Clin Endosc.
2017 Mar;50(2):185-190. 10.5946/ce.2016.030.
Endoscopic Ultrasound (EUS)-Directed Transgastric Endoscopic Retrograde Cholangiopancreatography or EUS: Mid-Term Analysis of an Emerging Procedure
- Affiliations
-
- 1Division of Gastroenterology and Hepatology, Weill Cornell Medical Center, New York, NY, USA. mkahaleh@gmail.com
- 2Division of Gastroenterology and Hepatology, Borland-Groover Clinic (BGC), Jacksonville, FL, USA.
- 3Interventional Endoscopy, Methodist Dallas Medical Center, Dallas, TX, USA.
- KMID: 2383536
- DOI: http://doi.org/10.5946/ce.2016.030
Abstract
- BACKGROUND/AIMS
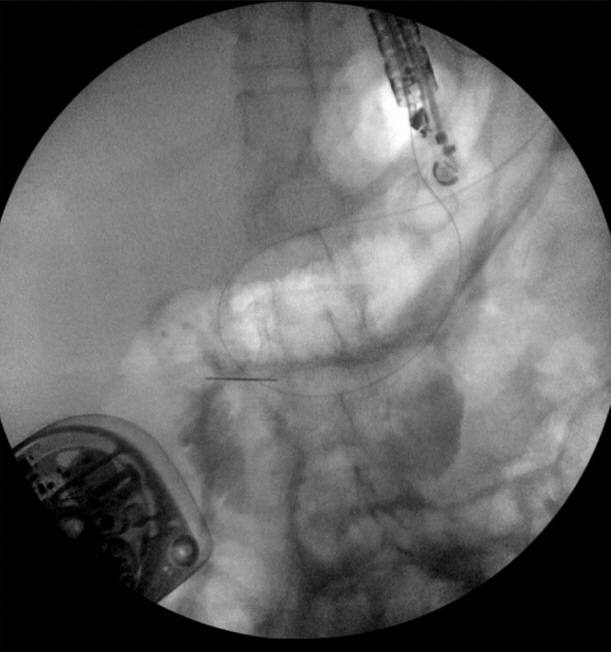
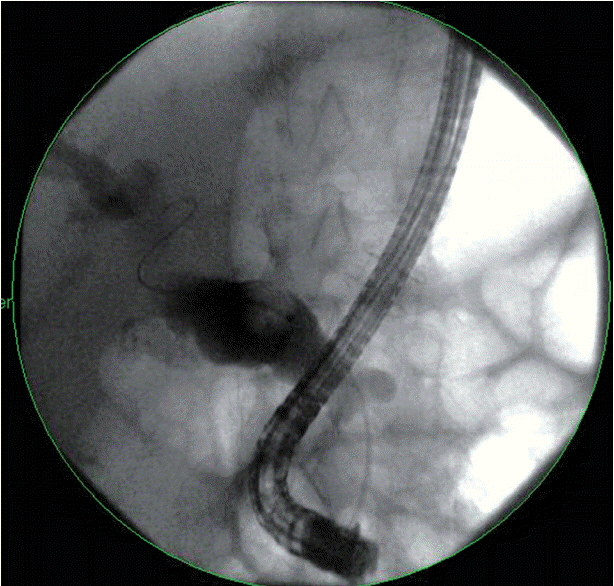
Performing endoscopic retrograde cholangiopancreatography (ERCP) in patients who have undergone Rouxen-Y gastric bypass (RYGB) is challenging. Standard ERCP and enteroscopy-assisted ERCP are associated with limited success rates. Laparoscopy- or laparotomy-assisted ERCP yields improved efficacy rates, but with higher complication rates and costs. We present the first multicenter experience regarding the efficacy and safety of endoscopic ultrasound (EUS)-directed transgastric ERCP (EDGE) or EUS.
METHODS
All patients who underwent EDGE at two academic centers were included. Clinical success was defined as successful ERCP and/or EUS through the use of lumen-apposing metal stents (LAMS). Adverse events related to EDGE were separated from ERCP- or EUS-related complications and were defined as bleeding, stent migration, perforation, and infection.
RESULTS
Sixteen patients were included in the study. Technical success was 100%. Clinical success was 90% (n=10); five patients were awaiting maturation of the fistula tract prior to ERCP or EUS, and one patient had an aborted ERCP due to perforation. One perforation occurred, which was managed endoscopically. Three patients experienced stent dislodgement; all stents were successfully repositioned or bridged with a second stent. Ten patients (62.5%) had their LAMS removed. The average weight change from LAMS insertion to removal was negative 2.85 kg.
CONCLUSIONS
EDGE is an effective, minimally invasive, single-team solution to the difficulties associated with ERCP in patients with RYGB.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Commentary on “Endoscopic Ultrasound (EUS)-Directed Transgastric Endoscopic Retrograde Cholangiopancreatography or EUS”
Se Woo Park
Clin Endosc. 2017;50(2):102-103. doi: 10.5946/ce.2017.033.
Reference
-
1. Buchwald H, Williams SE. Bariatric surgery worldwide 2003. Obes Surg. 2004; 14:1157–1164.
Article2. Buchwald H, Oien DM. Metabolic/bariatric surgery Worldwide 2008. Obes Surg. 2009; 19:1605–1611.
Article3. Ribaric G, Buchwald JN, McGlennon TW. Diabetes and weight in comparative studies of bariatric surgery vs conventional medical therapy: a systematic review and meta-analysis. Obes Surg. 2014; 24:437–455.
Article4. Ikramuddin S, Korner J, Lee WJ, et al. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA. 2013; 309:2240–2249.5. Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007; 357:741–752.
Article6. Sjöström L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004; 351:2683–2693.
Article7. Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013; 23:427–436.
Article8. Hintze RE, Adler A, Veltzke W, Abou-Rebyeh H. Endoscopic access to the papilla of Vater for endoscopic retrograde cholangiopancreatography in patients with billroth II or Roux-en-Y gastrojejunostomy. Endoscopy. 1997; 29:69–73.
Article9. Elton E, Hanson BL, Qaseem T, Howell DA. Diagnostic and therapeutic ERCP using an enteroscope and a pediatric colonoscope in long-limb surgical bypass patients. Gastrointest Endosc. 1998; 47:62–67.
Article10. Skinner M, Popa D, Neumann H, Wilcox CM, Mönkemüller K. ERCP with the overtube-assisted enteroscopy technique: a systematic review. Endoscopy. 2014; 46:560–572.
Article11. Lopes TL, Clements RH, Wilcox CM. Laparoscopy-assisted ERCP: experience of a high-volume bariatric surgery center (with video). Gastrointest Endosc. 2009; 70:1254–1259.
Article12. Gutierrez JM, Lederer H, Krook JC, Kinney TP, Freeman ML, Jensen EH. Surgical gastrostomy for pancreatobiliary and duodenal access following Roux en Y gastric bypass. J Gastrointest Surg. 2009; 13:2170–2175.
Article13. Saleem A, Levy MJ, Petersen BT, Que FG, Baron TH. Laparoscopic assisted ERCP in Roux-en-Y gastric bypass (RYGB) surgery patients. J Gastrointest Surg. 2012; 16:203–208.
Article14. Schreiner MA, Chang L, Gluck M, et al. Laparoscopy-assisted versus balloon enteroscopy-assisted ERCP in bariatric post-Roux-en-Y gastric bypass patients. Gastrointest Endosc. 2012; 75:748–756.
Article15. Shah RJ, Smolkin M, Yen R, et al. A multicenter, U.S. experience of single-balloon, double-balloon, and rotational overtube-assisted enteroscopy ERCP in patients with surgically altered pancreaticobiliary anatomy (with video). Gastrointest Endosc. 2013; 77:593–600.
Article16. Choi EK, Chiorean MV, Coté GA, et al. ERCP via gastrostomy vs. double balloon enteroscopy in patients with prior bariatric Roux-en-Y gastric bypass surgery. Surg Endosc. 2013; 27:2894–2899.
Article17. Kedia P, Sharaiha RZ, Kumta NA, Kahaleh M. Internal EUS-directed transgastric ERCP (EDGE): game over. Gastroenterology. 2014; 147:566–568.
Article18. Kedia P, Tyberg A, Kumta NA, et al. EUS-directed transgastric ERCP for Roux-en-Y gastric bypass anatomy: a minimally invasive approach. Gastrointest Endosc. 2015; 82:560–565.
Article19. Law R, Wong Kee Song LM, Petersen BT, Baron TH. Single-session ERCP in patients with previous Roux-en-Y gastric bypass using percutaneous-assisted transprosthetic endoscopic therapy: a case series. Endoscopy. 2013; 45:671–675.
Article20. Attam R, Leslie D, Freeman M, Ikramuddin S, Andrade R. EUS-assisted, fluoroscopically guided gastrostomy tube placement in patients with Roux-en-Y gastric bypass: a novel technique for access to the gastric remnant. Gastrointest Endosc. 2011; 74:677–682.
Article21. Tekola B, Wang AY, Ramanath M, et al. Percutaneous gastrostomy tube placement to perform transgastrostomy endoscopic retrograde cholangiopancreaticography in patients with Roux-en-Y anatomy. Dig Dis Sci. 2011; 56:3364–3369.
Article22. Kedia P, Kumta NA, Widmer J, et al. Endoscopic ultrasound-directed transgastric ERCP (EDGE) for Roux-en-Y anatomy: a novel technique. Endoscopy. 2015; 47:159–163.
Article23. Kedia P, Kumta NA, Sharaiha R, Kahaleh M. Bypassing the bypass: EUS-directed transgastric ERCP for Roux-en-Y anatomy. Gastrointest Endosc. 2015; 81:223–224.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Commentary on “Endoscopic Ultrasound (EUS)-Directed Transgastric Endoscopic Retrograde Cholangiopancreatography or EUSâ€
- Endoscopic ultrasound-guided biliary drainage in malignant distal biliary obstruction
- Endoscopic Ultrasound-Guided Hepaticogastrostomy: Technical Review and Tips to Prevent Adverse Events
- Successful endoscopic closure of an esophageal leak after endoscopic ultrasound-guided hepaticoesophagostomy by using n-butyl-2 cyanoacrylate
- Role of Repeated Endoscopic Ultrasound-Guided Fine Needle Aspiration for Inconclusive Initial Cytology Result