Ann Rehabil Med.
2017 Feb;41(1):90-96. 10.5535/arm.2017.41.1.90.
Efficacy of Intensive Neurodevelopmental Treatment for Children With Developmental Delay, With or Without Cerebral Palsy
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Dongguk University College of Medicine, Goyang, Korea. bskwon@dumc.or.kr
- KMID: 2383682
- DOI: http://doi.org/10.5535/arm.2017.41.1.90
Abstract
OBJECTIVE
To evaluate the effectiveness of intensive neurodevelopmental treatment (NDT) on gross motor function for the children having developmental delay (DD), with or without cerebral palsy (CP).
METHODS
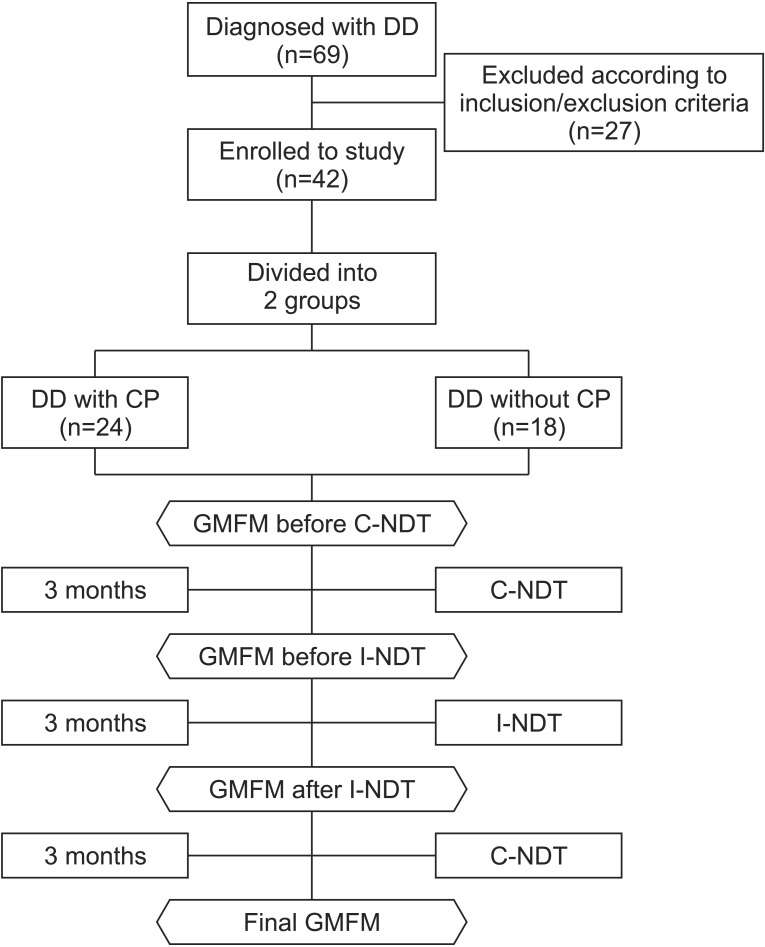
Forty-two children had intensive NDT three times weekly, 60 minutes a day, for 3 months, immediately followed by conventional NDT once or twice a week, 30 minutes a day, for another 3 months. We assessed Gross Motor Function Measure (GMFM) over three time points: before conventional NDT, before and after intensive NDT, and after 3 months of additional conventional NDT.
RESULTS
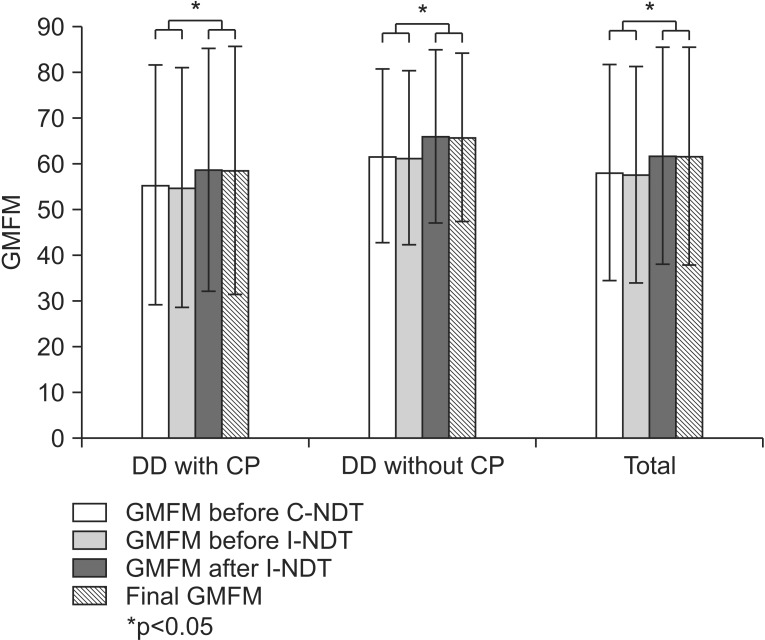
The GMFM score in DD children significantly improved after intensive NDT, and the improvement maintained after 3 months of conventional NDT (p<0.05). The children were further divided into two groups: DD with CP and DD without CP. Both groups showed significant improvement and maintained the improvements, after intensive NDT (p<0.05). Also, there was no significant difference in treatment efficacy between the two groups. When we calculate the absence rate for comparing the compliance between intensive and conventional NDT, the absence rate was lower during the intensive NDT.
CONCLUSION
Intensive NDT showed significantly improved gross motor function and higher compliance than conventional NDT. Additionally, all improvements were maintained through subsequent short-term conventional NDT. Thus, we recommend the intensive NDT program by day-hospital centers for children with DD, irrespective of accompanying CP.
MeSH Terms
Figure
Reference
-
1. Lim SY, Jung HY. Cerebral palsy: etiology and evaluation. In : Sung IY, editor. Pediatric rehabilitation. 2nd ed. Seoul: Koonja;2013. p. 367–382. .2. Sung IY, Shin YB, Park SS. Cerebral palsy: clinical features and management. In : Sung IY, editor. Pediatric rehabilitation. 2nd ed. Seoul: Koonja;2013. p. 383–418.3. Barry MJ. Physical therapy interventions for patients with movement disorders due to cerebral palsy. J Child Neurol. 1996; 11(Suppl 1):S51–S60. PMID: 8959462.
Article4. Molnar GE, Alexander MA. Pediatric rehabilitation. 3rd ed. Philadelphia: Hanley & Belfus;1999.5. Bobath B. A neuro-developmental treatment of cerebral palsy. Physiotherapy. 1963; 49:242–244. PMID: 14097882.6. Bobath B. Motor development, its effect on general development, and application to the treatment of cerebral palsy. Physiotherapy. 1971; 57:526–532. PMID: 5139032.7. Tsorlakis N, Evaggelinou C, Grouios G, Tsorbatzoudis C. Effect of intensive neurodevelopmental treatment in gross motor function of children with cerebral palsy. Dev Med Child Neurol. 2004; 46:740–745. PMID: 15540634.
Article8. Kim SJ, Lee CH, Na JK, Lee SH, Sung IY, Park BK. Current physical therapy status for the children with cerebral palsy in Korea. J Korean Acad Rehabil Med. 2000; 24:200–207.9. Ottenbacher KJ, Biocca Z, DeCremer G, Gevelinger M, Jedlovec KB, Johnson MB. Quantitative analysis of the effectiveness of pediatric therapy: emphasis on the neurodevelopmental treatment approach. Phys Ther. 1986; 66:1095–1101. PMID: 2941772.10. Jung HY. Functional assessment of pediatric disabilities. In : Sung IY, editor. Pediatric rehabilitation. 2nd ed. Seoul: Koonja;2013. p. 59–84.11. Blauw-Hospers CH, Hadders-Algra M. A systematic review of the effects of early intervention on motor development. Dev Med Child Neurol. 2005; 47:421–432. PMID: 15934492.
Article12. Siebes RC, Wijnroks L, Vermeer A. Qualitative analysis of therapeutic motor intervention programmes for children with cerebral palsy: an update. Dev Med Child Neurol. 2002; 44:593–603. PMID: 12227614.
Article13. Bower E, Michell D, Burnett M, Campbell MJ, McLellan DL. Randomized controlled trial of physiotherapy in 56 children with cerebral palsy followed for 18 months. Dev Med Child Neurol. 2001; 43:4–15. PMID: 11201422.
Article14. Trahan J, Malouin F. Intermittent intensive physiotherapy in children with cerebral palsy: a pilot study. Dev Med Child Neurol. 2002; 44:233–239. PMID: 11995891.
Article15. Rahlin M. An individualized intermittent intensive physical therapy schedule for a child with spastic quadriparesis. Physiother Theory Pract. 2011; 27:512–520. PMID: 21568817.
Article16. Shamir M, Dickstein R, Tirosh E. Intensive intermittent physical therapy in infants with cerebral palsy: a randomized controlled pilot study. Isr Med Assoc J. 2012; 14:737–741. PMID: 23393711.17. Palisano RJ, Hanna SE, Rosenbaum PL, Russell DJ, Walter SD, Wood EP, et al. Validation of a model of gross motor function for children with cerebral palsy. Phys Ther. 2000; 80:974–985. PMID: 11002433.
Article18. Palisano RJ, Walter SD, Russell DJ, Rosenbaum PL, Gemus M, Galuppi BE, et al. Gross motor function of children with down syndrome: creation of motor growth curves. Arch Phys Med Rehabil. 2001; 82:494–500. PMID: 11295010.
Article19. Russell DJ, Avery LM, Rosenbaum PL, Raina PS, Walter SD, Palisano RJ. Improved scaling of the gross motor function measure for children with cerebral palsy: evidence of reliability and validity. Phys Ther. 2000; 80:873–885. PMID: 10960935.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Developmental Delay of Language in Cerebral Palsy Children
- Neurodevelopmental Outcome in Children Born after in vitro Fertilization
- Neurodevelopmental Outcomes of Very Low Birth Weight Infants
- Correlation of brain CT findings and developmental outcome in patients with spastic cerebral palsy
- The Diagnostic Significance of Clinical Characteristics and Neuroimaging Findings for Diagnosis of Children with Developmental Delay