Management of ulcerative colitis in Taiwan: consensus guideline of the Taiwan Society of Inflammatory Bowel Disease
- Affiliations
-
- 1Department of Internal Medicine, National Taiwan University Hospital, National Taiwan University College of Medicine, Taipei, Taiwan. jmwong@ntu.edu.tw
- 2Department of Pathology, Taipei City Hospital Renai Branch, Taipei, Taiwan.
- 3Division of Colorectal Surgery, Department of Surgery, Taichung Veterans General Hospital, Taichung, Taiwan.
- 4Division of Colorectal Surgery, Chang Gung Memorial Hospital at Linkou, Taoyuan, Taiwan.
- 5Division of Gastroenterology and Hepatology, Department of Internal Medicine, China Medical University Hospital, Taichung, Taiwan.
- 6Division of General Surgery, Department of Surgery, Shin Kong Wu Ho-Su Memorial Hospital, Taipei, Taiwan.
- 7Department of Internal Medicine, National Cheng Kung University Hospital, National Cheng Kung University College of Medicine, Tainan, Taiwan.
- 8Division of Gastroenterology, Department of Internal Medicine, Kaohsiung Municipal Hsiaokang Hospital, Kaohsiung, Taiwan.
- 9Division of Gastroenterology, Department of Internal Medicine, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan.
- 10Division of Colon and Rectal Surgery, Department of Surgery, Mackay Memorial Hospital, Taipei, Taiwan.
- 11Division of Colon and Rectal Surgery, Department of Surgery, Taipei Veterans General Hospital, Taipei, Taiwan.
- 12Department of Surgery, National Yang-Ming University, Taipei, Taiwan.
- 13Department of Internal Medicine, Mackay Memorial Hospital, Taipei, Taiwan.
- 14Department of Pediatrics, National Taiwan University Hospital, Taipei, Taiwan.
- 15Department of Oncology, National Taiwan University Hospital, National Taiwan University College of Medicine, Taipei, Taiwan.
- 16Department of Medical Imaging, National Taiwan University Hospital, National Taiwan University College of Medicine, Taipei, Taiwan.
- 17Department of Pathology and Forensic Medicine, National Taiwan University Hospital, National Taiwan University College of Medicine, Taipei, Taiwan.
- 18Division of Medical Imaging, Department of Radiology, Far Eastern Memorial Hospital, New Taipei City, Taipei, Taiwan.
- 19Division of Gastroenterology, Department of Internal Medicine, MacKay Memorial Hospital, Taipei, Taiwan.
- 20MacKay Junior College of Medicine, Nursing, and Management, Taipei, Taiwan.
- 21MacKay Medical College, New Taipei City, Taipei, Taiwan.
- 22Department of Internal Medicine, Far Eastern Memorial Hospital, New Taipei City, Taipei, Taiwan.
- 23Division of Gastroenterology, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taipei, Taiwan.
- 24Department of Internal Medicine, Kaohsiung Municipal Ta-Tung Hospital, Kaohsiung, Taipei, Taiwan.
- 25Division of Gastroenterology, Department of Medicine, Taipei City Hospital Renai Branch, Taipei, Taiwan.
- 26Division of Gastroenterology, Department of Internal Medicine, Changhua Christian Hospital, Changhua, Taiwan.
- KMID: 2382372
- DOI: http://doi.org/10.5217/ir.2017.15.3.266
Abstract
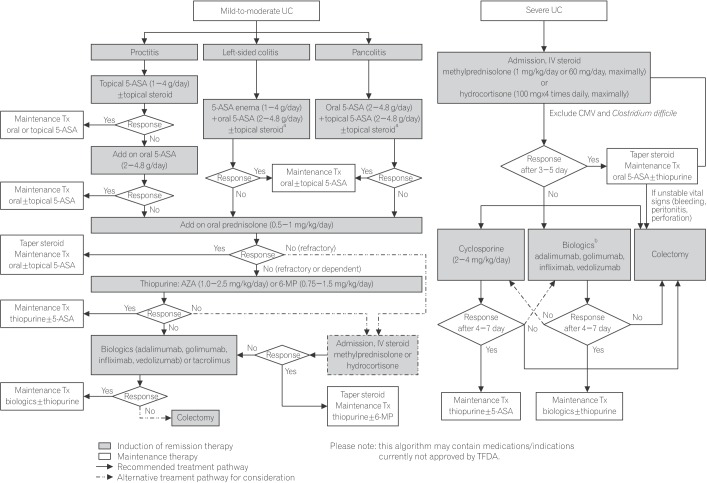
- Ulcerative colitis (UC) is an inflammatory bowel disease characterized by chronic mucosal inflammation of the colon, and the prevalence and incidence of UC have been steadily increasing in Taiwan. A steering committee was established by the Taiwan Society of Inflammatory Bowel Disease to formulate statements on the diagnosis and management of UC taking into account currently available evidence and the expert opinion of the committee. Accurate diagnosis of UC requires thorough clinical, endoscopic, and histological assessment and careful exclusion of differential diagnoses, particularly infectious colitis. The goals of UC therapy are to induce and maintain remission, reduce the risk of complications, and improve quality of life. As outlined in the recommended treatment algorithm, choice of treatment is dictated by severity, extent, and course of disease. Patients should be evaluated for hepatitis B virus and tuberculosis infection prior to immunosuppressive treatment, especially with steroids and biologic agents, and should be regularly monitored for reactivation of latent infection. These consensus statements are also based on current local evidence with consideration of factors, and could be serve as concise and practical guidelines for supporting clinicians in the management of UC in Taiwan.
Keyword
MeSH Terms
Figure
Cited by 5 articles
-
Epidemiological trend in inflammatory bowel disease in Taiwan from 2001 to 2015: a nationwide populationbased study
Hsu-Heng Yen, Meng-Tzu Weng, Chien-Chih Tung, Yu-Ting Wang, Yuan Ting Chang, Chin-Hao Chang, Ming-Jium Shieh, Jau-Min Wong, Shu-Chen Wei
Intest Res. 2019;17(1):54-62. doi: 10.5217/ir.2018.00096.Adherence to Asacol once daily versus divided regimen for maintenance therapy in ulcerative colitis: a prospective, multicenter, randomized study
Soo-Kyung Park, Sang Hyun Park, Chang Soo Eun, Geom Seog Seo, Jong Pil Im, Tae Oh Kim, Dong-Il Park
Intest Res. 2019;17(3):349-356. doi: 10.5217/ir.2018.00064.Response to hepatitis B vaccination in patients with inflammatory bowel disease: a prospective observational study in Korea
Ji Young Chang, Sung-Ae Jung, Chang Mo Moon, Seong-Eun Kim, Hye-Kyung Jung, Ki-Nam Shim
Intest Res. 2018;16(4):599-608. doi: 10.5217/ir.2018.00012.Improvement of ulcerative colitis control by searching and restricting of inflammatory trigger factors in daily clinical practice
Kun-Yu Tsai, Jeng-Fu You, Tzong-Yun Tsai, Yih Jong Chern, Yu-Jen Hsu, Shu-Huan Huang, Wen-Sy Tsai
Intest Res. 2023;21(1):100-109. doi: 10.5217/ir.2021.00110.Treatment of inflammatory bowel disease–Asian perspectives: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting
Eun Mi Song, Soo-Young Na, Sung Noh Hong, Siew Chien Ng, Tadakazu Hisamatsu, Byong Duk Ye
Intest Res. 2023;21(3):339-352. doi: 10.5217/ir.2022.00135.
Reference
-
1. Feuerstein JD, Cheifetz AS. Ulcerative colitis: epidemiology, diagnosis, and management. Mayo Clin Proc. 2014; 89:1553–1563. PMID: 25199861.2. Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012; 142:46–54. PMID: 22001864.
Article3. Cosnes J, Gower-Rousseau C, Seksik P, Cortot A. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011; 140:1785–1794. PMID: 21530745.
Article4. Wei SC, Lin MH, Tung CC, et al. A nationwide populationbased study of the inflammatory bowel diseases between 1998 and 2008 in Taiwan. BMC Gastroenterol. 2013; 13:166. PMID: 24314308.
Article5. Chuang CH, Lin SH, Chen CY, Sheu BS, Kao AW, Wang JD. Increasing incidence and lifetime risk of inflammatory bowel disease in Taiwan: a nationwide study in a low-endemic area 1998-2010. Inflamm Bowel Dis. 2013; 19:2815–2819. PMID: 24141711.
Article6. Kuo CJ, Yu KH, See LC, et al. The trend of inflammatory bowel diseases in Taiwan: a population-based study. Dig Dis Sci. 2015; 60:2454–2462. PMID: 25837597.7. Wang LH, Yang YJ, Cheng WC, Wang WM, Lin SH, Shieh CC. Higher risk for hematological malignancies in inflammatory bowel disease: a nationwide population-based study in Taiwan. Am J Gastroenterol. 2016; 111:1313–1319. PMID: 27296944.8. Danese S, Fiocchi C. Ulcerative colitis. N Engl J Med. 2011; 365:1713–1725. PMID: 22047562.9. Dignass A, Eliakim R, Magro F, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 1: definitions and diagnosis. J Crohns Colitis. 2012; 6:965–990. PMID: 23040452.10. Dignass A, Lindsay JO, Sturm A, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 2: current management. J Crohns Colitis. 2012; 6:991–1030. PMID: 23040451.
Article11. Talley NJ, Abreu MT, Achkar JP, et al. An evidence-based systematic review on medical therapies for inflammatory bowel disease. Am J Gastroenterol. 2011; 106(Suppl 1):S2–S25. PMID: 21472012.
Article12. Ooi CJ, Fock KM, Makharia GK, et al. The Asia-Pacific consensus on ulcerative colitis. J Gastroenterol Hepatol. 2010; 25:453–468. PMID: 20370724.
Article13. Lan JY. Achieving and sustaining universal health coverage: fiscal reform of the National Health Insurance in Taiwan. Appl Health Econ Health Policy. published online ahead of print October 25, 2016. DOI: 10.1007/s40258-016-0286-6.14. Ng SC, Tang W, Ching JY, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asiapacific Crohn's and colitis epidemiology study. Gastroenterology. 2013; 145:158–165.e2. PMID: 23583432.
Article15. Loftus EV Jr. Clinical epidemiology of inflammatory bowel disease: incidence, prevalence, and environmental influences. Gastroenterology. 2004; 126:1504–1517. PMID: 15168363.
Article16. Thia KT, Loftus EV Jr, Sandborn WJ, Yang SK. An update on the epidemiology of inflammatory bowel disease in Asia. Am J Gastroenterol. 2008; 103:3167–3182. PMID: 19086963.
Article17. Prideaux L, Kamm MA, De Cruz PP, Chan FK, Ng SC. Inflammatory bowel disease in Asia: a systematic review. J Gastroenterol Hepatol. 2012; 27:1266–1280. PMID: 22497584.
Article18. Asakura K, Nishiwaki Y, Inoue N, Hibi T, Watanabe M, Takebayashi T. Prevalence of ulcerative colitis and Crohn's disease in Japan. J Gastroenterol. 2009; 44:659–665. PMID: 19424654.
Article19. Yang SK, Yun S, Kim JH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008; 14:542–549. PMID: 17941073.
Article20. Bernstein CN, Wajda A, Svenson LW, et al. The epidemiology of inflammatory bowel disease in Canada: a population-based study. Am J Gastroenterol. 2006; 101:1559–1568. PMID: 16863561.
Article21. Gearry RB, Richardson A, Frampton CM, et al. High incidence of Crohn's disease in Canterbury, New Zealand: results of an epidemiologic study. Inflamm Bowel Dis. 2006; 12:936–943. PMID: 17012964.
Article22. Molinié F, Gower-Rousseau C, Yzet T, et al. Opposite evolution in incidence of Crohn's disease and ulcerative colitis in Northern France (1988-1999). Gut. 2004; 53:843–848. PMID: 15138211.
Article23. Larsen S, Bendtzen K, Nielsen OH. Extraintestinal manifestations of inflammatory bowel disease: epidemiology, diagnosis, and management. Ann Med. 2010; 42:97–114. PMID: 20166813.
Article24. Hsu YC, Wu TC, Lo YC, Wang LS. Gastrointestinal complications and extraintestinal manifestations of inflammatory bowel disease in Taiwan: a population-based study. J Chin Med Assoc. 2017; 80:56–62. PMID: 27838292.
Article25. Wei SC, Shieh MJ, Chang MC, Chang YT, Wang CY, Wong JM. Long-term follow-up of ulcerative colitis in Taiwan. J Chin Med Assoc. 2012; 75:151–155. PMID: 22541142.
Article26. Su CG, Judge TA, Lichtenstein GR. Extraintestinal manifestations of inflammatory bowel disease. Gastroenterol Clin North Am. 2002; 31:307–327. PMID: 12122740.
Article27. Bernstein CN, Blanchard JF, Rawsthorne P, Yu N. The prevalence of extraintestinal diseases in inflammatory bowel disease: a population-based study. Am J Gastroenterol. 2001; 96:1116–1122. PMID: 11316157.
Article28. Tedesco FJ, Hardin RD, Harper RN, Edwards BH. Infectious colitis endoscopically simulating inflammatory bowel disease: a prospective evaluation. Gastrointest Endosc. 1983; 29:195–197. PMID: 6618115.
Article29. Chodos JE. Campylobacter infection mimicking ulcerative colitis. N Y State J Med. 1986; 86:22–23. PMID: 3456506.30. Siegal D, Syed F, Hamid N, Cunha BA. Campylobacter jejuni pancolitis mimicking idiopathic ulcerative colitis. Heart Lung. 2005; 34:288–290. PMID: 16027651.
Article31. Dunzendorfer T, Kasznica J. Amebic and/or ulcerative colitis. Gastrointest Endosc. 1998; 48:450–451. PMID: 9786131.
Article32. Ibrahim TM, Iheonunekwu N, Gill V, Vantapool H. Differentiating amoebic ulcero-haemorrhagic recto-colitis from idiopathic inflammatory bowel disease: still a diagnostic dilemma. West Indian Med J. 2005; 54:210–212. PMID: 16209229.
Article33. Misra SP, Misra V, Dwivedi M, Singh PA. Colonic tuberculosis mimicking ulcerative colitis. J Assoc Physicians India. 1998; 46:309–310. PMID: 11273353.34. Sands BE. From symptom to diagnosis: clinical distinctions among various forms of intestinal inflammation. Gastroenterology. 2004; 126:1518–1532. PMID: 15168364.
Article35. Truelove SC, Witts LJ. Cortisone in ulcerative colitis: final report on a therapeutic trial. Br Med J. 1955; 2:1041–1048. PMID: 13260656.36. Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis: a randomized study. N Engl J Med. 1987; 317:1625–1629. PMID: 3317057.
Article37. Pera A, Bellando P, Caldera D, et al. Colonoscopy in inflammatory bowel disease: diagnostic accuracy and proposal of an endoscopic score. Gastroenterology. 1987; 92:181–185. PMID: 3781186.38. Carbonnel F, Lavergne A, Lémann M, et al. Colonoscopy of acute colitis: a safe and reliable tool for assessment of severity. Dig Dis Sci. 1994; 39:1550–1557. PMID: 8026269.39. Hibi T, Ueno F, Matsuoka K, Lee TC. Guidelines for the management of ulcerative colitis in Japan: developed through integration of evidence and consensus among experts. IBD Res. 2010; 4:189–239.40. Prantera C, Lorenzetti R, Cerro P, Davoli M, Brancato G, Fanucci A. The plain abdominal film accurately estimates extent of active ulcerative colitis. J Clin Gastroenterol. 1991; 13:231–234. PMID: 2033232.
Article41. Buckell NA, Williams GT, Bartram CI, Lennard-Jones JE. Depth of ulceration in acute colitis: correlation with outcome and clinical and radiologic features. Gastroenterology. 1980; 79:19–25. PMID: 7380218.42. Panes J, Bouhnik Y, Reinisch W, et al. Imaging techniques for assessment of inflammatory bowel disease: joint ECCO and ESGAR evidence-based consensus guidelines. J Crohns Colitis. 2013; 7:556–585. PMID: 23583097.
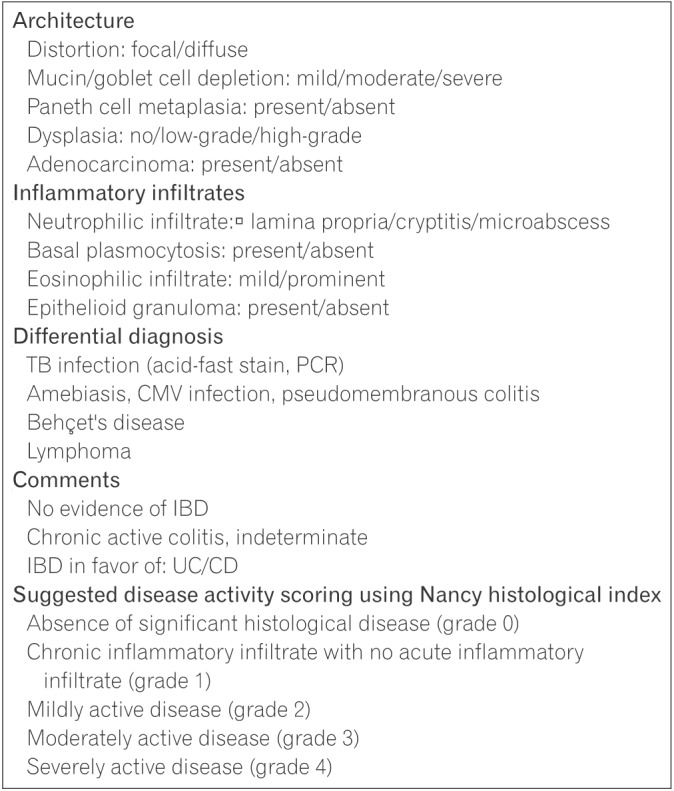
Article43. Washington K, Greenson JK, Montgomery E, et al. Histopathology of ulcerative colitis in initial rectal biopsy in children. Am J Surg Pathol. 2002; 26:1441–1449. PMID: 12409720.
Article44. Jenkins D, Balsitis M, Gallivan S, et al. Guidelines for the initial biopsy diagnosis of suspected chronic idiopathic inflammatory bowel disease: the British Society of Gastroenterology Initiative. J Clin Pathol. 1997; 50:93–105. PMID: 9155688.
Article45. Dundas SA, Dutton J, Skipworth P. Reliability of rectal biopsy in distinguishing between chronic inflammatory bowel disease and acute self-limiting colitis. Histopathology. 1997; 31:60–66. PMID: 9253626.
Article46. Tanaka M, Saito H, Kusumi T, et al. Spatial distribution and histogenesis of colorectal Paneth cell metaplasia in idiopathic inflammatory bowel disease. J Gastroenterol Hepatol. 2001; 16:1353–1359. PMID: 11851832.
Article47. Nostrant TT, Kumar NB, Appelman HD. Histopathology differentiates acute self-limited colitis from ulcerative colitis. Gastroenterology. 1987; 92:318–328. PMID: 3792768.
Article48. Schmitz-Moormann P, Himmelmann GW. Does quantitative histology of rectal biopsy improve the differential diagnosis of Crohn's disease and ulcerative colitis in adults. Pathol Res Pract. 1988; 183:481–488. PMID: 3186548.
Article49. DeRoche TC, Xiao SY, Liu X. Histological evaluation in ulcerative colitis. Gastroenterol Rep (Oxf). 2014; 2:178–192. PMID: 24942757.
Article50. Tanaka M, Riddell RH, Saito H, Soma Y, Hidaka H, Kudo H. Morphologic criteria applicable to biopsy specimens for effective distinction of inflammatory bowel disease from other forms of colitis and of Crohn's disease from ulcerative colitis. Scand J Gastroenterol. 1999; 34:55–67. PMID: 10048734.
Article51. Goldstein N, Dulai M. Contemporary morphologic definition of backwash ileitis in ulcerative colitis and features that distinguish it from Crohn disease. Am J Clin Pathol. 2006; 126:365–376. PMID: 16880149.
Article52. Kim B, Barnett JL, Kleer CG, Appelman HD. Endoscopic and histological patchiness in treated ulcerative colitis. Am J Gastroenterol. 1999; 94:3258–3262. PMID: 10566726.
Article53. Kleer CG, Appelman HD. Ulcerative colitis: patterns of involvement in colorectal biopsies and changes with time. Am J Surg Pathol. 1998; 22:983–989. PMID: 9706978.54. Bernstein CN, Shanahan F, Anton PA, Weinstein WM. Patchiness of mucosal inflammation in treated ulcerative colitis: a prospective study. Gastrointest Endosc. 1995; 42:232–237. PMID: 7498688.
Article55. Ott JJ, Stevens GA, Groeger J, Wiersma ST. Global epidemiology of hepatitis B virus infection: new estimates of age-specific HBsAg seroprevalence and endemicity. Vaccine. 2012; 30:2212–2219. PMID: 22273662.
Article56. Cheon JH. Understanding the complications of anti-tumor necrosis factor therapy in East Asian patients with inflammatory bowel disease. J Gastroenterol Hepatol. 2017; 32:769–777. PMID: 27723166.
Article57. Rahier JF, Magro F, Abreu C, et al. Second European evidencebased consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease. J Crohns Colitis. 2014; 8:443–468. PMID: 24613021.
Article58. Loras C, Gisbert JP, Mínguez M, et al. Liver dysfunction related to hepatitis B and C in patients with inflammatory bowel disease treated with immunosuppressive therapy. Gut. 2010; 59:1340–1346. PMID: 20577000.
Article59. Park SH, Yang SK, Lim YS, et al. Clinical courses of chronic hepatitis B virus infection and inflammatory bowel disease in patients with both diseases. Inflamm Bowel Dis. 2012; 18:2004–2010. PMID: 22337144.
Article60. Altunöz ME, Senateş E, Yeşil A, Calhan T, Ovünç AO. Patients with inflammatory bowel disease have a lower response rate to HBV vaccination compared to controls. Dig Dis Sci. 2012; 57:1039–1044. PMID: 22147248.
Article61. Gisbert JP, Menchén L, García-Sánchez V, Marín I, Villagrasa JR, Chaparro M. Comparison of the effectiveness of two protocols for vaccination (standard and double dosage) against hepatitis B virus in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2012; 35:1379–1385. PMID: 22530631.
Article62. Weng MT, Wei SC, Lin CC, et al. Seminar report from the 2014 Taiwan Society of Inflammatory Bowel Disease (TSIBD) spring forum (May 24th, 2014): Crohn's disease versus intestinal tuberculosis infection. Intest Res. 2015; 13:6–10. PMID: 25691838.
Article63. Horsburgh CR Jr, Rubin EJ. Clinical practice: latent tuberculosis infection in the United States. N Engl J Med. 2011; 364:1441–1448. PMID: 21488766.64. Tuberculosis diagnosis and treatment guidelines (version 5.1). Centers for Disease Control, R.O.C. (Taiwan) Web site;Updated December 17, 2015. Accessed March 3, 2017. http://www.cdc.gov.tw/professional/info.aspx?treeid=beac9c103df952c4&nowtreeid=6744c19c09435458&tid=B02B73C3D6F15437.65. Munkholm P, Michetti P, Probert CS, Elkjaer M, Marteau P. Best practice in the management of mild-to-moderately active ulcerative colitis and achieving maintenance of remission using mesalazine. Eur J Gastroenterol Hepatol. 2010; 22:912–916. PMID: 20665988.66. Cohen RD, Woseth DM, Thisted RA, Hanauer SB. A metaanalysis and overview of the literature on treatment options for left-sided ulcerative colitis and ulcerative proctitis. Am J Gastroenterol. 2000; 95:1263–1276. PMID: 10811338.
Article67. Marshall JK, Irvine EJ. Rectal corticosteroids versus alternative treatments in ulcerative colitis: a meta-analysis. Gut. 1997; 40:775–781. PMID: 9245932.
Article68. Safdi M, DeMicco M, Sninsky C, et al. A double-blind comparison of oral versus rectal mesalamine versus combination therapy in the treatment of distal ulcerative colitis. Am J Gastroenterol. 1997; 92:1867–1871. PMID: 9382054.69. Lewis JD, Gelfand JM, Troxel AB, et al. Immunosuppressant medications and mortality in inflammatory bowel disease. Am J Gastroenterol. 2008; 103:1428–1435. PMID: 18494836.
Article70. Hoes JN, Jacobs JW, Verstappen SM, Bijlsma JW, Van der. Adverse events of low- to medium-dose oral glucocorticoids in inflammatory diseases: a meta-analysis. Ann Rheum Dis. 2009; 68:1833–1838. PMID: 19066177.
Article71. Lichtenstein GR. Budesonide multi-matrix for the treatment of patients with ulcerative colitis. Dig Dis Sci. 2016; 61:358–370. PMID: 26541989.
Article72. Brunner M, Ziegler S, Di Stefano AF, et al. Gastrointestinal transit, release and plasma pharmacokinetics of a new oral budesonide formulation. Br J Clin Pharmacol. 2006; 61:31–38. PMID: 16390349.
Article73. Sandborn WJ, Travis S, Moro L, et al. Once-daily budesonide MMX® extended-release tablets induce remission in patients with mild to moderate ulcerative colitis: results from the CORE I study. Gastroenterology. 2012; 143:1218–1226. PMID: 22892337.
Article74. Travis SP, Danese S, Kupcinskas L, et al. Once-daily budesonide MMX in active, mild-to-moderate ulcerative colitis: results from the randomised CORE II study. Gut. 2014; 63:433–441. PMID: 23436336.
Article75. Marteau P, Probert CS, Lindgren S, et al. Combined oral and enema treatment with Pentasa (mesalazine) is superior to oral therapy alone in patients with extensive mild/moderate active ulcerative colitis: a randomised, double blind, placebo controlled study. Gut. 2005; 54:960–965. PMID: 15951542.
Article76. Kamm MA, Sandborn WJ, Gassull M, et al. Once-daily, highconcentration MMX mesalamine in active ulcerative colitis. Gastroenterology. 2007; 132:66–75. PMID: 17241860.
Article77. Kruis W, Kiudelis G, Rácz I, et al. Once daily versus three times daily mesalazine granules in active ulcerative colitis: a doubleblind, double-dummy, randomised, non-inferiority trial. Gut. 2009; 58:233–240. PMID: 18832520.
Article78. Sandborn WJ, Kamm MA, Lichtenstein GR, Lyne A, Butler T, Joseph RE. MMX Multi Matrix System mesalazine for the induction of remission in patients with mild-to-moderate ulcerative colitis: a combined analysis of two randomized, doubleblind, placebo-controlled trials. Aliment Pharmacol Ther. 2007; 26:205–215. PMID: 17593066.
Article79. Truelove SC, Jewell DP. Intensive intravenous regimen for severe attacks of ulcerative colitis. Lancet. 1974; 1:1067–1070. PMID: 4135487.
Article80. Turner D, Walsh CM, Steinhart AH, Griffiths AM. Response to corticosteroids in severe ulcerative colitis: a systematic review of the literature and a meta-regression. Clin Gastroenterol Hepatol. 2007; 5:103–110. PMID: 17142106.
Article81. Laharie D, Bourreille A, Branche J, et al. Ciclosporin versus infliximab in patients with severe ulcerative colitis refractory to intravenous steroids: a parallel, open-label randomised controlled trial. Lancet. 2012; 380:1909–1915. PMID: 23063316.
Article82. Lennard-Jones JE, Ritchie JK, Hilder W, Spicer CC. Assessment of severity in colitis: a preliminary study. Gut. 1975; 16:579–584. PMID: 1183857.
Article83. Lindgren SC, Flood LM, Kilander AF, Löfberg R, Persson TB, Sjödahl RI. Early predictors of glucocorticosteroid treatment failure in severe and moderately severe attacks of ulcerative colitis. Eur J Gastroenterol Hepatol. 1998; 10:831–835. PMID: 9831403.
Article84. Benazzato L, D'Incà R, Grigoletto F, et al. Prognosis of severe attacks in ulcerative colitis: effect of intensive medical treatment. Dig Liver Dis. 2004; 36:461–466. PMID: 15285525.
Article85. Chew CN, Nolan DJ, Jewell DP. Small bowel gas in severe ulcerative colitis. Gut. 1991; 32:1535–1537. PMID: 1773962.
Article86. Almer S, Bodemar G, Franzén L, Lindström E, Nyström P, Ström M. Use of air enema radiography to assess depth of ulceration during acute attacks of ulcerative colitis. Lancet. 1996; 347:1731–1735. PMID: 8656906.
Article87. Randall J, Singh B, Warren BF, Travis SP, Mortensen NJ, George BD. Delayed surgery for acute severe colitis is associated with increased risk of postoperative complications. Br J Surg. 2010; 97:404–409. PMID: 20101648.
Article88. Wang Y, Parker CE, Feagan BG, MacDonald JK. Oral 5-aminosalicylic acid for maintenance of remission in ulcerative colitis. Cochrane Database Syst Rev. 2016; (5):CD000544. DOI: 10.1002/14651858.CD000544.pub4. PMID: 27158764.
Article89. Gionchetti P, Rizzello F, Venturi A, et al. Comparison of oral with rectal mesalazine in the treatment of ulcerative proctitis. Dis Colon Rectum. 1998; 41:93–97. PMID: 9510317.
Article90. Marshall JK, Irvine EJ. Putting rectal 5-aminosalicylic acid in its place: the role in distal ulcerative colitis. Am J Gastroenterol. 2000; 95:1628–1636. PMID: 10925961.
Article91. Prantera C, Marconi S. Glucocorticosteroids in the treatment of inflammatory bowel disease and approaches to minimizing systemic activity. Therap Adv Gastroenterol. 2013; 6:137–156.
Article92. Timmer A, McDonald JW, Macdonald JK. Azathioprine and 6-mercaptopurine for maintenance of remission in ulcerative colitis. Cochrane Database Syst Rev. 2007; (1):CD000478. DOI: 10.1002/14651858.CD000478.pub2. PMID: 17253451.
Article93. Ardizzone S, Maconi G, Russo A, Imbesi V, Colombo E, Bianchi Porro G. Randomised controlled trial of azathioprine and 5-aminosalicylic acid for treatment of steroid dependent ulcerative colitis. Gut. 2006; 55:47–53. PMID: 15972298.
Article94. Fernández-Bañares F, Bertrán X, Esteve-Comas M, et al. Azathioprine is useful in maintaining long-term remission induced by intravenous cyclosporine in steroid-refractory severe ulcerative colitis. Am J Gastroenterol. 1996; 91:2498–2499. PMID: 8946973.95. Moskovitz DN, Van Assche G, Maenhout B, et al. Incidence of colectomy during long-term follow-up after cyclosporine-induced remission of severe ulcerative colitis. Clin Gastroenterol Hepatol. 2006; 4:760–765. PMID: 16716758.
Article96. Rutgeerts P, Sandborn WJ, Feagan BG, et al. Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2005; 353:2462–2476. PMID: 16339095.
Article97. Sandborn WJ, van Assche G, Reinisch W, et al. Adalimumab induces and maintains clinical remission in patients with moderate-to-severe ulcerative colitis. Gastroenterology. 2012; 142:257–265.e3. PMID: 22062358.
Article98. Sandborn WJ, Feagan BG, Marano C, et al. Subcutaneous golimumab maintains clinical response in patients with moderate-to-severe ulcerative colitis. Gastroenterology. 2014; 146:96–109. PMID: 23770005.
Article99. Monterubbianesi R, Daperno M, Armuzzi A, et al. Infliximab for severe ulcerative colitis: short-term and one year outcome of three dose regimen: an Italian multicentre open-label study. Gastroenterology. 2010; 138:S685.100. Venu M, Naik AS, Ananthakrishnan AN, et al. Early infliximab infusion in hospitalized severe UC patients: one year outcome. Gastroenterology. 2009; 136(Suppl 1):A201.101. Feagan BG, Rutgeerts P, Sands BE, et al. Vedolizumab as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2013; 369:699–710. PMID: 23964932.
Article102. Keane J, Gershon S, Wise RP, et al. Tuberculosis associated with infliximab, a tumor necrosis factor alpha-neutralizing agent. N Engl J Med. 2001; 345:1098–1104. PMID: 11596589.
Article103. Toruner M, Loftus EV Jr, Harmsen WS, et al. Risk factors for opportunistic infections in patients with inflammatory bowel disease. Gastroenterology. 2008; 134:929–936. PMID: 18294633.
Article104. Mackey AC, Green L, Liang LC, Dinndorf P, Avigan M. Hepatosplenic T cell lymphoma associated with infliximab use in young patients treated for inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2007; 44:265–267. PMID: 17255842.
Article105. Kotlyar DS, Osterman MT, Diamond RH, et al. A systematic review of factors that contribute to hepatosplenic T-cell lymphoma in patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2011; 9:36–41. PMID: 20888436.
Article106. Froslie KF, Jahnsen J, Moum BA, Vatn MH. IBSEN Group. Mucosal healing in inflammatory bowel disease: results from a Norwegian population-based cohort. Gastroenterology. 2007; 133:412–422. PMID: 17681162.
Article107. Wright R, Truelove SR. Serial rectal biopsy in ulcerative colitis during the course of a controlled therapeutic trial of various diets. Am J Dig Dis. 1966; 11:847–857. PMID: 5953695.
Article108. Meucci G, Fasoli R, Saibeni S. Prognostic significance of endoscopy remission in patients with active ulcerative colitis treated with oral and topical mesalazine: preliminary results of a prospective, multicenter study. Gastroenterology. 2006; 130. PMID: 16831597.109. Rutter MD, Saunders BP, Wilkinson KH, et al. Cancer surveillance in longstanding ulcerative colitis: endoscopic appearances help predict cancer risk. Gut. 2004; 53:1813–1816. PMID: 15542520.
Article110. American Society for Gastrointestinal Endoscopy. Appropriate use of gastrointestinal endoscopy. Gastrointest Endosc. 2000; 52:831–837.111. Leighton JA, Shen B, Baron TH, et al. ASGE guideline: endoscopy in the diagnosis and treatment of inflammatory bowel disease. Gastrointest Endosc. 2006; 63:558–565. PMID: 16564852.
Article112. Bjarnason I, Sherwood R. Fecal calprotectin: a significant step in the noninvasive assessment of intestinal inflammation. J Pediatr Gastroenterol Nutr. 2001; 33:11–13. PMID: 11479401.
Article113. Summerton CB, Longlands MG, Wiener K, Shreeve DR. Faecal calprotectin: a marker of inflammation throughout the intestinal tract. Eur J Gastroenterol Hepatol. 2002; 14:841–845. PMID: 12172403.
Article114. Lin WC, Wong JM, Tung CC, et al. Fecal calprotectin correlated with endoscopic remission for Asian inflammatory bowel disease patients. World J Gastroenterol. 2015; 21:13566–13573. PMID: 26730169.
Article115. Limburg PJ, Ahlquist DA, Sandborn WJ, et al. Fecal calprotectin levels predict colorectal inflammation among patients with chronic diarrhea referred for colonoscopy. Am J Gastroenterol. 2000; 95:2831–2837. PMID: 11051356.
Article116. Tibble JA, Sigthorsson G, Bridger S, Fagerhol MK, Bjarnason I. Surrogate markers of intestinal inflammation are predictive of relapse in patients with inflammatory bowel disease. Gastroenterology. 2000; 119:15–22. PMID: 10889150.
Article117. Costa F, Mumolo MG, Ceccarelli L, et al. Calprotectin is a stronger predictive marker of relapse in ulcerative colitis than in Crohn's disease. Gut. 2005; 54:364–368. PMID: 15710984.
Article118. Aadland E, Fagerhol MK. Faecal calprotectin: a marker of inflammation throughout the intestinal tract. Eur J Gastroenterol Hepatol. 2002; 14:823–825. PMID: 12172400.
Article119. Røseth AG, Aadland E, Grzyb K. Normalization of faecal calprotectin: a predictor of mucosal healing in patients with inflammatory bowel disease. Scand J Gastroenterol. 2004; 39:1017–1020. PMID: 15513345.
Article120. Konikoff MR, Denson LA. Role of fecal calprotectin as a biomarker of intestinal inflammation in inflammatory bowel disease. Inflamm Bowel Dis. 2006; 12:524–534. PMID: 16775498.
Article121. Schoepfer AM, Trummler M, Seeholzer P. Calprotectin helps to distinguish between an acute IBD episode and symptoms related to IBS. Inflamm Bowel Dis. 2008; 14:1432–1439. PMID: 18484669.122. Rodgers AD, Cummins AG. CRP correlates with clinical score in ulcerative colitis but not in Crohn's disease. Dig Dis Sci. 2007; 52:2063–2068. PMID: 17436102.
Article123. Sachar DB, Smith H, Chan S, Cohen LB, Lichtiger S, Messer J. Erythrocytic sedimentation rate as a measure of clinical activity in inflammatory bowel disease. J Clin Gastroenterol. 1986; 8:647–650. PMID: 3805662.
Article124. Prantera C, Davoli M, Lorenzetti R, et al. Clinical and laboratory indicators of extent of ulcerative colitis: serum C-reactive protein helps the most. J Clin Gastroenterol. 1988; 10:41–45. PMID: 3356884.125. Solem CA, Loftus EV Jr, Tremaine WJ, Harmsen WS, Zinsmeister AR, Sandborn WJ. Correlation of C-reactive protein with clinical, endoscopic, histologic, and radiographic activity in inflammatory bowel disease. Inflamm Bowel Dis. 2005; 11:707–712. PMID: 16043984.
Article126. Murdoch T, O'Donnell S, Silverberg MS, Panaccione R. Biomarkers as potential treatment targets in inflammatory bowel disease: a systematic review. Can J Gastroenterol Hepatol. 2015; 29:203–208. PMID: 25965441.
Article127. Schneeweiss S, Korzenik J, Solomon DH, Canning C, Lee J, Bressler B. Infliximab and other immunomodulating drugs in patients with inflammatory bowel disease and the risk of serious bacterial infections. Aliment Pharmacol Ther. 2009; 30:253–264. PMID: 19438424.
Article128. Hsu J, Abad C, Dinh M, Safdar N. Prevention of endemic healthcare-associated Clostridium difficile infection: reviewing the evidence. Am J Gastroenterol. 2010; 105:2327–2339. PMID: 20606676.
Article129. Johal SS, Hammond J, Solomon K, James PD, Mahida YR. Clostridium difficile associated diarrhoea in hospitalised patients: onset in the community and hospital and role of flexible sigmoidoscopy. Gut. 2004; 53:673–677. PMID: 15082585.
Article130. Kandiel A, Lashner B. Cytomegalovirus colitis complicating inflammatory bowel disease. Am J Gastroenterol. 2006; 101:2857–2865. PMID: 17026558.
Article131. Nakase H, Chiba T. TNF-alpha is an important pathogenic factor contributing to reactivation of cytomegalovirus in inflamed mucosa of colon in patients with ulcerative colitis: lesson from clinical experience. Inflamm Bowel Dis. 2010; 16:550–551. PMID: 19637380.
Article132. Riley SA, Mani V, Goodman MJ, Dutt S, Herd ME. Microscopic activity in ulcerative colitis: what does it mean? Gut. 1991; 32:174–178. PMID: 1864537.
Article133. Geboes K, Riddell R, Ost A, Jensfelt B, Persson T, Löfberg R. A reproducible grading scale for histological assessment of inflammation in ulcerative colitis. Gut. 2000; 47:404–409. PMID: 10940279.
Article134. Marchal-Bressenot A, Salleron J, Boulagnon-Rombi C, et al. Development and validation of the Nancy histological index for UC. Gut. 2017; 66:43–49. PMID: 26464414.
Article135. Mosli MH, Feagan BG, Zou G, et al. Development and validation of a histological index for UC. Gut. 2017; 66:50–58. PMID: 26475633.
Article136. Øresland T, Bemelman WA, Sampietro GM, et al. European evidence based consensus on surgery for ulcerative colitis. J Crohns Colitis. 2015; 9:4–25. PMID: 25304060.
Article137. Fazio VW, Kiran RP, Remzi FH, et al. Ileal pouch anal anastomosis: analysis of outcome and quality of life in 3707 patients. Ann Surg. 2013; 257:679–685. PMID: 23299522.138. Ording Olsen K, Juul S, Berndtsson I, Øresland T, Laurberg S. Ulcerative colitis: female fecundity before diagnosis, during disease, and after surgery compared with a population sample. Gastroenterology. 2002; 122:15–19. PMID: 11781275.
Article139. Rajaratnam SG, Eglinton TW, Hider P, Fearnhead NS. Impact of ileal pouch-anal anastomosis on female fertility: meta-analysis and systematic review. Int J Colorectal Dis. 2011; 26:1365–1374. PMID: 21766164.
Article140. Waljee A, Waljee J, Morris AM, Higgins PD. Threefold increased risk of infertility: a meta-analysis of infertility after ileal pouch anal anastomosis in ulcerative colitis. Gut. 2006; 55:1575–1580. PMID: 16772310.
Article141. Thomas DM, Filipe MI, Smedley FH. Dysplasia and carcinoma in the rectal stump of total colitics who have undergone colectomy and ileo-rectal anastomosis. Histopathology. 1989; 14:289–298. PMID: 2707763.
Article142. Williamson ME, Lewis WG, Sagar PM, Holdsworth PJ, Johnston D. One-stage restorative proctocolectomy without temporary ileostomy for ulcerative colitis: a note of caution. Dis Colon Rectum. 1997; 40:1019–1022. PMID: 9293928.
Article143. Van Assche G, Dignass A, Bokemeyer B, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 3: special situations. J Crohns Colitis. 2013; 7:1–33. PMID: 23040453.
Article144. Sandborn WJ. Pouchitis following ileal pouch-anal anastomosis: definition, pathogenesis, and treatment. Gastroenterology. 1994; 107:1856–1860. PMID: 7958702.
Article145. Shen B, Lashner BA. Diagnosis and treatment of pouchitis. Gastroenterol Hepatol (N Y). 2008; 4:355–361. PMID: 21904509.146. Shen B, Achkar JP, Lashner BA, et al. Endoscopic and histologic evaluation together with symptom assessment are required to diagnose pouchitis. Gastroenterology. 2001; 121:261–267. PMID: 11487535.
Article147. Chiang CJ, Chen YC, Chen CJ, You SL, Lai MS. Taiwan Cancer Registry Task Force. Cancer trends in Taiwan. Jpn J Clin Oncol. 2010; 40:897–904. PMID: 20495192.
Article148. Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001; 48:526–535. PMID: 11247898.
Article149. Nuako KW, Ahlquist DA, Mahoney DW, Schaid DJ, Siems DM, Lindor NM. Familial predisposition for colorectal cancer in chronic ulcerative colitis: a case-control study. Gastroenterology. 1998; 115:1079–1083. PMID: 9797361.
Article150. Shetty K, Rybicki L, Brzezinski A, Carey WD, Lashner BA. The risk for cancer or dysplasia in ulcerative colitis patients with primary sclerosing cholangitis. Am J Gastroenterol. 1999; 94:1643–1649. PMID: 10364038.
Article151. Giardiello FM, Gurbuz AK, Bayless TM, Goodman SN, Yardley JH. Colorectal cancer in ulcerative colitis: survival in patients with and without colorectal cancer symptoms. Inflamm Bowel Dis. 1996; 2:6–10. PMID: 23282450.
Article152. Kiesslich R, Neurath MF. Advanced endoscopy imaging in inflammatory bowel diseases. Gastrointest Endosc. 2017; 85:496–508. PMID: 27816496.
Article153. Kappelman MD, Farkas DK, Long MD, et al. Risk of cancer in patients with inflammatory bowel diseases: a nationwide population-based cohort study with 30 years of follow-up evaluation. Clin Gastroenterol Hepatol. 2014; 12:265–273. PMID: 23602821.154. Cullen SN, Chapman RW. The medical management of primary sclerosing cholangitis. Semin Liver Dis. 2006; 26:52–61. PMID: 16496233.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Chemoprevention of Colitis-Associated Dysplasia or Cancer in Inflammatory Bowel Disease
- Balloon-Assisted Enteroscopy and Capsule Endoscopy in Suspected Small Bowel Crohn's Disease
- Therapeutic Drug Monitoring of Biologics for Patients with Inflammatory Bowel Diseases: How, When, and for Whom?
- Association of young age and male sex with primary sclerosing cholangitis in Taiwanese patients with inflammatory bowel disease
- Epidemiological trend in inflammatory bowel disease in Taiwan from 2001 to 2015: a nationwide populationbased study