Korean J Gastroenterol.
2016 Oct;68(4):202-209. 10.4166/kjg.2016.68.4.202.
The Usefulness of Early Endoscopic Ultrasonography in Acute Biliary Pancreatitis with Undetectable Choledocholithiasis on Multidetector Computed Tomography
- Affiliations
-
- 1Department of Internal Medicine, Chungbuk National University College of Medicine, Cheongju, Korea. smpark@chungbuk.ac.kr
- KMID: 2383516
- DOI: http://doi.org/10.4166/kjg.2016.68.4.202
Abstract
- BACKGROUND/AIMS
EUS can detect bile duct stones (BDS) that are undetectable on multidetector computed tomography (MDCT). BDS associated with acute biliary pancreatitis (ABP) are small and tend to be excreted spontaneously. This study evaluated the usefulness of early EUS in patients with ABP and undetectable BDS on MDCT.
METHODS
Forty-one patients with ABP and undetectable BDS on MDCT underwent EUS within 24 hours of admission and were diagnosed with BDS, sludge, dilated common bile duct (CBD), or normal CBD. ERCP was performed in patients with BDS, sludge, or clinical deterioration. The diagnostic yield and the effects of early EUS on morbidity, mortality, and the length of hospitalization were evaluated.
RESULTS
EUS detected BDS or sludge in 48.8% of patients examined. BDS was the diagnosis in 13 patients, sludge in seven, and neither for 21 patients. ERCP was performed in 20 patients with BDS or sludge, in two patients with coexisting cholangitis, and in one patient with worsening liver function tests. ERCP identified BDS in 12 patients and sludge in seven. No lesions were diagnosed in four patients by ERCP. All patients improved, and the length of hospitalization in patients with ERCP was 9.0 days, without ERCP 7.1 days. Two patients with major complications by ERCP were hospitalized for a prolonged time.
CONCLUSIONS
Early EUS may be useful to select patients for therapeutic ERCP in cases of suspected ABP with undetectable BDS on MDCT.
MeSH Terms
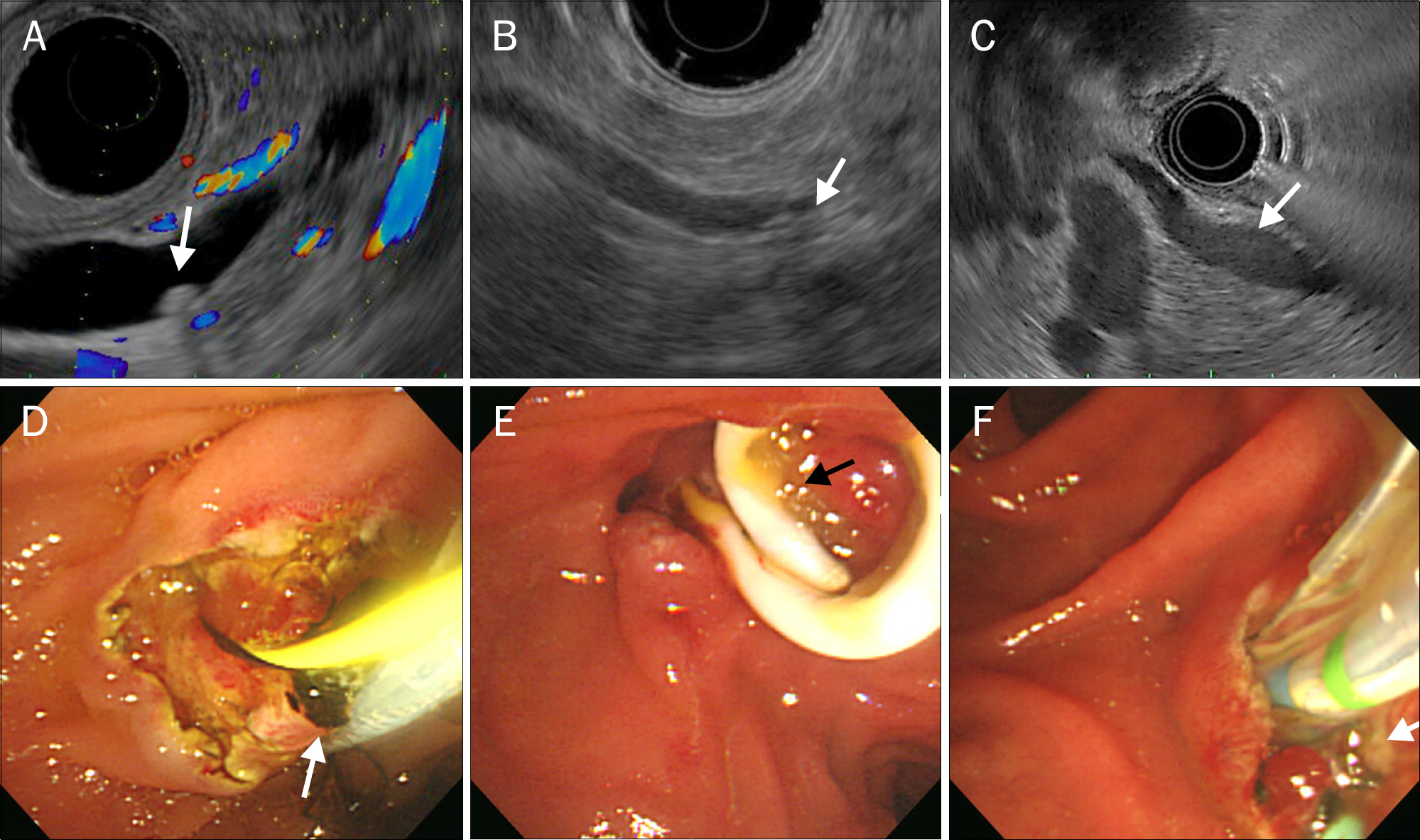
Figure
Reference
-
References
1. Attasaranya S, Fogel EL, Lehman GA. Choledocholithiasis, ascending cholangitis, and gallstone pancreatitis. Med Clin North Am. 2008; 92:925–960.
Article2. Anderson SW, Lucey BC, Varghese JC, Soto JA. Accuracy of MDCT in the diagnosis of choledocholithiasis. AJR Am J Roentgenol. 2006; 187:174–180.
Article3. Sgouros SN, Bergele C. Endoscopic ultrasonography versus other diagnostic modalities in the diagnosis of choledocholithiasis. Dig Dis Sci. 2006; 51:2280–2286.
Article4. Fogel EL, Sherman S. ERCP for gallstone pancreatitis. N Engl J Med. 2014; 370:150–157.
Article5. Liu CL, Lo CM, Chan JK, et al. Detection of choledocholithiasis by EUS in acute pancreatitis: a prospective evaluation in 100 consecutive patients. Gastrointest Endosc. 2001; 54:325–330.
Article6. Chak A, Hawes RH, Cooper GS, et al. Prospective assessment of the utility of EUS in the evaluation of gallstone pancreatitis. Gastrointest Endosc. 1999; 49:599–604.
Article7. Prat F, Edery J, Meduri B, et al. Early EUS of the bile duct before endoscopic sphincterotomy for acute biliary pancreatitis. Gastrointest Endosc. 2001; 54:724–729.
Article8. Arguedas MR, Dupont AW, Wilcox CM. Where do ERCP, endoscopic ultrasound, magnetic resonance cholangiopancreatography, and intraoperative cholangiography fit in the management of acute biliary pancreatitis? A decision analysis model. Am J Gastroenterol. 2001; 96:2892–2899.
Article9. Adams MA, Hosmer AE, Wamsteker EJ, et al. Predicting the likelihood of a persistent bile duct stone in patients with suspected choledocholithiasis: accuracy of existing guidelines and the impact of laboratory trends. Gastrointest Endosc. 2015; 82:88–93.
Article10. Anderloni A, Galeazzi M, Ballarè M, et al. Early endoscopic ultrasonography in acute biliary pancreatitis: a prospective pilot study. World J Gastroenterol. 2015; 21:10427–10434.
Article11. Liu CL, Fan ST, Lo CM, et al. Comparison of early endoscopic ultrasonography and endoscopic retrograde cholangiopancreatography in the management of acute biliary pancreatitis: a prospective randomized study. Clin Gastroenterol Hepatol. 2005; 3:1238–1244.
Article12. Cavdar F, Yildar M, Tellioğ lu G, Kara M, Tilki M, Titiz Mİ. Controversial issues in biliary pancreatitis: when should we perform MRCP and ERCP? Pancreatology. 2014; 14:411–414.
Article13. Goodman AJ, Neoptolemos JP, Carr-Locke DL, Finlay DB, Fossard DP. Detection of gall stones after acute pancreatitis. Gut. 1985; 26:125–132.
Article14. Leung TK, Lee CM, Lin SY, et al. Balthazar computed tomography severity index is superior to Ranson criteria and APACHE II scoring system in predicting acute pancreatitis outcome. World J Gastroenterol. 2005; 11:6049–6052.
Article15. Andari R, Modiri A, Makipour K. Endoscopic ultrasound should be performed before endoscopic retrograde cholangiopancreatography in all patients with mild acute gallstone pancreatitis. Pancreas. 2014; 43:147–148.
Article16. Bergele C, Giovannini M. EUS and common bile duct stones. Ann Gastroenterol. 2004; 17:246–252.17. Giljaca V, Gurusamy KS, Takwoingi Y, et al. Endoscopic ultrasound versus magnetic resonance cholangiopancreatography for common bile duct stones. Cochrane Database Syst Rev. 2015; (2):CD011549.
Article18. Shapiro T, Melzer E, Binder Y, et al. Selective utilization of preoperative endoscopic ultrasound to exclude choledocholithiasis prior to laparoscopic cholecystectomy: a retrospective study. Hepatogastroenterology. 2013; 60:456–460.19. De Lisi S, Leandro G, Buscarini E. Endoscopic ultrasonography versus endoscopic retrograde cholangiopancreatography in acute biliary pancreatitis: a systematic review. Eur J Gastroenterol Hepatol. 2011; 23:367–374.20. Tranter SE, Thompson MH. Spontaneous passage of bile duct stones: frequency of occurrence and relation to clinical presentation. Ann R Coll Surg Engl. 2003; 85:174–177.
Article21. Kohut M, Nowak A, Nowakowska-Duiawa E, Marek T. Presence and density of common bile duct microlithiasis in acute biliary pancreatitis. World J Gastroenterol. 2002; 8:558–561.
Article22. Fabbri C, Polifemo AM, Luigiano C, et al. Single session versus separate session endoscopic ultrasonography plus endoscopic retrograde cholangiography in patients with low to moderate risk for choledocholithiasis. J Gastroenterol Hepatol. 2009; 24:1107–1112.
Article23. Fan ST, Lai EC, Mok FP, Lo CM, Zheng SS, Wong J. Early treatment of acute biliary pancreatitis by endoscopic papillotomy. N Engl J Med. 1993; 328:228–232.
Article24. Tse F, Yuan Y. Early routine endoscopic retrograde cholangiopancreatography strategy versus early conservative management strategy in acute gallstone pancreatitis. Cochrane Database Syst Rev. 2012; (5):CD009779.
Article25. Petrov MS, van Santvoort HC, Besselink MG, van der Heijden GJ, van Erpecum KJ, Gooszen HG. Early endoscopic retrograde cholangiopancreatography versus conservative management in acute biliary pancreatitis without cholangitis: a metaanalysis of randomized trials. Ann Surg. 2008; 247:250–257.26. Moretti A, Papi C, Aratari A, et al. Is early endoscopic retrograde cholangiopancreatography useful in the management of acute biliary pancreatitis? A metaanalysis of randomized controlled trials. Dig Liver Dis. 2008; 40:379–385.27. Keizman D, Ish-Shalom M, Konikoff FM. The clinical significance of bile duct sludge: is it different from bile duct stones? Surg Endosc. 2007; 21:769–773.
Article28. Ney MV, Maluf-Filho F, Sakai P, Zilberstein B, Gama-Rodrigues J, Rosa H. Echo-endoscopy versus endoscopic retrograde cholangiography for the diagnosis of choledocholithiasis: the influence of the size of the stone and diameter of the common bile duct. Arq Gastroenterol. 2005; 42:239–243.29. Tenner S, Dubner H, Steinberg W. Predicting gallstone pancreatitis with laboratory parameters: a metaanalysis. Am J Gastroenterol. 1994; 89:1863–1836.30. Ş urlin V, Săftoiu A, Dumitrescu D. Imaging tests for accurate diagnosis of acute biliary pancreatitis. World J Gastroenterol. 2014; 20:16544–16549.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Biliary Ascariasis with Choledocholithiasis and Biliary Pancreatitis: Endoscopically Treated
- Biliary Tract & Pancreas; Effectiveness of Endoscopic Ultrasonography in Detecting the Extrahepatic Choledocholithiasis
- Effective Removal Methods for Common Bile Duct Stones
- Diagnosis of gallstone
- Indications and Timing of ERCP and Cholecystectomy for Biliary Pancreatitis