Investig Clin Urol.
2017 Jun;58(Suppl 1):S14-S22. 10.4111/icu.2017.58.S1.S14.
Critical appraisal of the top-down approach for vesicoureteral reflux
- Affiliations
-
- 1Department of Urology, University of California, Irvine, Children's Hospital of Orange County, Orange, CA, USA. aekhoury@uci.edu
- 2Department of Urology, Mansoura Urology and Nephrology Center, Mansoura University, Mansoura, Egypt.
- KMID: 2379891
- DOI: http://doi.org/10.4111/icu.2017.58.S1.S14
Abstract
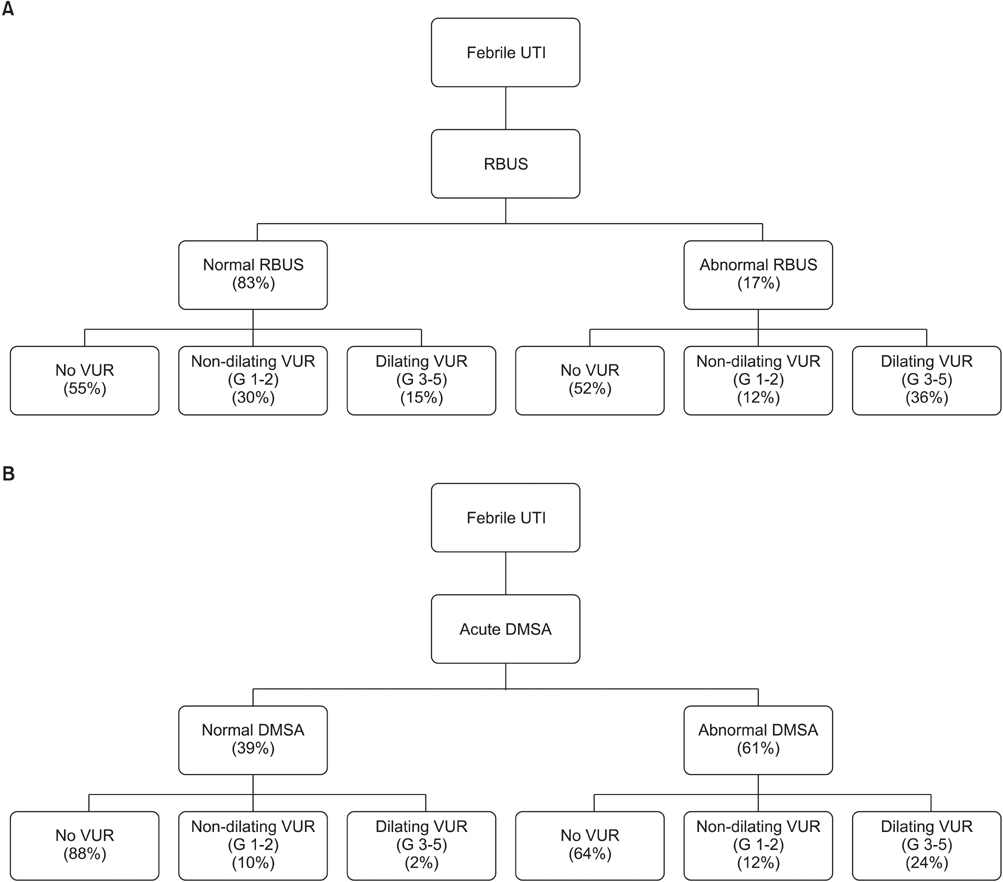
- Vesicoureteral reflux (VUR) has been linked to recurrent urinary tract infections (UTIs), renal scarring, hypertension, renal insufficiency and end-stage kidney disease. Different imaging strategies have been proposed to approach children presenting with UTI to sort out patients with significant VUR while minimizing patient morbidity, radiation exposure and financial burden. None of these imaging strategies is universally accepted. The"top-down approach" (TDA) aims at restricting the number of voiding cystourethrograms (VCUGs) and its associated morbidity while identifying patients with clinically-significant reflux. In this approach, children presenting with febrile UTIs are acutely investigated with dimercapto-succinic acid (DMSA) renal scans to identify patients with renal parenchymal inflammation. Those with evidence of renal affection are offered VCUG and late DMSA scan to identify VUR and permanent renal scarring, respectively. Although TDA could identify clinically-significant VUR with high sensitivity, it is not without limitations. The approach segregates patients based on the presence of DMSA cortical lesions omitting the morbidity and the economic burden of UTI. Additionally, some of DMSA lesions are attributed to congenital dysplasia and unrelated to UTI. Ionizing radiation exposure, financial costs, limited availability of DMSA scans in the acute setting, variability in interpreting the results and low yield of actionable findings on DMSA scans are some other limitations. In this review, we tried to address the drawbacks of the TDA and reinforce the value of patient-centered approach for VUR.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Pediatric vesicoureteral reflux: Slow but steady steps
Yong Seung Lee, Sang Won Han
Investig Clin Urol. 2017;58(Suppl 1):S1-S3. doi: 10.4111/icu.2017.58.S1.S1.Predictors of renal scars in infants with recurrent febrile urinary tract infection: a retrospective, single-center study
Jae Ha Han, Seonkyeong Rhie, Jun Ho Lee
Child Kidney Dis. 2022;26(1):52-57. doi: 10.3339/ckd.22.019.
Reference
-
1. Peters CA, Skoog SJ, Arant BS Jr, Copp HL, Elder JS, Hudson RG, et al. Summary of the AUA Guideline on Management of Primary Vesicoureteral Reflux in Children. J Urol. 2010; 184:1134–1144.2. RIVUR Trial Investigators. Hoberman A, Greenfield SP, Mattoo TK, Keren R, Mathews R, et al. Antimicrobial prophylaxis for children with vesicoureteral reflux. N Engl J Med. 2014; 370:2367–2376.3. Hidas G, Billimek J, Nam A, Soltani T, Kelly MS, Selby B, et al. Predicting the risk of breakthrough urinary tract infections: primary vesicoureteral reflux. J Urol. 2015; 194:1396–1401.4. Arlen AM, Alexander SE, Wald M, Cooper CS. Computer model predicting breakthrough febrile urinary tract infection in children with primary vesicoureteral reflux. J Pediatr Urol. 2016; 12:288.e1–288.e5.5. Keren R, Shaikh N, Pohl H, Gravens-Mueller L, Ivanova A, Zaoutis L, et al. Risk factors for recurrent urinary tract infection and renal scarring. Pediatrics. 2015; 136:e13–e21.6. Hidas G, Nam A, Soltani T, Pribish M, Watts B, Khoury AE. Primary vesico-ureteric reflux: the need for individualised risk stratification. Arab J Urol. 2013; 11:8–12.7. Baumer JH, Jones RW. Urinary tract infection in children, National Institute for Health and Clinical Excellence. Arch Dis Child Educ Pract Ed. 2007; 92:189–192.8. Subcommittee on Urinary Tract Infection, Steering Committee on Quality Improvement and Management. Roberts KB. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011; 128:595–610.9. Brader P, Riccabona M, Schwarz T, Seebacher U, Ring E. Value of comprehensive renal ultrasound in children with acute urinary tract infection for assessment of renal involvement: comparison with DMSA scintigraphy and final diagnosis. Eur Radiol. 2008; 18:2981–2989.10. Agrawalla S, Pearce R, Goodman TR. How to perform the perfect voiding cystourethrogram. Pediatr Radiol. 2004; 34:114–119.11. Riccabona M, Avni FE, Blickman JG, Dacher JN, Darge K, Lobo ML, et al. Imaging recommendations in paediatric uroradiology: minutes of the ESPR workgroup session on urinary tract infection, fetal hydronephrosis, urinary tract ultrasonography and voiding cystourethrography, Barcelona, Spain, June 2007. Pediatr Radiol. 2008; 38:138–145.12. Hansson S, Dhamey M, Sigström O, Sixt R, Stokland E, Wennerström M, et al. Dimercapto-succinic acid scintigraphy instead of voiding cystourethrography for infants with urinary tract infection. J Urol. 2004; 172:1071–1073.13. Herz D, Merguerian P, McQuiston L, Danielson C, Gheen M, Brenfleck L. 5-year prospective results of dimercapto-succinic acid imaging in children with febrile urinary tract infection: proof that the top-down approach works. J Urol. 2010; 184:4 Suppl. 1703–1709.14. Zhang X, Xu H, Zhou L, Cao Q, Shen Q, Sun L, et al. Accuracy of early DMSA scan for VUR in young children with febrile UTI. Pediatrics. 2014; 133:e30–e38.15. Hoberman A, Charron M, Hickey RW, Baskin M, Kearney DH, Wald ER. Imaging studies after a first febrile urinary tract infection in young children. N Engl J Med. 2003; 348:195–202.16. Shaikh N, Mattoo TK, Keren R, Ivanova A, Cui G, Moxey-Mims M, et al. Early antibiotic treatment for pediatric febrile urinary tract infection and renal scarring. JAMA Pediatr. 2016; 170:848–854.17. Jacobson SH, Eklöf O, Eriksson CG, Lins LE, Tidgren B, Winberg J. Development of hypertension and uraemia after pyelonephritis in childhood: 27 year follow up. BMJ. 1989; 299:703–706.18. Pohl HG, Belman AB. The “top-down” approach to the evaluation of children with febrile urinary tract infection. Adv Urol. 2009; 783409.19. Agras K, Ortapamuk H, Naldöken S, Tuncel A, Atan A. Resolution of cortical lesions on serial renal scans in children with acute pyelonephritis. Pediatr Radiol. 2007; 37:153–158.20. Parvex P, Willi JP, Kossovsky MP, Girardin E. Longitudinal analyses of renal lesions due to acute pyelonephritis in children and their impact on renal growth. J Urol. 2008; 180:2602–2606.21. Tseng MH, Lin WJ, Lo WT, Wang SR, Chu ML, Wang CC. Does a normal DMSA obviate the performance of voiding cystourethrography in evaluation of young children after their first urinary tract infection? J Pediatr. 2007; 150:96–99.22. La Scola C, De Mutiis C, Hewitt IK, Puccio G, Toffolo A, Zucchetta P, et al. Different guidelines for imaging after first UTI in febrile infants: yield, cost, and radiation. Pediatrics. 2013; 131:e665–e671.23. Craig JC, Simpson JM, Williams GJ, Lowe A, Reynolds GJ, McTaggart SJ, et al. Antibiotic prophylaxis and recurrent urinary tract infection in children. N Engl J Med. 2009; 361:1748–1759.24. Moorthy I, Easty M, McHugh K, Ridout D, Biassoni L, Gordon I. The presence of vesicoureteric reflux does not identify a population at risk for renal scarring following a first urinary tract infection. Arch Dis Child. 2005; 90:733–736.25. Merguerian PA, Jamal MA, Agarwal SK, McLorie GA, Bägli DJ, Shuckett B, et al. Utility of SPECT DMSA renal scanning in the evaluation of children with primary vesicoureteral reflux. Urology. 1999; 53:1024–1028.26. Koyle MA, Kirsch AJ, Barone CJ 2nd, Elder JS, Shifrin D, Skoog SJ, et al. Challenges in childhood urinary tract infection/vesicoureteral reflux investigation and management: calming the storm. Urology. 2012; 80:503–508.27. Winter AL, Hardy BE, Alton DJ, Arbus GS, Churchill BM. Acquired renal scars in children. J Urol. 1983; 129:1190–1194.28. Smellie JM, Poulton A, Prescod NP. Retrospective study of children with renal scarring associated with reflux and urinary infection. BMJ. 1994; 308:1193–1196.29. Craig JC, Williams GJ. Denominators do matter: it's a myth--urinary tract infection does not cause chronic kidney disease. Pediatrics. 2011; 128:984–985.30. Snodgrass WT, Shah A, Yang M, Kwon J, Villanueva C, Traylor J, et al. Prevalence and risk factors for renal scars in children with febrile UTI and/or VUR: a cross-sectional observational study of 565 consecutive patients. J Pediatr Urol. 2013; 9(6 Pt A):856–863.31. Montini G, Tullus K, Hewitt I. Febrile urinary tract infections in children. N Engl J Med. 2011; 365:239–250.32. Jodal U, Smellie JM, Lax H, Hoyer PF. Ten-year results of randomized treatment of children with severe vesicoureteral reflux. Final report of the International Reflux Study in Children. Pediatr Nephrol. 2006; 21:785–792.33. Juliano TM, Stephany HA, Clayton DB, Thomas JC, Pope JC 4th, Adams MC, et al. Incidence of abnormal imaging and recurrent pyelonephritis after first febrile urinary tract infection in children 2 to 24 months old. J Urol. 2013; 190:4 Suppl. 1505–1510.34. Bush NC, Keays M, Adams C, Mizener K, Pritzker K, Smith W, et al. Renal damage detected by DMSA, despite normal renal ultrasound, in children with febrile UTI. J Pediatr Urol. 2015; 11:126.e1–126.e7.35. Majd M, Nussbaum Blask AR, Markle BM, Shalaby-Rana E, Pohl HG, Park JS, et al. Acute pyelonephritis: comparison of diagnosis with 99mTc-DMSA, SPECT, spiral CT, MR imaging, and power Doppler US in an experimental pig model. Radiology. 2001; 218:101–108.36. Mohammadjafari H, Aalaee A, Salehifar E, Shiri A, Khademloo M, Shahmohammadi S. Doppler ultrasonography as a predictive tool for permanent kidney damage following acute pyelonephritis: comparison with dimercaptosuccinic acid scintigraphy. Iran J Kidney Dis. 2011; 5:386–391.37. Narchi H, Donovan R. Renal power Doppler ultrasound does not predict renal scarring after urinary tract infection. Scott Med J. 2008; 53:7–10.38. American Academy of Pediatrics. Committee on Quality Improvement. Subcommittee on Urinary Tract Infection. Practice parameter: the diagnosis, treatment, and evaluation of the initial urinary tract infection in febrile infants and young children. Pediatrics. 1999; 103(4 Pt 1):843–852.39. Jodal U. The natural history of bacteriuria in childhood. Infect Dis Clin North Am. 1987; 1:713–729.40. Ward VL, Strauss KJ, Barnewolt CE, Zurakowski D, Venkatakrishnan V, Fahey FH, et al. Pediatric radiation exposure and effective dose reduction during voiding cystourethrography. Radiology. 2008; 249:1002–1009.41. Tasian GE. Commentary to ‘Renal damage detected by DMSA despite normal renal ultrasound in children with febrile UTI’. J Pediatr Urol. 2015; 11:127–128.42. Ziessman HA, Majd M. Importance of methodology on (99m) technetium dimercapto-succinic acid scintigraphic image quality: imaging pilot study for RIVUR (Randomized Intervention for Children With Vesicoureteral Reflux) multicenter investigation. J Urol. 2009; 182:272–279.43. Preda I, Jodal U, Sixt R, Stokland E, Hansson S. Normal dimercaptosuccinic acid scintigraphy makes voiding cystourethrography unnecessary after urinary tract infection. J Pediatr. 2007; 151:581–584. 584.e144. Sheu JN, Wu KH, Chen SM, Tsai JD, Chao YH, Lue KH. Acute 99mTc DMSA scan predicts dilating vesicoureteral reflux in young children with a first febrile urinary tract infection: a population-based cohort study. Clin Nucl Med. 2013; 38:163–168.45. Massanyi EZ, Preece J, Gupta A, Lin SM, Wang MH. Utility of screening ultrasound after first febrile UTI among patients with clinically significant vesicoureteral reflux. Urology. 2013; 82:905–909.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Aspects of Vesicoureteral Reflux
- Endoscopic teflon injection in vesicoureteral reflux
- Clinical Observation on Vesicoureteral Reflex Following Renal Tuberculosis
- Reflux Nephropathy in Children
- A Case of High Grade Vesicoureteral Reflux in Infancy Detected Early through the Sibling Screening Test