J Endocr Surg.
2017 Jun;17(2):73-79. 10.16956/jes.2017.17.2.73.
Clinical Experience of Isolated Metachronous Adrenal Gland Metastases from Solid Primary Carcinomas
- Affiliations
-
- 1Department of Surgery, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. tysung@amc.seoul.kr
- KMID: 2383824
- DOI: http://doi.org/10.16956/jes.2017.17.2.73
Abstract
- PURPOSE
Owing to the development of improved techniques, the use of adrenal gland surgery for the treatment of metachronous metastatic adrenal tumors originating from primary carcinomas has increased. Here, we have analyzed the postoperative outcomes of patients who received surgical treatment for isolated metastatic adrenal gland originated from solid primary carcinomas.
METHODS
Patients who underwent metastatic adrenalectomy after treatment of the primary carcinoma at the Asan Medical Center from 2000 to 2010 were included. Clinicopathological parameters were analyzed to determine the prognostic outcomes.
RESULTS
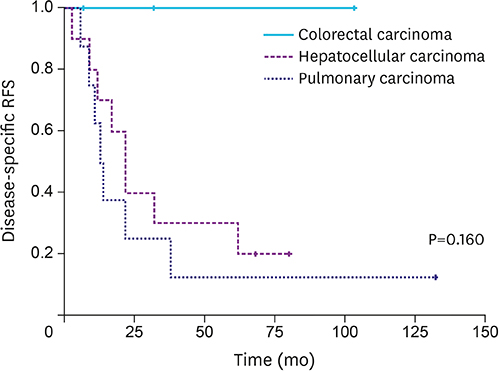
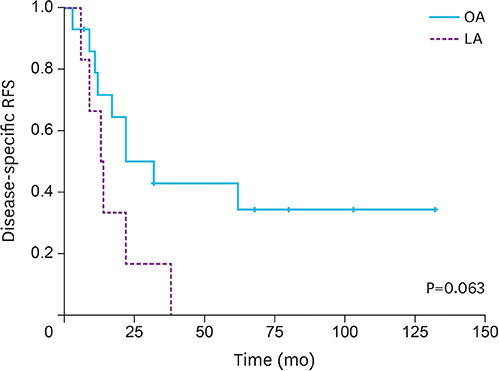
Our study cohort consisted of 21 patients with hepatocellular carcinoma (n=10), lung carcinoma (n=8), and colorectal carcinoma (n=3). The mean age was 54.6 years old. The mean overall survival (OS) duration was 78.5 months. Disease-specific recurrence-free survival (RFS) after metastatic adrenalectomy was significantly longer when the interval between primary carcinoma treatment and metachronous metastasis to the adrenal glands was ≥16 months (P=0.043). There was no significant difference in disease-specific RFS between patients who underwent open adrenalectomy (OA) vs. laparoscopic adrenalectomy (LA) (P=0.063).
CONCLUSION
Surgical treatment should be recommended for isolated metachronous adrenal gland metastases when the interval between primary carcinoma treatment and metastasis is ≥16 months to achieve better disease-specific RFS. LA was not inferior to OA.
MeSH Terms
Figure
Reference
-
1. Tomasini P, Garcia ME, Greillier L, Paladino C, Sebag F, Barlesi F. Adrenal surgery for oligometastatic tumors improves survival in selected cases. J Visc Surg. 2017; 154:87–91.
Article2. Marangos IP, Kazaryan AM, Rosseland AR, Røsok BI, Carlsen HS, Kromann-Andersen B, et al. Should we use laparoscopic adrenalectomy for metastases? Scandinavian multicenter study. J Surg Oncol. 2009; 100:43–47.
Article3. Solaini L, Ministrini S, Tomasoni M, Merigo G, Gaverini G, Bertoloni GP, et al. Adrenalectomy for metastasis: long-term results and predictors of survival. Endocrine. 2015; 50:187–192.
Article4. Kim SH, Brennan MF, Russo P, Burt ME, Coit DG. The role of surgery in the treatment of clinically isolated adrenal metastasis. Cancer. 1998; 82:389–394.
Article5. Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015; 136:E359–E386.
Article6. Castillo OA, Vitagliano G, Kerkebe M, Parma P, Pinto I, Diaz M. Laparoscopic adrenalectomy for suspected metastasis of adrenal glands: our experience. Urology. 2007; 69:637–641.
Article7. Herr K, Muglia VF, Koff WJ, Westphalen AC. Imaging of the adrenal gland lesions. Radiol Bras. 2014; 47:228–239.
Article8. Abdel-Raheem MM, Potti A, Becker WK, Saberi A, Scilley BS, Mehdi SA. Late adrenal metastasis in operable non-small-cell lung carcinoma. Am J Clin Oncol. 2002; 25:81–83.
Article9. Park JS, Yoon DS, Kim KS, Choi JS, Lee WJ, Chi HS, et al. What is the best treatment modality for adrenal metastasis from hepatocellular carcinoma? J Surg Oncol. 2007; 96:32–36.
Article10. Strong VE, D’Angelica M, Tang L, Prete F, Gönen M, Coit D, et al. Laparoscopic adrenalectomy for isolated adrenal metastasis. Ann Surg Oncol. 2007; 14:3392–3400.
Article11. Suzuki H. Laparoscopic adrenalectomy for adrenal carcinoma and metastases. Curr Opin Urol. 2006; 16:47–53.
Article12. Sarela AI, Murphy I, Coit DG, Conlon KC. Metastasis to the adrenal gland: the emerging role of laparoscopic surgery. Ann Surg Oncol. 2003; 10:1191–1196.
Article13. Porte H, Siat J, Guibert B, Lepimpec-Barthes F, Jancovici R, Bernard A, et al. Resection of adrenal metastases from non-small cell lung cancer: a multicenter study. Ann Thorac Surg. 2001; 71:981–985.
Article14. Tanvetyanon T, Robinson LA, Schell MJ, Strong VE, Kapoor R, Coit DG, et al. Outcomes of adrenalectomy for isolated synchronous versus metachronous adrenal metastases in non-small-cell lung cancer: a systematic review and pooled analysis. J Clin Oncol. 2008; 26:1142–1147.
Article15. Sebag F, Calzolari F, Harding J, Sierra M, Palazzo FF, Henry JF. Isolated adrenal metastasis: the role of laparoscopic surgery. World J Surg. 2006; 30:888–892.
Article16. Howell GM, Carty SE, Armstrong MJ, Stang MT, McCoy KL, Bartlett DL, et al. Outcome and prognostic factors after adrenalectomy for patients with distant adrenal metastasis. Ann Surg Oncol. 2013; 20:3491–3496.
Article17. Gagner M, Lacroix A, Bolté E. Laparoscopic adrenalectomy in Cushing's syndrome and pheochromocytoma. N Engl J Med. 1992; 327:1033.
Article18. Kebebew E, Siperstein AE, Clark OH, Duh QY. Results of laparoscopic adrenalectomy for suspected and unsuspected malignant adrenal neoplasms. Arch Surg. 2002; 137:948–951.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CT Differentiation of Adrenal Pheochromocytoma from Primary Carcinoma and Metastasis
- Metachronous Solitary Contralateral Adrenal Metastasis of Renal Cell Carcinoma
- Isolated Adrenal Injury after Blunt Abdominal Trauma without Visceral Organ Injury
- Computed tomography of adrenal tumor
- A Case of Metachronous Carcinosarcoma and Squamous Cell Carcinoma of the Both Parotid Glands