J Rhinol.
2017 May;24(1):26-30. 10.18787/jr.2017.24.1.26.
Changes in Etiologies and Clinical Characteristics of Operated Unilateral Sinus Diseases: Comparison Study between 2005 and 2015
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, School of Medicine, Catholic University of Daegu, Daegu, Korea. miky@cu.ac.kr
- KMID: 2379786
- DOI: http://doi.org/10.18787/jr.2017.24.1.26
Abstract
- BACKGROUND AND OBJECTIVES
A considerable proportion of sinus diseases is associated with a unilateral lesion. Unilateral paranasal pathological lesions require precise preoperative diagnosis and histopathological assessment. This study aimed to analyze the changes in etiologies and clinical characteristics of operated unilateral sinus diseases between 2005 and 2015.
SUBJECTS AND METHODS
Two hundred eighteen operated cases with unilateral sinus disease in 2005 and 2015 were reviewed to retrospectively analyze the etiologies and clinical characteristics.
RESULTS
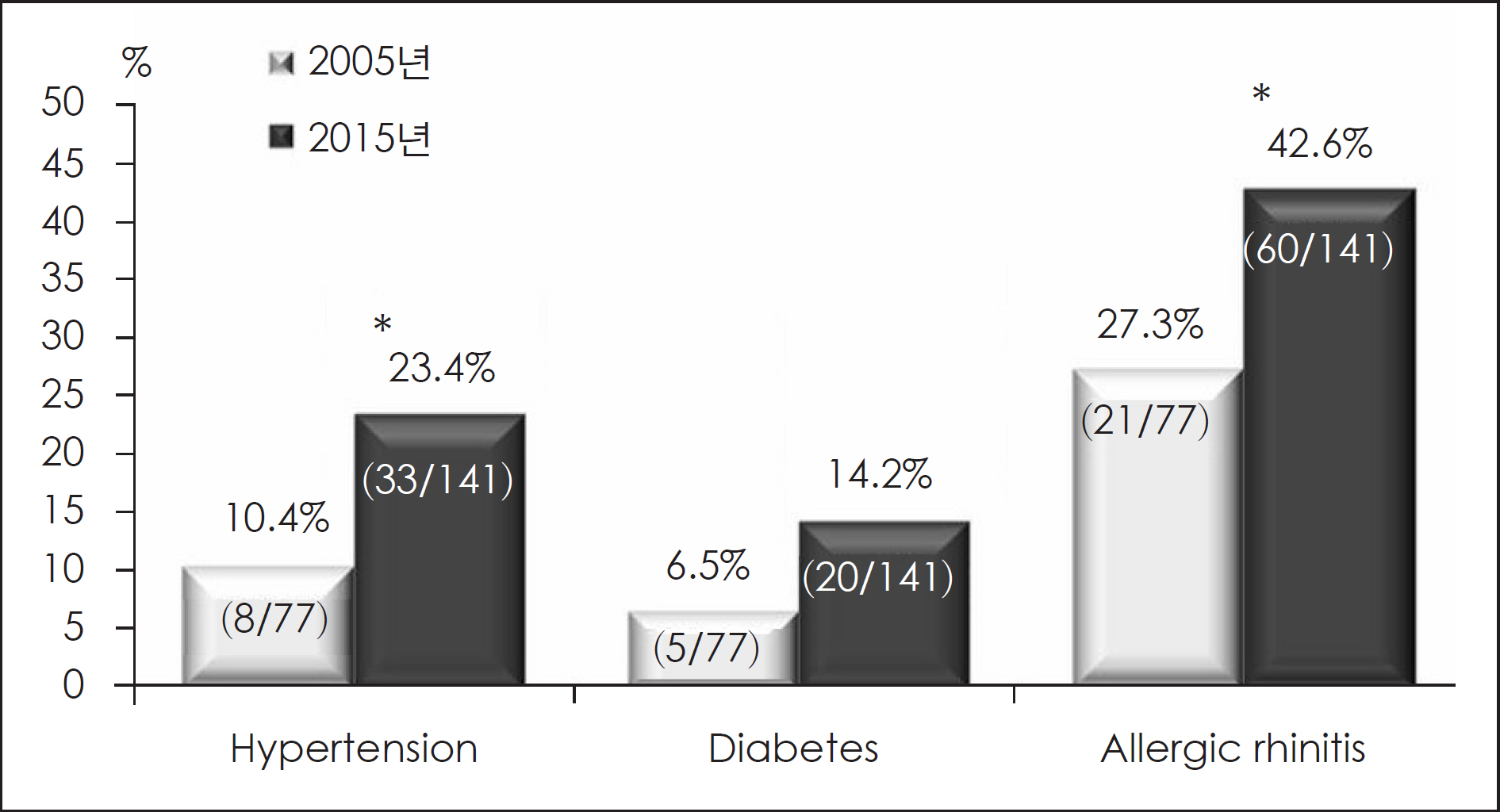
In 2015 compared with 2005, the proportion of unilateral sinus disease and patient age were increased. The proportions of patients with allergic rhinitis and hypertension were significantly increased in 2015. The leading cause of unilateral sinus lesions was nasal polyp, followed by fungus, tumor, mucocele, anatomical variation, odontogenic sinusitis, and foreign body. This ranking did not change between 2005 and 2015. The number of patients with fungal sinusitis was significantly increased in 2015. The direction of nasal septal deviation had no statistically significant relation with unilateral sinus disease.
CONCLUSION
This comparison study of unilateral sinus disease between 2005 and 2015 showed that the proportion of fungal sinusitis, patient age, and patients with underlying disease were increased.
MeSH Terms
Figure
Reference
-
1). Kim YB, Choi KS, Kang BS, Kim NP, Kim CA. Anatomical Factors Influencing Unilateral Chronic Sinusitis. Korean J Otolaryngol. 1997; 40:1109–14.2). Park KH, Lee JG, Chung SK, Hyun SJ, Park SI, Paik SI, et al. Clinical Analysis of Unilateral Lesion by Radiologic Paranasal Sinus Ex-amination. Korean J Otolaryngol. 1989; 32:40–7.3). Lee SM, Park SK, Lee SC, Eom JW, Park CK. Clinicostatistical Ob-servation on Cases with Unilateral Leisions of Maxillary Sinus. Korean J Otolaryngol. 1994; 37:1207–18.4). Troeltzsch M, Pache C, Troeltzsch M, Kaeppler G, Ehrenfeld M, Otto S, et al. Etiology and clinical characteristics of symptomatic unilateral maxillary sinusitis: A review of 174 cases. J Craniomax-illofac Surg. 2015; 43:1522–9.
Article5). Kim SW, Park YJ, Kim SW, Kang MG, Joo YH, Cho JH. A Clinical Analysis of Fungal Sinusitis. Korean J Otolaryngol. 2005; 48:332–7.6). Min YG, Lee CH, Lee JS, Song BH, Park SW, Seo SJ, et al. Unilateral sinus lesions. Korean J rhinol. 1994; 1:63–8.7). Yeo CK, Ahn BH, Kim JS, Kim YD, Shin SH, Ye MK. Fungal Ball in Sinus-Multi-Center Study in Daegu. Korean J Rhinol. 2005; 12:105–7.8). Aramani A, Karadi RN, Kumar S. A Study of Anatomical Variations of Osteomeatal Complex in Chronic Rhinosinusitis Patients-CT Findings. J Clin Diagn Res. 2014; 8:Kc01–4.9). Kapusuz Gencer Z, Ozkiris M, Okur A, Karacavus S, Saydam L. The effect of nasal septal deviation on maxillary sinus volumes and development of maxillary sinusitis. Eur Arch Otorhinolaryngol. 2013; 270:3069–73.
Article10). Park JY, Kim YS. The relationship between septal deviation and paranasal sinusitis. Korean J Otolaryngol. 1995; 38:236–9.11). Lee SJ, Shin SH, Kim CG, Ye MK, Chang HW. The Relationship between Anatomic Variation of Nasal Cavity and Paranasal Sinusitis. Korean J Otolaryngol. 2002; 45:1069–72.12). Orlandi RR. A systematic analysis of septal deviation associated with rhinosinusitis. Laryngoscope. 2010; 120:1687–95.
Article13). Prasad S, Varshney S, Bist SS, Mishra S, Kabdwal N. Correlation study between nasal septal deviation and rhinosinusitis. Indian J Otolaryngol Head Neck Surg. 2013; 65:363–6.
Article14). Kaygusuz A, Haksever M, Akduman D, Aslan S, Sayar Z. Sinonasal anatomical variations: their relationship with chronic rhinosinusitis and effect on the severity of disease-a computerized tomogra-phy assisted anatomical and clinical study. Indian J Otolaryngol Head Neck Surg. 2014; 66:260–6.
Article15). Elahi MM, Frenkiel S, Fageeh N. Paraseptal structural changes and chronic sinus disease in relation to the deviated septum. J Otolaryngol. 1997; 26:236–40.16). Yasan H, Dogru H, Baykal B, Doner F, Tuz M. What is the relationship between chronic sinus disease and isolated nasal septal deviation? Otolaryngol Head Neck Surg. 2005; 133:190–3.
Article17). Li L, Han D, Zhang L, Li Y, Zang H, Wang T, et al. Aerodynamic investigation of the correlation between nasal septal deviation and chronic rhinosinusitis. Laryngoscope. 2012; 122:1915–9.
Article18). Brook I. Sinusitis of odontogenic origin. Otolaryngol Head Neck Surg. 2006; 135:349–55.
Article19). Simuntis R, Kubilius R, Vaitkus S. Odontogenic maxillary sinusitis: a review. Stomatologija. 2014; 16:39–43.20). Matsumoto Y, Ikeda T, Yokoi H, Kohno N. Association between odontogenic infections and unilateral sinus opacification. Auris Na-sus Larynx. 2015; 42:288–93.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Pediatric Endoscopic Sinus Surgery with Antrochoanal Polyps on Sinus Growth
- Fungal Sinusitis: a Retrospective Analysis of Operated 298 Cases at a Single Medical Center, 2005–2015
- Pneumatization of the Frontal and Sphenoid Sinus in Korean Adults: A Study of Using Computed Tomography Scans
- Benign Diseases Widening the Unilateral Ethmoidal Infundibulum: Clinical and Radiological Characteristics
- Clinical Experience in Treatment of the Giant Frontal Sinus Osteoma using Cranialization