Anesth Pain Med.
2017 Apr;12(2):159-164. 10.17085/apm.2017.12.2.159.
Pretransplant diastolic wall strain assessed by transthoracic echocardiography and its implication on posttransplant survival rate in liver transplantation
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Catholic Kwandong University of Korea College of Medicine, International St. Mary's Hospital, Incheon, Korea. perhaps00@hanmail.net
- 2Department of Anesthesiology and Pain Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2379738
- DOI: http://doi.org/10.17085/apm.2017.12.2.159
Abstract
- BACKGROUND
In cirrhotic patients, left ventricular diastolic dysfunction is associated with poor outcomes. Diastolic wall strain (DWS) is a new index of left ventricular diastolic function that correlates with the myocardial stiffness. In this study, we aimed to determine whether DWS calculated from preoperative transthoracic echocardiography can predict the survival of liver transplantation recipients.
METHODS
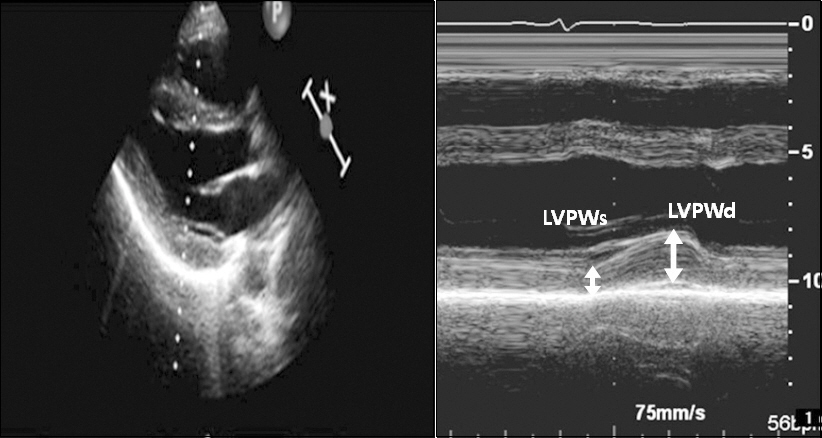
A total of 981 patients who underwent liver transplantation were enrolled. We collected the clinical, laboratory and echocardiographic data retrospectively. The left ventricular posterior wall thickness at end-systole (LVPWs) and end-diastole (LVPWd) were measured using M-mode imaging. DWS was calculated as follows: DWS = (LVPWs - LVPWd) / LVPWs. As previously reported, DWS ≤ 0.33 was defined as low DWS and DWS > 0.33 was defined as normal DWS. The primary outcome of this study was 2-years survival after liver transplantation.
RESULTS
The 2-years mortality rate following liver transplantation was higher in low DWS group than normal DWS group (14.6% vs.10.0%, P = 0.038). In univariate Cox regression analysis, age, model for end-stage liver disease score, Child-Turcotte-Pugh score, creatinine, b-type natriuretic peptide, heart rate, left ventricular end-diastolic volume index, left ventricular stroke volume index, left ventricular ejection fraction, E/A ratio, e"², E/e"² ratio, and DWS were associated with 2-years survival after liver transplantation. In multivariate Cox regression analysis, DWS was an independent predictor of 2-years survival after adjusting significant univariate covariates.
CONCLUSIONS
This study results indicated that the DWS is an independent prognostic predictor in liver transplantation recipients.
MeSH Terms
Figure
Reference
-
1. Zardi EM, Abbate A, Zardi DM, Dobrina A, Margiotta D, Van Tassell BW, et al. Cirrhotic cardiomyopathy. J Am Coll Cardiol. 2010; 56:539–49. DOI: 10.1016/j.jacc.2009.12.075. PMID: 20688208.2. Inserte J, Perelló A, Agulló L, Ruiz-Meana M, Schlüter KD, Escalona N, et al. Left ventricular hypertrophy in rats with biliary cirrhosis. Hepatology. 2003; 38:589–98. DOI: 10.1053/jhep.2003.50369. PMID: 12939585.3. Ruíz-del-Árbol L, Achécar L, Serradilla R, Rodríguez-Gandía MÁ, Rivero M, Garrido E, et al. Diastolic dysfunction is a predictor of poor outcomes in patients with cirrhosis, portal hypertension, and a normal creatinine. Hepatology. 2013; 58:1732–41. DOI: 10.1002/hep.26509. PMID: 23703953.4. Dowsley TF, Bayne DB, Langnas AN, Dumitru I, Windle JR, Porter TR, et al. Diastolic dysfunction in patients with end-stage liver disease is associated with development of heart failure early after liver transplantation. Transplantation. 2012; 94:646–51. DOI: 10.1097/TP.0b013e31825f0f97. PMID: 22918216.5. Raevens S, De Pauw M, Geerts A, Berrevoet F, Rogiers X, Troisi RI, et al. Prevalence and outcome of diastolic dysfunction in liver transplantation recipients. Acta Cardiol. 2014; 69:273–80. PMID: 25029872.6. Mittal C, Qureshi W, Singla S, Ahmad U, Huang MA. Pre-transplant left ventricular diastolic dysfunction is associated with post transplant acute graft rejection and graft failure. Dig Dis Sci. 2014; 59:674–80. DOI: 10.1007/s10620-013-2955-8. PMID: 24323177.7. Graham RJ, Gelman JS, Donelan L, Mottram PM, Peverill RE. Effect of preload reduction by haemodialysis on new indices of diastolic function. Clin Sci (Lond). 2003; 105:499–506. DOI: 10.1042/CS20030059. PMID: 12816536.8. Takeda Y, Sakata Y, Higashimori M, Mano T, Nishio M, Ohtani T, et al. Noninvasive assessment of wall distensibility with the evaluation of diastolic epicardial movement. J Card Fail. 2009; 15:68–77. DOI: 10.1016/j.cardfail.2008.09.004. PMID: 19181296.9. Ohtani T, Mohammed SF, Yamamoto K, Dunlay SM, Weston SA, Sakata Y, et al. Diastolic stiffness as assessed by diastolic wall strain is associated with adverse remodelling and poor outcomes in heart failure with preserved ejection fraction. Eur Heart J. 2012; 33:1742–9. DOI: 10.1093/eurheartj/ehs135. PMID: 22645191. PMCID: PMC3530390.10. Myers RP, Lee SS. Cirrhotic cardiomyopathy and liver transplantation. Liver Transpl. 2000; 6(4 Suppl 1):S44–52. DOI: 10.1002/lt.500060510. PMID: 10915191.11. Møller S, Henriksen JH. Cardiovascular complications of cirrhosis. Postgrad Med J. 2009; 85:44–54. PMID: 19240290.12. Ripoll C, Catalina MV, Yotti R, Olmedilla L, Pérez-Peña J, Lo Iacono O, et al. Cardiac dysfunction during liver transplantation:incidence and preoperative predictors. Transplantation. 2008; 85:1766–72. DOI: 10.1097/TP.0b013e318172c936. PMID: 18580469.13. Carvalheiro F, Rodrigues C, Adrego T, Viana J, Vieira H, Seco C, et al. Diastolic dysfunction in liver cirrhosis:prognostic predictor in liver transplantation? Transplant Proc. 2016; 48:128–31. DOI: 10.1016/j.transproceed.2016.01.010. PMID: 26915857.14. Josefsson A, Fu M, Allayhari P, Björnsson E, Castedal M, Olausson M, et al. Impact of peri-transplant heart failure &left-ventricular diastolic dysfunction on outcomes following liver transplantation. Liver Int. 2012; 32:1262–9. DOI: 10.1111/j.1478-3231.2012.02818.x. PMID: 22621679.15. Nagueh SF, Sun H, Kopelen HA, Middleton KJ, Khoury DS. Hemodynamic determinants of the mitral annulus diastolic velocities by tissue Doppler. J Am Coll Cardiol. 2001; 37:278–85. DOI: 10.1016/S0735-1097(00)01056-1.16. Liu YW, Lee WH, Lin CC, Huang YY, Lee WT, Lee CH, et al. Left ventricular diastolic wall strain and myocardial fibrosis in treated hypertension. Int J Cardiol. 2014; 172:e304–6. DOI: 10.1016/j.ijcard.2013.12.187. PMID: 24461969.17. Liu H, Gaskari SA, Lee SS. Cardiac and vascular changes in cirrhosis:pathogenic mechanisms. World J Gastroenterol. 2006; 12:837–42. DOI: 10.3748/wjg.v12.i6.837. PMID: 16521209. PMCID: PMC4066146.18. Møller S, Henriksen JH. Cardiovascular dysfunction in cirrhosis. Pathophysiological evidence of a cirrhotic cardiomyopathy. Scand J Gastroenterol. 2001; 36:785–94. DOI: 10.1080/00365520120972. DOI: 10.1080/003655201750313289. PMID: 11495071.19. Torregrosa M, Aguadé S, Dos L, Segura R, Gónzalez A, Evangelista A, et al. Cardiac alterations in cirrhosis:reversibility after liver transplantation. J Hepatol. 2005; 42:68–74. DOI: 10.1016/j.jhep.2004.09.008. PMID: 15629509.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pretransplant hepatic malignancy increases risk of de novo malignancy after liver transplantation
- De novo hepatitis B virus infection after liver transplantation from anti-hepatitis B core antibody positive donor: a 20-year experience at a single center
- Pretransplant Functional Status Predicts Postoperative Morbidity and Mortality after Liver Transplantation in Patients with Cirrhosis
- Pretransplant Hepatic Malignancy Increases Risk of De Novo Malignancy after Liver Transplantation
- Successful Pediatric ABO-Incompatible Kidney Transplantation without Pretransplant Plasmapheresis: Report of a Case