J Pathol Transl Med.
2015 Mar;49(2):136-143. 10.4132/jptm.2015.01.03.
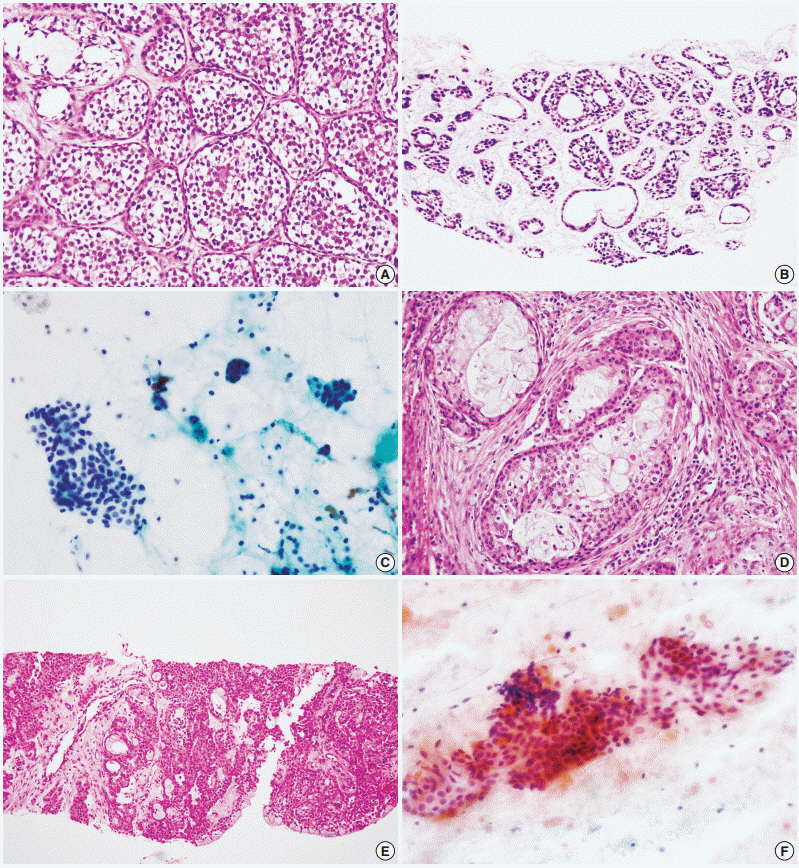
Accuracy of Core Needle Biopsy Versus Fine Needle Aspiration Cytology for Diagnosing Salivary Gland Tumors
- Affiliations
-
- 1Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. kjc@amc.seoul.kr
- 2Department of Otorhinolaryngology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2381368
- DOI: http://doi.org/10.4132/jptm.2015.01.03
Abstract
- BACKGROUND
Core needle biopsy is a relatively new technique used to diagnose salivary gland lesions, and its role in comparison with fine needle aspiration cytology needs to be refined.
METHODS
We compared the results of 228 ultrasound-guided core needle biopsy and 371 fine needle aspiration procedures performed on major salivary gland tumors with their postoperative histological diagnoses.
RESULTS
Core needle biopsy resulted in significantly higher sensitivity and more accurate tumor subtyping, especially for malignant tumors, than fine needle aspiration. No patient developed major complications after core needle biopsy.
CONCLUSIONS
We recommend ultrasoundguided core needle biopsy as the primary diagnostic tool for the preoperative evaluation of patients with salivary gland lesions, especially when malignancy is suspected.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Comprehensive Cytomorphologic Analysis of Pulmonary Adenoid Cystic Carcinoma: Comparison to Small Cell Carcinoma and Non-pulmonary Adenoid Cystic Carcinoma
Seokhwi Kim, Jinah Chu, Hojoong Kim, Joungho Han
J Pathol Transl Med. 2015;49(6):511-519. doi: 10.4132/jptm.2015.09.07.
Reference
-
1. Schmidt RL, Hall BJ, Wilson AR, Layfield LJ. A systematic review and meta-analysis of the diagnostic accuracy of fine-needle aspiration cytology for parotid gland lesions. Am J Clin Pathol. 2011; 136:45–59.
Article2. Kim BY, Hyeon J, Ryu G, et al. Diagnostic accuracy of fine needle aspiration cytology for high-grade salivary gland tumors. Ann Surg Oncol. 2013; 20:2380–7.
Article3. Tryggvason G, Gailey MP, Hulstein SL, et al. Accuracy of fine-needle aspiration and imaging in the preoperative workup of salivary gland mass lesions treated surgically. Laryngoscope. 2013; 123:158–63.
Article4. Nguansangiam S, Jesdapatarakul S, Dhanarak N, Sosrisakorn K. Accuracy of fine needle aspiration cytology of salivary gland lesions: routine diagnostic experience in Bangkok, Thailand. Asian Pac J Cancer Prev. 2012; 13:1583–8.5. Huang YT, Jung SM, Ko SF, et al. Diagnostic efficacy of ultrasonography-guided fine needle aspiration biopsy in evaluating salivary gland malignancy. Chang Gung Med J. 2012; 35:62–9.6. Kechagias N, Ntomouchtsis A, Valeri R, et al. Fine-needle aspiration cytology of salivary gland tumours: a 10-year retrospective analysis. Oral Maxillofac Surg. 2012; 16:35–40.
Article7. Piccioni LO, Fabiano B, Gemma M, Sarandria D, Bussi M. Fine-needle aspiration cytology in the diagnosis of parotid lesions. Acta Otorhinolaryngol Ital. 2011; 31:1–4.8. Cho HW, Kim J, Choi J, et al. Sonographically guided fine-needle aspiration biopsy of major salivary gland masses: a review of 245 cases. AJR Am J Roentgenol. 2011; 196:1160–3.
Article9. Schmidt RL, Hall BJ, Layfield LJ, et al. A systematic review and meta-analysis of the diagnostic accuracy of ultrasound-guided core needle biopsy for salivary gland lesions. Am J Clin Pathol. 2011; 136:516–26.
Article10. Novoa E, Gurtler N, Arnoux A, Kraft M. Role of ultrasound-guided core-needle biopsy in the assessment of head and neck lesions: a meta-analysis and systematic review of the literature. Head Neck. 2012; 34:1497–503.
Article11. Pfeiffer J, Ridder GJ. Diagnostic value of ultrasound-guided core needle biopsy in patients with salivary gland masses. Int J Oral Maxillofac Surg. 2012; 41:437–43.
Article12. Huang YC, Wu CT, Lin G, Chuang WY, Yeow KM, Wan YL. Comparison of ultrasonographically guided fine-needle aspiration and core needle biopsy in the diagnosis of parotid masses. J Clin Ultrasound. 2012; 40:189–94.
Article13. Buckland JR, Manjaly G, Violaris N, Howlett DC. Ultrasound-guided cutting-needle biopsy of the parotid gland. J Laryngol Otol. 1999; 113:988–92.
Article14. Kesse KW, Manjaly G, Violaris N, Howlett DC. Ultrasound-guided biopsy in the evaluation of focal lesions and diffuse swelling of the parotid gland. Br J Oral Maxillofac Surg. 2002; 40:384–8.
Article15. Howlett DC, Menezes LJ, Lewis K, Moody AB, Violaris N, Williams MD. Sonographically guided core biopsy of a parotid mass. AJRAm J Roentgenol. 2007; 188:223–7.
Article16. Breeze J, Andi A, Williams MD, Howlett DC. The use of fine needle core biopsy under ultrasound guidance in the diagnosis of a parotid mass. Br J Oral Maxillofac Surg. 2009; 47:78–9.
Article17. Sriskandan N, Manjaly G, Howlett DC. Re: Breeze J, Andi A, Williams MD, Howlett DC. The use of fine needle core biopsy under ultrasound guidance in the diagnosis of a parotid mass [Br. J. Oral Maxillofac. Surg. 2009;47(1):78-9]. Br J Oral Maxillofac Surg. 2009; 47:493–4.
Article18. Wan YL, Chan SC, Chen YL, et al. Ultrasonography-guided coreneedle biopsy of parotid gland masses. AJNR Am J Neuroradiol. 2004; 25:1608–12.19. Taki S, Yamamoto T, Kawai A, Terahata S, Kinuya K, Tonami H. Sonographically guided core biopsy of the salivary gland masses: safety and efficacy. Clin Imaging. 2005; 29:189–94.20. Pratap R, Qayyum A, Ahmed N, Jani P, Berman LH. Ultrasoundguided core needle biopsy of parotid gland swellings. J Laryngol Otol. 2009; 123:449–52.
Article21. Schmidt RL, Jedrzkiewicz JD, Allred RJ, Matsuoka S, Witt BL. Verification bias in diagnostic accuracy studies for fine- and core needle biopsy of salivary gland lesions in otolaryngology journals: a systematic review and analysis. Head Neck. 2014; 36:1654–61.
Article22. Roussel F, Nouvet G. Evaluation of large-needle biopsy for the diagnosis of cancer. Acta Cytol. 1995; 39:449–52.23. Witt BL, Schmidt RL. Ultrasound-guided core needle biopsy of salivary gland lesions: a systematic review and meta-analysis. Laryngoscope. 2014; 124:695–700.
Article24. Douville NJ, Bradford CR. Comparison of ultrasound-guided core biopsy versus fine-needle aspiration biopsy in the evaluation of salivary gland lesions. Head Neck. 2013; 35:1657–61.
Article25. Howlett DC. Diagnosing a parotid lump: fine needle aspiration cytology or core biopsy? Br J Radiol. 2006; 79:295–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cytologic Diagnosis of Basaloid Neoplasms of Salivary Gland
- The Role of Fine Needle Aspiration Cytology of Salivary Gland Tumors
- The Usefulness of Fine Needle Aspiration Cytology of Bone Lesions
- Quality Assuarance on Fine Needle Aspiration Cytology of Malignant Salivary Gland Neoplasms
- A Cytologic Study of Fine Needle Aspiration Biopsy of Salivary Gland Diseases