Anesth Pain Med.
2017 Apr;12(2):140-146. 10.17085/apm.2017.12.2.140.
Heart rate variability may be more useful than pulse transit time for confirming successful caudal block under general anesthesia in children
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul, Korea. dami0605@snu.ac.kr
- KMID: 2379734
- DOI: http://doi.org/10.17085/apm.2017.12.2.140
Abstract
- BACKGROUND
Confirming a successful caudal block is challenging in the pediatric population. Pulse transit time (PTT) may reflect the decrease in arterial resistance and may act as a potential indicator for confirming successful peripheral nerve or axial block. Heart rate variability (HRV) is also a possible candidate because it may be influenced by variation in sympathetic tone. We expected an increasing PTT pattern and change in HRV parameters after caudal block.
METHODS
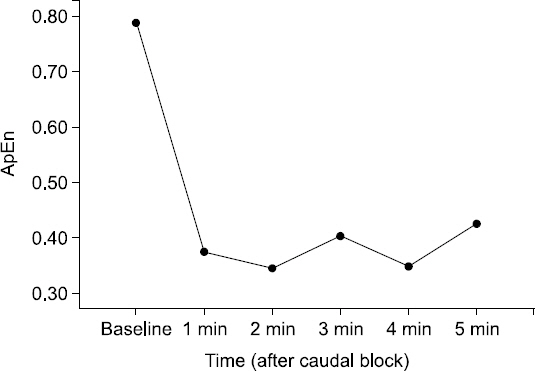
We enrolled 27 male patients (range, 1-4 years old) who were scheduled for urological surgeries. Caudal block was performed with 1 ml/kg of 0.25% ropivacaine and 1 : 200,000 epinephrine under sevoflurane anesthesia after the surgery. Successful block was confirmed by auscultation and ultrasonography. PTT and HRV parameters, such as standard deviation of normal-to-normal intervals, root mean square of successive differences, very low-frequency power, low-frequency power (LF), high-frequency power (HF), LF/HF ratio, approximate entropy (ApEn) were calculated based on electrocardiography from 1 min before to 5 min after the block. Those variables were analyzed by repeated measures analysis of variance.
RESULTS
No significant change was found in PTT with time interval after caudal block. Heart rate and ApEn of the R-R interval decreased with time interval (P = 0.001, 0.033, respectively). Some HRV parameters showed notable changes, although statistically insignificant.
CONCLUSIONS
The PTT pattern may not be an indicator for successful caudal block. However, heart rate with parameters of HRV analysis may be alternatives.
Keyword
MeSH Terms
Figure
Reference
-
1. Schuepfer G, Konrad C, Schmeck J, Poortmans G, Staffelbach B, Jöhr M. Generating a learning curve for pediatric caudal epidural blocks:an empirical evaluation of technical skills in novice and experienced anesthetists. Reg Anesth Pain Med. 2000; 25:385–8. DOI: 10.1097/00115550-200007000-00011. PMID: 10925935.2. Suresh S, Long J, Birmingham PK, De Oliveira GS Jr. Are caudal blocks for pain control safe in children?an analysis of 18,650 caudal blocks from the Pediatric Regional Anesthesia Network (PRAN) database. Anesth Analg. 2015; 120:151–6. DOI: 10.1213/ANE.0000000000000446. PMID: 25393589.3. Lewis MP, Thomas P, Wilson LF, Mulholland RC. The ‘whoosh’ test. A clinical test to confirm correct needle placement in caudal epidural injections. Anaesthesia. 1992; 47:57–8. DOI: 10.1111/j.1365-2044.1992.tb01957.x. PMID: 1536408.4. Tsui BC, Tarkkila P, Gupta S, Kearney R. Confirmation of caudal needle placement using nerve stimulation. Anesthesiology. 1999; 91:374–8. DOI: 10.1097/00000542-199908000-00010. PMID: 10443599.5. Abukawa Y, Hiroki K, Morioka N, Iwakiri H, Fukada T, Higuchi H, et al. Ultrasound versus anatomical landmarks for caudal epidural anesthesia in pediatric patients. BMC Anesthesiol. 2015; 15:102. DOI: 10.1186/s12871-015-0082-0. PMID: 26169595. PMCID: PMC4499894.6. Aydin T, Sahin L, Yaylak F. Predicting the success of caudal block. Paediatr Anaesth. 2008; 18:1117–8. DOI: 10.1111/j.1460-9592.2008.02609.x. PMID: 18950345.7. Seyedhejazi M, Moghadam A, Sharabiani BA, Golzari SE, Taghizadieh N. Success rates and complications of awake caudal versus spinal block in preterm infants undergoing inguinal hernia repair:A prospective study. Saudi J Anaesth. 2015; 9:348–52. DOI: 10.4103/1658-354X.154704. PMID: 26543447. PMCID: PMC4610074.8. Ghai B, Makkar JK, Behra BK, Rao KP. Is a fall in baseline heart rate a reliable predictor of a successful single shot caudal epidural in children? Paediatr Anaesth. 2007; 17:552–6. DOI: 10.1111/j.1460-9592.2006.02179.x. PMID: 17498017.9. Adler AC, Schwartz DA, Begley A, Friderici J, Connelly NR. Heart rate response to a caudal block in children anesthetized with sevoflurane after ultrasound confirmation of placement. Paediatr Anaesth. 2015; 25:1274–9. DOI: 10.1111/pan.12752. PMID: 26415988.10. Talwar V, Tyagi R, Mullick P, Gogia AR. Comparison of ‘whoosh’ and modified ‘swoosh’ test for identification of the caudal epidural space in children. Paediatr Anaesth. 2006; 16:134–9. DOI: 10.1111/j.1460-9592.2005.01729.x. PMID: 16430408.11. Verghese ST, Mostello LA, Patel RI, Kaplan RF, Patel KM. Testing anal sphincter tone predicts the effectiveness of caudal analgesia in children. Anesth Analg. 2002; 94:1161–4. DOI: 10.1097/00000539-200205000-00019. PMID: 11973180.12. Roberts SA, Guruswamy V, Galvez I. Caudal injectate can be reliably imaged using portable ultrasound--a preliminary study. Paediatr Anaesth. 2005; 15:948–52. DOI: 10.1111/j.1460-9592.2005.01606.x. PMID: 16238555.13. Schwartz D, Raghunathan K, Dunn S, Connelly NR. Ultrasonography and pediatric caudals. Anesth Analg. 2008; 106:97–9. DOI: 10.1213/01.ane.0000287681.41646.b8. PMID: 18165561.14. Kim YU, Cheong Y, Kong YG, Lee J, Kim S, Choi HG, et al. The prolongation of pulse transit time after a stellate ganglion block:An objective indicator of successful block. Pain Res Manag. 2015; 20:305–8. DOI: 10.1155/2015/324514. PMCID: PMC4676500.15. Babchenko A, Davidson E, Adler D, Ginosar Y, Kurz V, Nitzan M. Increase in pulse transit time to the foot after epidural anaesthesia treatment. Med Biol Eng Comput. 2000; 38:674–9. DOI: 10.1007/BF02344874. PMID: 11217886.16. Chen YQ, Jin XJ, Liu ZF, Zhu MF. Effects of stellate ganglion block on cardiovascular reaction and heart rate variability in elderly patients during anesthesia induction and endotracheal intubation. J Clin Anesth. 2015; 27:140–5. DOI: 10.1016/j.jclinane.2014.06.012. PMID: 25559299.17. Simeoforidou M, Vretzakis G, Chantzi E, Bareka M, Tsiaka K, Iatrou C, et al. Effect of interscalene brachial plexus block on heart rate variability. Korean J Anesthesiol. 2013; 64:432–8. DOI: 10.4097/kjae.2013.64.5.432. PMID: 23741566. PMCID: PMC3668105.18. Crellin D, Sullivan TP, Babl FE, O’Sullivan R, Hutchinson A. Analysis of the validation of existing behavioral pain and distress scales for use in the procedural setting. Paediatr Anaesth. 2007; 17:720–33. DOI: 10.1111/j.1460-9592.2007.02218.x. PMID: 17596217.19. Song IK, Park YH, Lee JH, Kim JT, Choi IH, Kim HS. Randomized controlled trial on preemptive analgesia for acute postoperative pain management in children. Paediatr Anaesth. 2016; 26:438–43. DOI: 10.1111/pan.12864. PMID: 26890267.20. Kang JE, Song IK, Lee JH, Hur M, Kim JT, Kim HS. Pulse transit time shows vascular changes caused by propofol in children. J Clin Monit Comput. 2015; 29:533–7. DOI: 10.1007/s10877-015-9680-0. PMID: 25750017.21. Stein PK, Bosner MS, Kleiger RE, Conger BM. Heart rate variability:a measure of cardiac autonomic tone. Am Heart J. 1994; 127:1376–81. DOI: 10.1016/0002-8703(94)90059-0.22. Toweill DL, Kovarik WD, Carr R, Kaplan D, Lai S, Bratton S, et al. Linear and nonlinear analysis of heart rate variability during propofol anesthesia for short-duration procedures in children. Pediatr Crit Care Med. 2003; 4:308–14. DOI: 10.1097/01.PCC.0000074260.93430.6A. PMID: 12831412.23. Billman GE. The LF/HF ratio does not accurately measure cardiac sympatho-vagal balance. Front Physiol. 2013; 4:26. DOI: 10.3389/fphys.2013.00026. PMID: 23431279. PMCID: PMC3576706.24. Silvetti MS, Drago F, Ragonese P. Heart rate variability in healthy children and adolescents is partially related to age and gender. Int J Cardiol. 2001; 81:169–74. DOI: 10.1016/S0167-5273(01)00537-X.