Korean J Gastroenterol.
2017 May;69(5):308-311. 10.4166/kjg.2017.69.5.308.
A Case of Tuberculous Peritonitis Presenting as Small Bowel Obstruction
- Affiliations
-
- 1Department of Internal Medicine, Kosin University College of Medicine, Busan, Korea. solefide@hanmail.net
- KMID: 2383389
- DOI: http://doi.org/10.4166/kjg.2017.69.5.308
Abstract
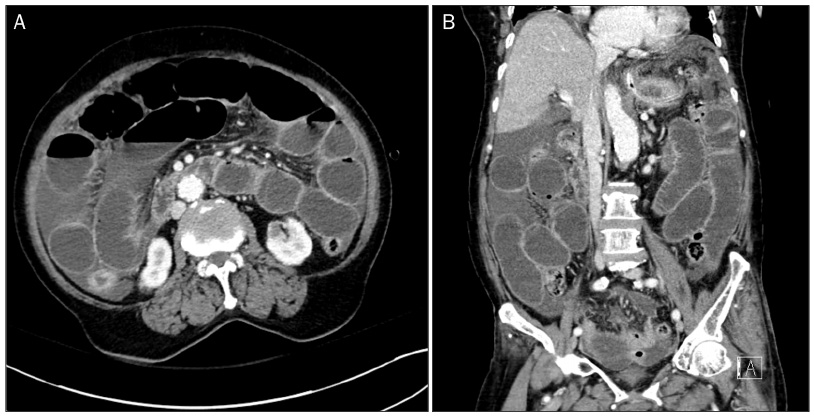
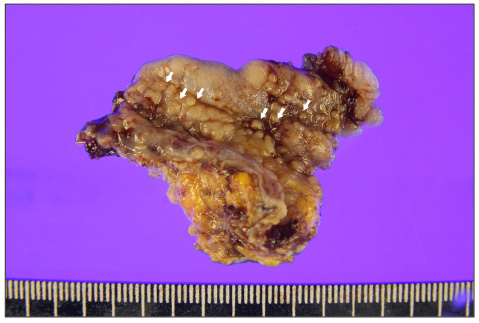
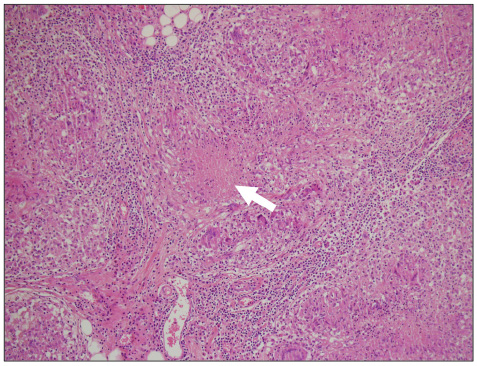
- The peritoneum is one of the common extrapulmonary sites of tuberculosis infection. Patients with underlying end-stage renal or liver disease are frequently complicated by tuberculous peritonitis; however, the diagnosis of the tuberculous peritonitis is difficult due to its insidious nature, well as its variability in presentation and limitation of available diagnostic tests. Once diagnosed, the preferred treatment is usually antituberculous therapy in uncomplicated cases. However, surgical treatment may also be required for complicated cases, such as small bowel obstruction or perforation. An 85-year-old woman was referred our hospital for abdominal pain with ileus. Despite medical therapy, prolonged ileus and progression to sepsis were shown, she underwent surgery to confirm the diagnosis and relief of mechanical ileus. Intraoperative peritoneal biopsy and macroscopic findings confirmed tuberculous peritonitis. Therefore, physicians should consider the possibility of tuberculous peritonitis in patients with unexplained small bowel obstruction.
MeSH Terms
Figure
Reference
-
1. Mehta JB, Dult A, Harvill L, Mathews KM. Epidemiology of extrapulmonary tuberculosis: a comparative analysis with pre-AIDS era. Chest. 1991; 99:1134–1138.2. Sanai FM, Bzeizi KI. Systemic review: tuberculous peritonitis--presenting features, diagnostic strategies and treatment. Aliment Pharmacol Ther. 2005; 22:685–700.3. Palmer KR, Patil DH, Basran GS, Riordan JF, Silk BD. Abdominal tuberculosis in urban Britain--a common disease. Gut. 1985; 26:1296–1305.4. Tang LC, Cho HK, Wong Taam VC. Atypical presentation of female genital tract tuberculosis. Eur J Obstet Gynecol Reprod Biol. 1984; 17:355–363.5. Cavalli Z, Ader F, Valour F, et al. Clinical presentation, diagnosis, and bacterial epidemiology of peritoneal tuberculosis in two university hospitals in France. Infect Dis Ther. 2016; 5:193–199.6. al-Quorain AA, Facharzt , Satti MB, al-Freihi HM, al-Gindan YM, al-Awad N. Abdominal tuberculosis in Saudi Arabia: a clinicopathological study of 65 cases. Am J Gastroenterol. 1993; 88:75–79.7. Ilhan AH, Durmuşoğlu F. Case report of a pelvic-peritoneal tuberculosis presenting as an adnexial mass and mimicking ovarian cancer, and a review of the literature. Infect Dis Obstet Gynecol. 2004; 12:87–89.8. Demirkazik FB, Akhan O, Ozmen MN, Akata D. US and CT findings in the diagnosis of tuberculous peritonitis. Acta Radiol. 1996; 37:517–520.9. Akhan O, Pringot J. Imaging of abdominal tuberculosis. Eur Radiol. 2002; 12:312–323.10. Demir K, Okten A, Kaymakoglu S, et al. Tuberculous peritonitis--reports of 26 cases, detailing diagnostic and therapeutic problems. Eur J Gastroenterol Hepatol. 2001; 13:581–585.11. Farantos Ch, Damilakis I, Germanos S, Lagoudellis A, Skaltsas S. Acute intestinal obstruction as the first manifestation of tuberculous peritonitis. Hellenic J Surg. 2013; 85:192–196.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cytomegalovirus Enteritis in an Immunocompetent Patient Causing Small Bowel Obstruction and Superior Mesenteric Artery Thrombosis: A Case Report
- Small Bowel Obstruction in Children: Usefulness of CT for Diagnosis and Localization
- A Case of Fulminant Sclerosing Peritonitis Presented Like Acute Culture-Negative Peritonitis and Successfully Treated with Corticosteroid Therapy
- Closed loop obstruction of the small bowel: CT and sonographic findings
- A case of a dialysis patient with sclerosing peritonitis initially suspected of tuberculous peritonitis