve the quality of the RRT system.
MeSH Terms
Figure
Cited by 1 articles
-
Rapid response systems in Korea
Bo Young Lee, Sang-Bum Hong
Acute Crit Care. 2019;34(2):108-116. doi: 10.4266/acc.2019.00535.
Reference
-
References
1. Devita MA, Bellomo R, Hillman K, Kellum J, Rotondi A, Teres D, et al. Findings of the first consensus conference on medical emergency teams. Crit Care Med. 2006; 34:2463–78.
Article2. Buist MD, Jarmolowski E, Burton PR, Bernard SA, Waxman BP, Anderson J. Recognising clinical instability in hospital patients before cardiac arrest or unplanned admission to intensive care: a pilot study in a tertiary-care hospital. Med J Aust. 1999; 171:22–5.
Article3. Jones DA, DeVita MA, Bellomo R. Rapid-response teams. N Engl J Med. 2011; 365:139–46.
Article4. Franklin C, Mathew J. Developing strategies to prevent inhospital cardiac arrest: analyzing responses of physicians and nurses in the hours before the event. Crit Care Med. 1994; 22:244–7.
Article5. Hillman KM, Bristow PJ, Chey T, Daffurn K, Jacques T, Norman SL, et al. Antecedents to hospital deaths. Intern Med J. 2001; 31:343–8.
Article6. Chen J, Ou L, Flabouris A, Hillman K, Bellomo R, Parr M. Impact of a standardized rapid response system on outcomes in a large healthcare jurisdiction. Resuscitation. 2016; 107:47–56.
Article7. Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid response teams: a systematic review and meta-analysis. Arch Intern Med. 2010; 170:18–26.8. Jung B, Daurat A, De Jong A, Chanques G, Mahul M, Monnin M, et al. Rapid response team and hospital mortality in hospitalized patients. Intensive Care Med. 2016; 42:494–504.
Article9. Salvatierra G, Bindler RC, Corbett C, Roll J, Daratha KB. Rapid response team implementation and inhospital mortality. Crit Care Med. 2014; 42:2001–6.
Article10. White K, Scott IA, Vaux A, Sullivan CM. Rapid response teams in adult hospitals: time for another look? Intern Med J. 2015; 45:1211–20.
Article11. Lee YJ, Lee DS, Min H, Choi YY, Lee EY, Song I, et al. Differences in the clinical characteristics of rapid response system activation in patients admitted to medical or surgical services. J Korean Med Sci. 2017; 32:688–94.
Article12. Kwak HJ, Yun I, Kim SH, Sohn JW, Shin DH, Yoon HJ, et al. The extended rapid response system: 1-year experience in a university hospital. J Korean Med Sci. 2014; 29:423–30.
Article13. Huh JW, Lim CM, Koh Y, Lee J, Jung YK, Seo HS, et al. Activation of a medical emergency team using an electronic medical recording-based screening system. Crit Care Med. 2014; 42:801–8.
Article14. Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. BMJ. 2002; 324:387–90.
Article15. Dacey MJ, Mirza ER, Wilcox V, Doherty M, Mello J, Boyer A, et al. The effect of a rapid response team on major clinical outcome measures in a community hospital. Crit Care Med. 2007; 35:2076–82.
Article16. Jones D, Bellomo R, Bates S, Warrillow S, Gold-smith D, Hart G, et al. Long term effect of a medical emergency team on cardiac arrests in a teaching hospital. Crit Care. 2005; 9:R808–15.17. Sebat F, Musthafa AA, Johnson D, Kramer AA, Shoffner D, Eliason M, et al. Effect of a rapid response system for patients in shock on time to treatment and mortality during 5 years. Crit Care Med. 2007; 35:2568–75.
Article18. McGaughey J, Alderdice F, Fowler R, Kapila A, Mayhew A, Moutray M. Outreach and Early Warning Systems (EWS) for the prevention of intensive care admission and death of critically ill adult patients on general hospital wards. Cochrane Database Syst Rev. 2007; (3):CD005529.
Article19. Hillman K, Chen J, Cretikos M, Bellomo R, Brown D, Doig G, et al. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet. 2005; 365:2091–7.20. Jones D. The epidemiology of adult rapid response team patients in Australia. Anaesth Intensive Care. 2014; 42:213–9.
Article21. Bannard-Smith J, Lighthall GK, Subbe CP, Durham L, Welch J, Bellomo R, et al. Clinical outcomes of patients seen by rapid response teams: a template for benchmarking international teams. Resuscitation. 2016; 107:7–12.
Article22. Jones D, Bellomo R, DeVita MA. Effectiveness of the medical emergency team: the importance of dose. Crit Care. 2009; 13:313.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of Medical Emergency Team Activation in Surgical Wards
- Implementation and Outcomes of a Difficult Airway Code Team Composed of Anesthesiologists in a Korean Tertiary Hospital: A Retrospective Analysis of a Prospective Registry
- Factors Influencing the Activation Time of the Rapid Response Team
- Effects of a Rapid Response Team on the Clinical Outcomes of Cardiopulmonary Resuscitation of Patients Hospitalized in General Wards
- The Extended Rapid Response System: 1-Year Experience in a University Hospital