Korean J Gastroenterol.
2016 Nov;68(5):279-283. 10.4166/kjg.2016.68.5.279.
Traumatic Neuroma at the Inferior Mesenteric Artery Stump after Rectal Cancer Surgery: A Case Report and Literature Review
- Affiliations
-
- 1Department of Education and Training, Seoul National University Hospital, Seoul, Korea.
- 2Department of Radiology, Seoul National University Hospital, Seoul, Korea. leejy4u@snu.ac.kr
- 3Department of Pathology, Asan Medical Center, Seoul, Korea.
- KMID: 2383507
- DOI: http://doi.org/10.4166/kjg.2016.68.5.279
Abstract
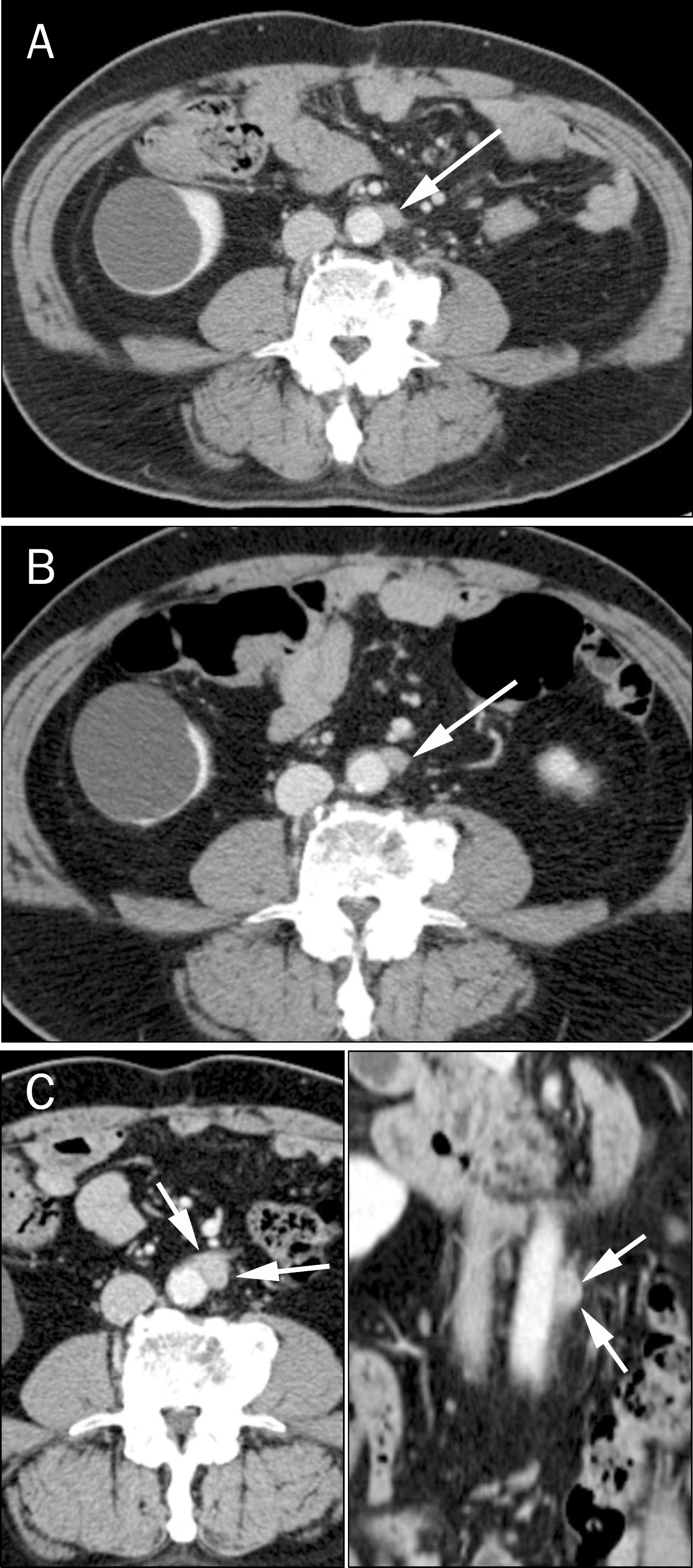
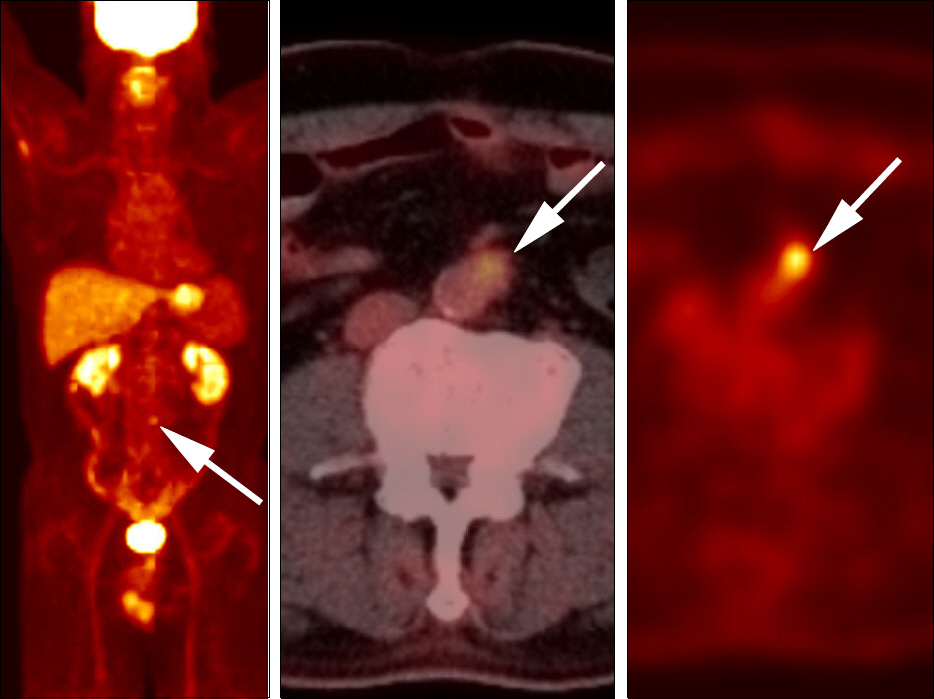
- Traumatic neuroma results from regeneration attempts of the proximal end of an injured or severed nerve, resulting in a non-neoplastic nodular lesion. The lower extremity after amputation is the most common site, followed by the head and neck. Traumatic neuromas occurring in the abdomen, however, are rare. In the abdominal region, traumatic neuromas occur in the cystic duct stump and the common bile ducts as well as around the celiac trunk. This study reports a case of a 59-year-old man who presented with a traumatic neuroma arising at the stump of the inferior mesenteric artery after rectal cancer surgery. Traumatic neuromas at the stump of the inferior mesenteric artery have not been previously reported. The lesion exhibited atypical imaging features, including a well-enhanced nodule, a significant interval growth in size and a mild increase in 18F-fluorodeoxyglucose uptake, resembling lymph node metastasis. This case report will help physicians understand the sites of occurrence and imaging features of traumatic neuromas in the abdomen.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Huang LF, Weissman JL, Fan C. Traumatic neuroma after neck dissection: CT characteristics in four cases. AJNR Am J Neuroradiol. 2000; 21:1676–1680.2. Yabuuchi H, Kuroiwa T, Fukuya T, Tomita K, Hachitanda Y. Traumatic neuroma and recurrent lymphadenopathy after neck dissection: comparison of radiologic features. Radiology. 2004; 233:523–529.
Article3. Boutin RD, Pathria MN, Resnick D. Disorders in the stumps of amputee patients: MR imaging. AJR Am J Roentgenol. 1998; 171:497–501.
Article4. Brogan DM, Kakar S. Management of neuromas of the upper extremity. Hand Clin. 2013; 29:409–420.
Article5. Swanson HH. Traumatic neuromas. A review of the literature. Oral Surg Oral Med Oral Pathol. 1961; 14:317–326.6. Murphey MD, Smith WS, Smith SE, Kransdorf MJ, Temple HT. From the archives of the AFIP. Imaging of musculoskeletal neurogenic tumors: radiologic-pathologic correlation. Radiographics. 1999; 19:1253–1280.7. Nagata Y, Tomioka T, Chiba K, Kanematsu T. Traumatic neuroma of the common hepatic duct after laparoscopic cholecystectomy. Am J Gastroenterol. 1995; 90:1887–1888.8. Koh DW, Lee WJ, Kim JH, et al. Amputation neuroma mimicking common bile duct cancer: a case report. Korean J Gastroenterol. 2008; 52:32–36.9. Shimura K, Tamada K, Asada M, et al. Intraductal ultrasonography of traumatic neuroma of the bile duct. Abdom Imaging. 2001; 26:632–634.
Article10. van Gulik TM, Brummelkamp WH, Lygidakis NJ. Traumatic neuroma giving rise to biliary obstruction after reconstructive surgery for iatrogenic lesions of the biliary tract–a report of three cases. Hepatogastroenterology. 1989; 36:255–257.11. Mentha G, Rubbia-Brandt L, Orci L, et al. Traumatic neuroma with biliary duct obstruction after orthotopic liver transplantation. Transplantation. 1999; 67:177–179.
Article12. Katsinelos P, Dimiropoulos S, Galanis I, et al. Biliary stricture due to neuroma after an innocent blunt abdominal trauma. Surg Endosc. 2002; 16:1494.
Article13. Kwon JH, Ryu SW, Kang YN. Traumatic neuroma around the celiac trunk after gastrectomy mimicking a nodal metastasis: a case report. Korean J Radiol. 2007; 8:242–245.
Article14. Curran T, Poylin V, Kane R, Harris A, Goldsmith JD, Nagle D. Case report of a traumatic rectal neuroma. Gastroenterol Rep (Oxf). 2015. DOI: doi:10.1093/gastro/gov023.
Article15. Ahlawat S, Belzberg AJ, Montgomery EA, Fayad LM. MRI features of peripheral traumatic neuromas. Eur Radiol. 2016; 26:1204–1212.
Article16. Chang JM, Lee HJ, Goo JM, et al. False positive and false negative FDG-PET scans in various thoracic diseases. Korean J Radiol. 2006; 7:57–69.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Traumatic Neuroma in Breast Cancer Patient after Mastectomy: A Case Report
- Inferior Mesenteric Artery Embolization with N-Butyl Cyanoacrylate for Life-Threatening Postpartum Hemorrhage: A Report of Two Cases and Literature Review
- A Case of Traumatic Neuroma in Infraorbital Nerve
- A Case of the Inferior Mesenteric Artery Arising from the Superior Mesenteric Artery in a Korean Woman
- Idiopathic Inferior Mesenteric Arteriovenous Fistula with Ischemic Colitis: A Case Report and Literature Review