Ann Rehabil Med.
2016 Oct;40(5):915-923. 10.5535/arm.2016.40.5.915.
Physiological Responses During the Lower Body Positive Pressure Supported Treadmill Test
- Affiliations
-
- 1Department of Physical and Rehabilitation Medicine, Regional Cardiocerebrovascular Center, Chonnam National University Hospital, Gwangju, Korea. rmhanjy@daum.net
- 2Center for Aging and Geriatrics, Chonnam National University Medical School, Gwangju, Korea.
- KMID: 2382924
- DOI: http://doi.org/10.5535/arm.2016.40.5.915
Abstract
OBJECTIVE
To quantify changes in cardiopulmonary function using a lower body positive pressure supported (LBPPS) treadmill during the exercise tolerance test (ETT) in healthy subjects before applying the LBPPS treadmill in patients with gait problems.
METHODS
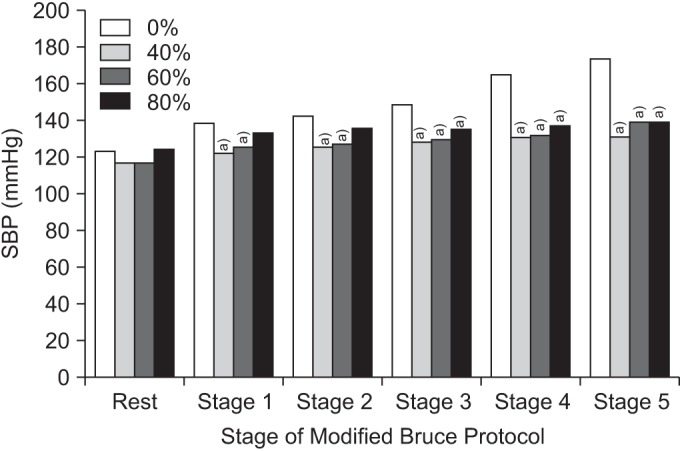
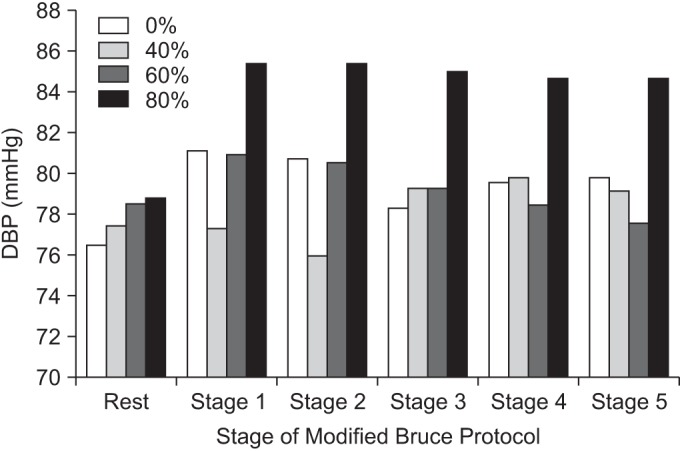
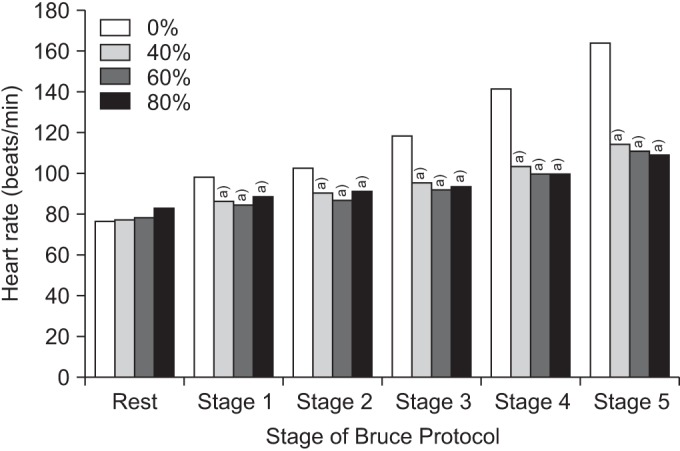
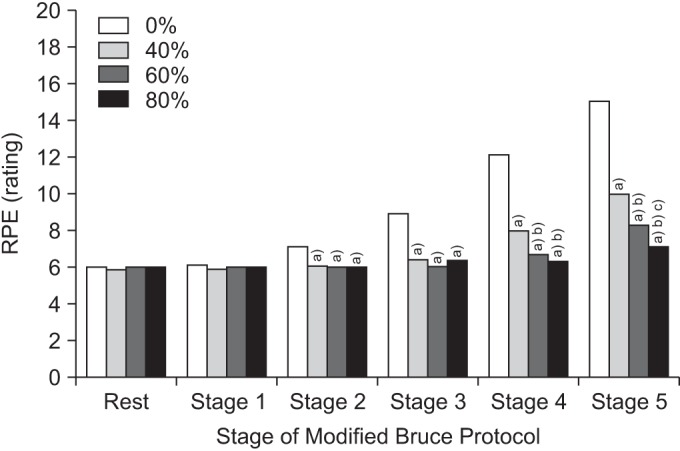
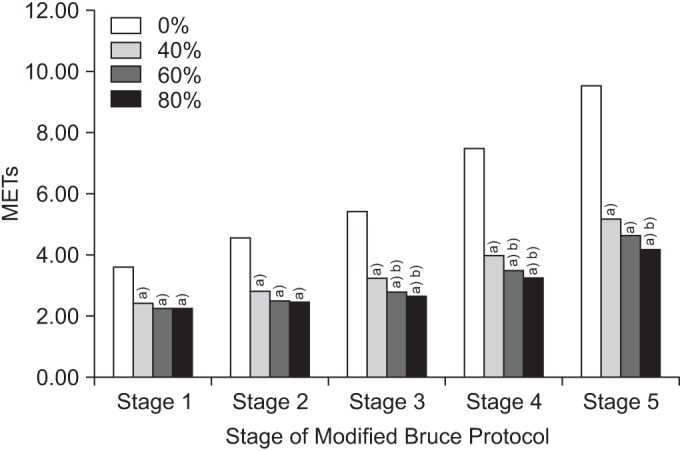
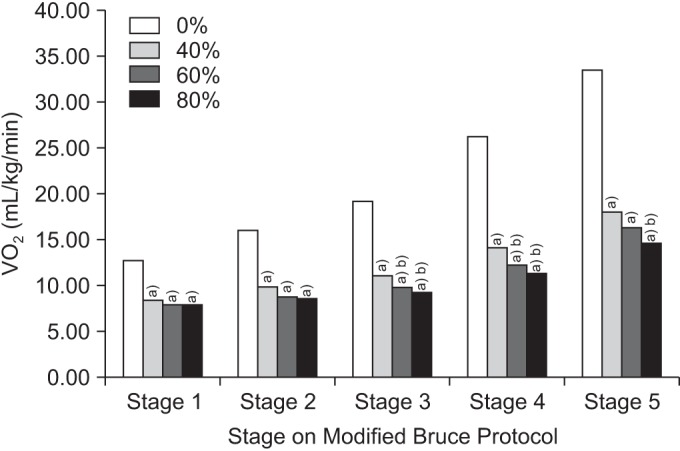
We evaluated 30 healthy subjects who were able to walk independently. The ETT was performed using the Modified Bruce Protocol (stages 1-5) at four levels (0%, 40%, 60%, and 80%) of LBPPS. The time interval at each level of the LBPPS treadmill test was 20 minutes to recover to baseline status. We measured systolic blood pressure, diastolic blood pressure, peak heart rate (PHR), rating of perceived exertion (RPE), metabolic equivalents (METs), and oxygen consumption rate (VOâ‚‚) during each LBPPS condition.
RESULTS
Systolic blood pressure increased as the LBPPS level was increased (40% to 80%). PHR, RPE, METs, and VOâ‚‚ were negatively associated with the LBPPS condition, although they were not always significant different among the LBPPS levels. The equation from a random effect linear regression model was as follows: VOâ‚‚ (mL/kg/min)=(2.75×stage)+(-0.14×LBPPS level)+11.9 (r²=0.69).
CONCLUSION
Detection of the changes in physiological parameters during a submaximal ETT using the LBPPS system may be helpful for applying the LBPPS treadmill in patients who cannot perform the ETT due to gait problems, even at submaximal intensity.
MeSH Terms
Figure
Cited by 1 articles
-
An Erratum to Correct Typographical Errors
Ann Rehabil Med. 2016;40(6):1151-1151. doi: 10.5535/arm.2016.40.6.1151.
Reference
-
1. Dunagan J, Adams J, Cheng D, Barton S, Bigej-Cerqua J, Mims L, et al. Development and evaluation of a treadmill-based exercise tolerance test in cardiac rehabilitation. Proc (Bayl Univ Med Cent). 2013; 26:247–251. PMID: 23814381.
Article2. Cutuk A, Groppo ER, Quigley EJ, White KW, Pedowitz RA, Hargens AR. Ambulation in simulated fractional gravity using lower body positive pressure: cardiovascular safety and gait analyses. J Appl Physiol (1985). 2006; 101:771–777. PMID: 16777997.
Article3. Kurz MJ, Corr B, Stuberg W, Volkman KG, Smith N. Evaluation of lower body positive pressure supported treadmill training for children with cerebral palsy. Pediatr Phys Ther. 2011; 23:232–239. PMID: 21829114.
Article4. Takacs J, Anderson JE, Leiter JR, MacDonald PB, Peeler JD. Lower body positive pressure: an emerging technology in the battle against knee osteoarthritis? Clin Interv Aging. 2013; 8:983–991. PMID: 23926425.5. Moore MN, Vandenakker-Albanese C, Hoffman MD. Use of partial body-weight support for aggressive return to running after lumbar disk herniation: a case report. Arch Phys Med Rehabil. 2010; 91:803–805. PMID: 20434621.
Article6. Mangione KK, Axen K, Haas F. Mechanical unweighting effects on treadmill exercise and pain in elderly people with osteoarthritis of the knee. Phys Ther. 1996; 76:387–394. PMID: 8606901.7. Ganesan M, Sathyaprabha TN, Pal PK, Gupta A. Partial body weight-supported treadmill training in patients with Parkinson disease: impact on gait and clinical manifestation. Arch Phys Med Rehabil. 2015; 96:1557–1565. PMID: 26008873.
Article8. Rose MH, Lokkegaard A, Sonne-Holm S, Jensen BR. Improved clinical status, quality of life, and walking capacity in Parkinson's disease after body weight-supported high-intensity locomotor training. Arch Phys Med Rehabil. 2013; 94:687–692. PMID: 23187043.
Article9. Sousa CO, Barela JA, Prado-Medeiros CL, Salvini TF, Barela AM. Gait training with partial body weight support during overground walking for individuals with chronic stroke: a pilot study. J Neuroeng Rehabil. 2011; 8:48. PMID: 21864373.
Article10. Visintin M, Barbeau H, Korner-Bitensky N, Mayo NE. A new approach to retrain gait in stroke patients through body weight support and treadmill stimulation. Stroke. 1998; 29:1122–1128. PMID: 9626282.
Article11. Senthilvelkumar T, Magimairaj H, Fletcher J, Tharion G, George J. Comparison of body weight-supported treadmill training versus body weight-supported overground training in people with incomplete tetraplegia: a pilot randomized trial. Clin Rehabil. 2015; 29:42–49. PMID: 24965958.
Article12. Ruckstuhl H, Kho J, Weed M, Wilkinson MW, Hargens AR. Comparing two devices of suspended treadmill walking by varying body unloading and Froude number. Gait Posture. 2009; 30:446–451. PMID: 19674901.
Article13. Grabowski AM. Metabolic and biomechanical effects of velocity and weight support using a lower-body positive pressure device during walking. Arch Phys Med Rehabil. 2010; 91:951–957. PMID: 20510989.
Article14. Sota T, Matsuo S, Uchida Y, Hagino H, Kawai Y. Effects of lower body positive pressure on cardiovascular responses during walking in elderly women. Physiol Res. 2013; 62:653–662. PMID: 23869890.
Article15. Gojanovic B, Cutti P, Shultz R, Matheson GO. Maximal physiological parameters during partial bodyweight support treadmill testing. Med Sci Sports Exerc. 2012; 44:1935–1941. PMID: 22543742.
Article16. Hoffman MD, Donaghe HE. Physiological responses to body weight : supported treadmill exercise in healthy adults. Arch Phys Med Rehabil. 2011; 92:960–966. PMID: 21621673.17. Fu Q, Sugiyama Y, Kamiya A, Shamsuzzaman AS, Mano T. Responses of muscle sympathetic nerve activity to lower body positive pressure. Am J Physiol. 1998; 275(4 Pt 2):H1254–H1259. PMID: 9746473.18. Macias BR, D'Lima DD, Cutuk A, Patil S, Steklov N, Neuschwander TB, et al. Leg intramuscular pressures and in vivo knee forces during lower body positive and negative pressure treadmill exercise. J Appl Physiol (1985). 2012; 113:31–38. PMID: 22539171.
Article19. Williamson JW, Mitchell JH, Olesen HL, Raven PB, Secher NH. Reflex increase in blood pressure induced by leg compression in man. J Physiol. 1994; 475:351–357. PMID: 8021841.
Article20. Nishiyasu T, Nagashima K, Nadel ER, Mack GW. Effects of posture on cardiovascular responses to lower body positive pressure at rest and during dynamic exercise. J Appl Physiol (1985). 1998; 85:160–167. PMID: 9655770.21. Grabowski A, Farley CT, Kram R. Independent metabolic costs of supporting body weight and accelerating body mass during walking. J Appl Physiol (1985). 2005; 98:579–583. PMID: 15649878.
Article22. McNeill DK, Kline JR, de Heer HD, Coast JR. Oxygen consumption of elite distance runners on an antigravity treadmill. J Sports Sci Med. 2015; 14:333–339. PMID: 25983582.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correction: Physiological Responses During the Lower Body Positive Pressure Supported Treadmill Test
- The Therapeutic Effects of Body Weight-Supported Treadmill Training on Childeren with Cerebral Palsy
- Cardiovascular Response During Submaximal Underwater Treadmill Exercise in Stroke Patients
- Usefulness of Treadmill Exercise Test on Diabetes Mellitus
- The Effect of Treadmill Aerobic Exercise in Stroke Patients