Clin Endosc.
2017 Mar;50(2):191-196. 10.5946/ce.2016.093.
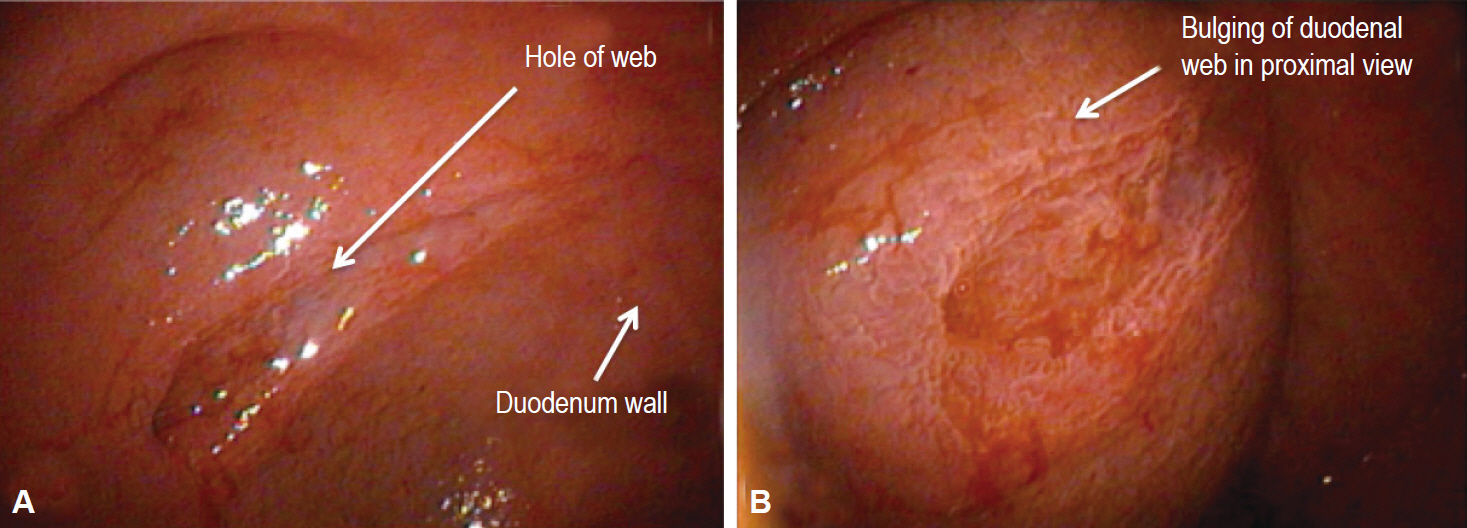
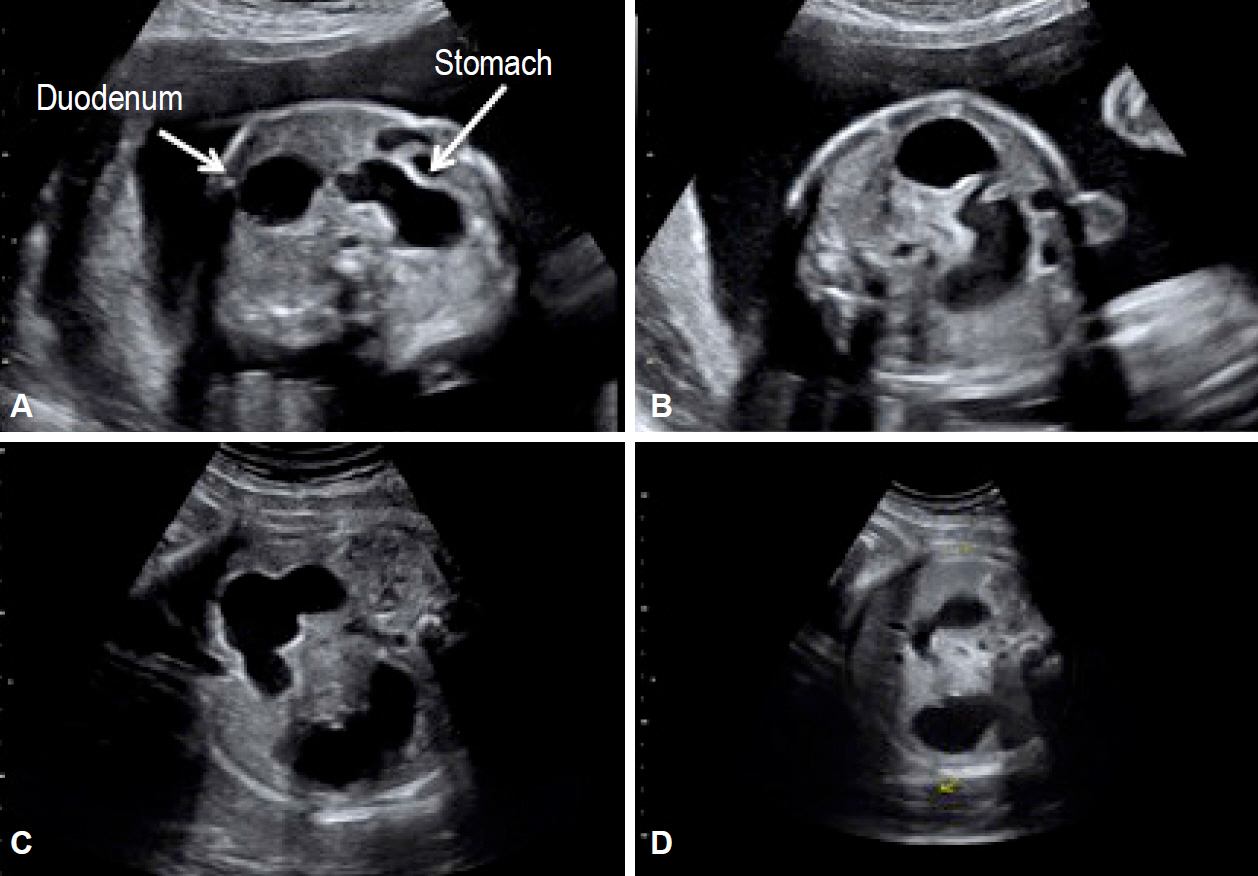
Persistent Nonbilious Vomiting in a Child: Possible Duodenal Webbing
- Affiliations
-
- 1Division of Pediatric Surgery, Department of Medical, Surgical and Neurological Sciences, University of Siena, Siena, Italy. rossellaangotti@me.com
- 2Pediatric Surgery Unit, Academic Salesi Children Hospital, Marche Polytechnic University, Ancona, Italy.
- 3Section of Obstetrics and Gynecology, Department of Molecular and Developmental Medicine, University of Siena, Siena, Italy.
- KMID: 2383537
- DOI: http://doi.org/10.5946/ce.2016.093
Abstract
- An association between malrotation and congenital duodenal webbing is rare. We present our experience with four patients at two centers, and a review of published reports. There are currently 94 reported cases of duodenal pathology associated with malrotation. However, only 15 of the 94 cases (15.9%) include patients with malrotation and a duodenal web. We suggest that nonbilious vomiting in a child must prompt the surgeon to consider duodenal pathology even in the presence of malrotation.
Figure
Reference
-
1. Ingoe R, Lange P. The Ladd’s procedure for correction of intestinal malrotation with volvulus in children. AORN J. 2007; 85:300–308.2. Angotti R, Bulotta AL, Ferrara F, et al. Uncommon surgical emergencies in neonatology. Pediatr Med Chir. 2014; 36:99.
Article3. Beeks A, Gosche J, Giles H, Nowicki M. Endoscopic dilation and partial resection of a duodenal web in an infant. J Pediatr Gastroenterol Nutr. 2009; 48:378–381.
Article4. Sweed Y. Duodenal obstruction. In : Puri P, Höllwarth ME, editors. Pediatric Surgery: Diagnosis and Management. London: Springer;2009. p. 383–392.5. Lampl B, Levin TL, Berdon WE, Cowles RA. Malrotation and midgut volvulus: a historical review and current controversies in diagnosis and management. Pediatr Radiol. 2009; 39:359–366.
Article6. Penco JM, Murillo JC, Hernández A, De La Calle Pato U, Masjoan DF, Aceituno FR. Anomalies of intestinal rotation and fixation: consequences of late diagnosis beyond two years of age. Pediatr Surg Int. 2007; 23:723–730.
Article7. Yoon CH, Goo HW, Kim EA, Kim KS, Pi SY. Sonographic windsock sign of a duodenal web. Pediatr Radiol. 2001; 31:856–857.
Article8. Madding GF, Everhart MW, Heath J. Congenital duodenal atresia with malrotation of the intestine; a case successfully treated by duodeno-jejunostomy. Ann Surg. 1950; 131:433–436.9. Baumgartner F, Moore TC. Atretic, obstructive proximal duodenal mass associated with annular pancreas and malrotation in a newborn male. Eur J Pediatr Surg. 1992; 2:42–44.
Article10. Barrack SM, Kyambi JM, Ndungu J, Wachira N, Anangwe G, Safwat S. Intestinal atresia and stenosis as seen and treated at Kenyatta National Hospital, Nairobi. East Afr Med J. 1993; 70:558–564.11. Zerin JM, Polley TZ Jr. Malrotation in patients with duodenal atresia: a true association or an expected finding on postoperative upper gastrointestinal barium study? Pediatr Radiol. 1994; 24:170–172.
Article12. Samuel M, Wheeler RA, Mami AG. Does duodenal atresia and stenosis prevent midgut volvulus in malrotation? Eur J Pediatr Surg. 1997; 7:11–12.
Article13. Dalla Vecchia LK, Grosfeld JL, West KW, Rescorla FJ, Scherer LR, Engum SA. Intestinal atresia and stenosis: a 25-year experience with 277 cases. Arch Surg. 1998; 133:490–496.14. Chandran H, Upadhyay V, Pease PW. Multiple organ malrotation syndrome with duodenal atresia: a case report. Pediatr Surg Int. 1999; 15:61–62.
Article15. Pumberger W, Birnbacher R, Pomberger G, Deutinger J. Duodeno-jejunal atresia with volvulus, absent dorsal mesentery, and absent superior mesenteric artery: a hereditary compound structure in duodenal atresia? Am J Med Genet. 2002; 109:52–55.
Article16. Glüer S, Petersen C, Ure BM. Simultaneous correction of duodenal atresia due to annular pancreas and malrotation by laparoscopy. Eur J Pediatr Surg. 2002; 12:423–425.
Article17. Aslanabadi S, Ghalehgolab-Behbahan A, Jamshidi M, Veisi P, Zarrintan S. Intestinal malrotations: a review and report of thirty cases. Folia Morphol (Warsz). 2007; 66:277–282.18. Morikawa N, Kuroda T, Honna T, et al. A novel association of duodenal atresia, malrotation, segmental dilatation of the colon, and anorectal malformation. Pediatr Surg Int. 2009; 25:1003–1005.
Article19. Patil RT, Gupta R, Parelkar SV, et al. A rare case of duodenal atresia with apple-peel configuration of the small intestine and malrotation. Eur J Pediatr Surg. 2011; 21:340–342.
Article20. Eksarko P, Nazir S, Kessler E, et al. Duodenal web associated with malrotation and review of literature. J Surg Case Rep. 2013; 2013.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Diagnosis of Duodenal Stenosis in a 5-Month-Old Male Infant
- A Case of Duodenal Web Associated with Intestinal Malrotation
- Duodenal Obstruction due to Duodenal Web in Three-year-old Girl: A Case Report
- Heterotopic Pancreas Presented as Duodenal Tumor with Obstruction
- Congenital Duodenal Web Associated with a Foreign Body (Go Stone) in a 10-Year-Old Girl