J Breast Cancer.
2017 Mar;20(1):74-81. 10.4048/jbc.2017.20.1.74.
Oncologic Outcomes after Immediate Breast Reconstruction Following Total Mastectomy in Patients with Breast Cancer: A Matched Case-Control Study
- Affiliations
-
- 1Division of Breast and Endocrine Surgery, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jeongeon.lee@samsung.com
- KMID: 2379401
- DOI: http://doi.org/10.4048/jbc.2017.20.1.74
Abstract
- PURPOSE
The use of immediate breast reconstruction (IBR) following total mastectomy (TM) has increased markedly in patients with breast cancer. As the indications for IBR have been broadened and more breast-conserving surgery-eligible patients are undergoing IBR, comparing the oncologic safety between TM only and IBR following TM becomes more difficult. This study aimed to analyze the oncologic outcomes between TM only and IBR following TM via a matched case-control methodology.
METHODS
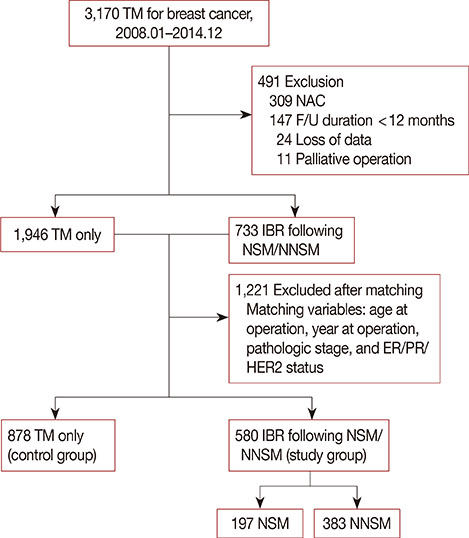
A retrospective review was conducted to identify all patients who underwent TM between 2008 and 2014. We excluded patients who underwent neoadjuvant chemotherapy, including palliative chemotherapy, and had a follow-up duration <12 months, inflammatory breast cancer, or incomplete data. We divided the remaining patients into two groups: those who underwent TM only (control group) and those who underwent IBR following TM (study group). The groups were propensity score-matched. Matched variables included age, pathologic stage, estrogen or progesterone receptor status, human epidermal growth factor receptor 2 status, and year of operation.
RESULTS
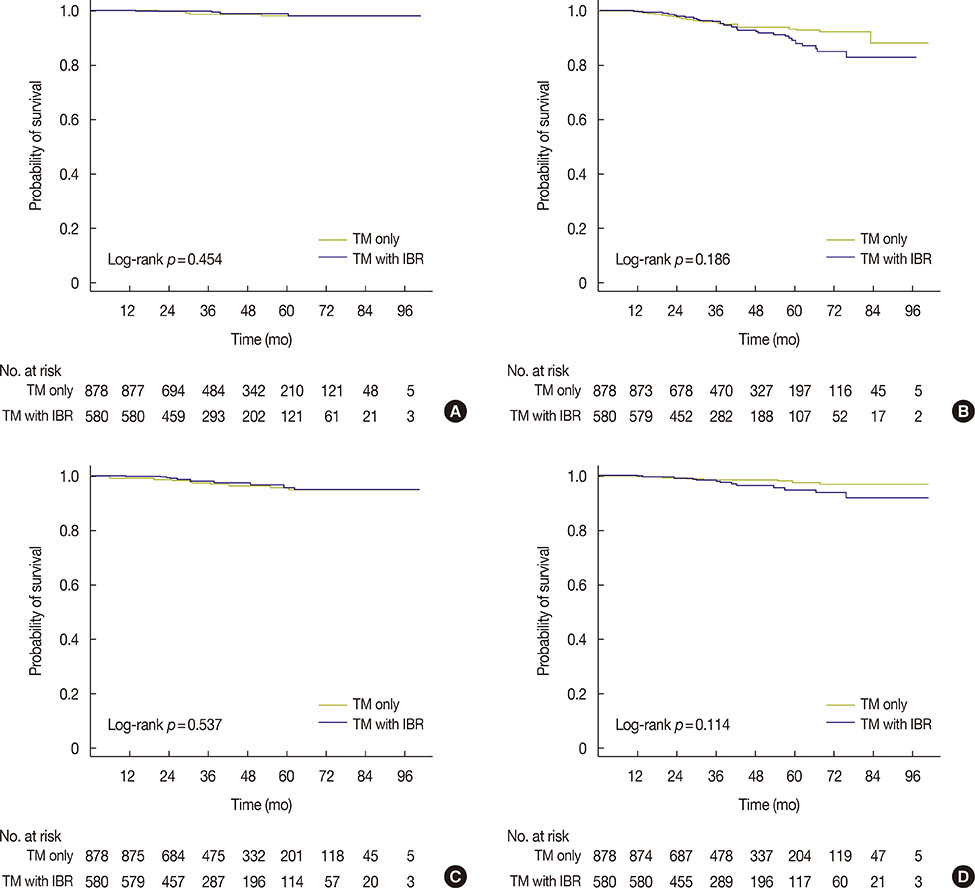
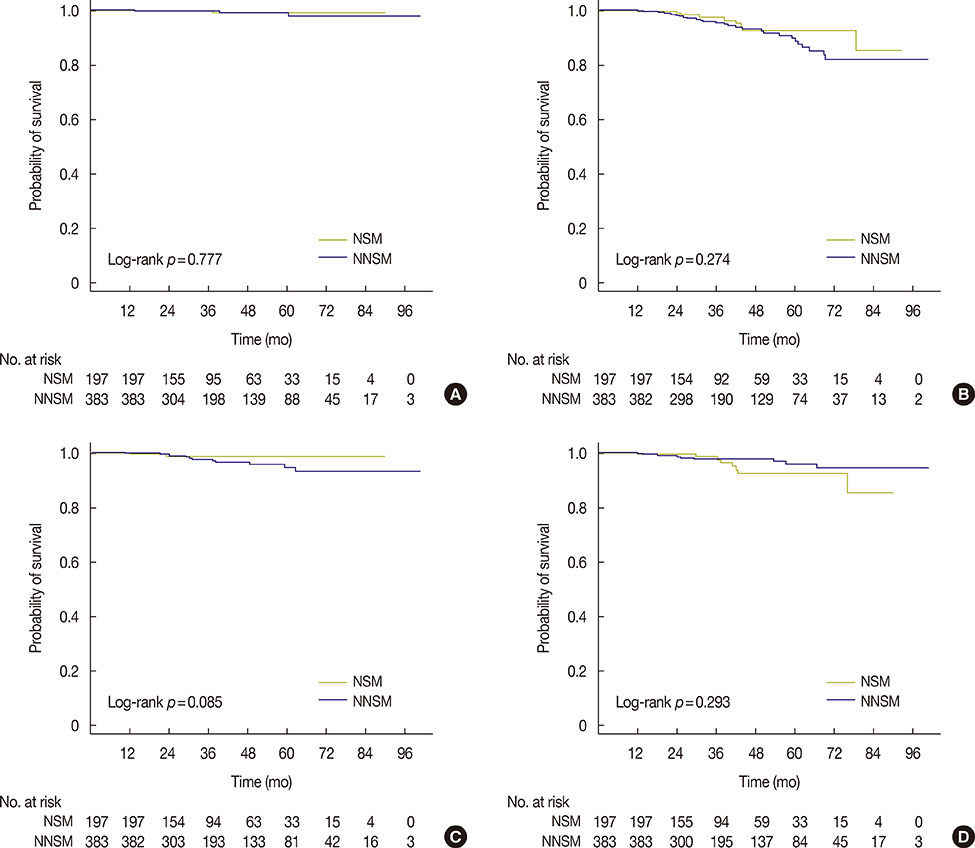
After matching, 878 patients were enrolled in the control group and 580 patients in the study group. The median follow-up duration was 43.4 months (range, 11-100 months) for the control group and 41.3 months (range, 12-100 months) for the study group (p=1.000). The mean age was 47.3±8.46 years for the control group and 43.9±7.14 years for the study group (p>0.050). Matching was considered successful for the matching variables and other factors, such as family history, histology, multiplicity, and lymphovascular invasion. There were no significant differences in overall survival (log-rank p=0.454), disease-free survival (log-rank p=0.186), local recurrence-free survival (log-rank p=0.114), or distant metastasis-free survival rates (logrank p=0.537) between the two groups.
CONCLUSION
Our results suggest that IBR following TM is a feasible treatment option for patients with breast cancer.
Keyword
MeSH Terms
-
Breast Neoplasms*
Breast*
Case-Control Studies*
Disease-Free Survival
Drug Therapy
Estrogens
Female
Follow-Up Studies
Humans
Inflammatory Breast Neoplasms
Mammaplasty*
Mastectomy, Simple*
Receptor, Epidermal Growth Factor
Receptors, Progesterone
Retrospective Studies
Survival Rate
Treatment Outcome
Estrogens
Receptor, Epidermal Growth Factor
Receptors, Progesterone
Figure
Cited by 1 articles
-
Immediate Breast Reconstruction Does Not Have a Clinically Significant Impact on Adjuvant Treatment Delay and Subsequent Survival Outcomes
Seung Ho Baek, Soon June Bae, Chang Ik Yoon, So Eun Park, Chi Hwan Cha, Sung Gwe Ahn, Young Seok Kim, Tai Suk Roh, Joon Jeong
J Breast Cancer. 2019;22(1):109-119. doi: 10.4048/jbc.2019.22.e7.
Reference
-
1. Min SY, Kim Z, Hur MH, Yoon CS, Park EH, Jung KW, et al. The basic facts of Korean breast cancer in 2013: results of a nationwide survey and breast cancer registry database. J Breast Cancer. 2016; 19:1–7.
Article2. Kummerow KL, Du L, Penson DF, Shyr Y, Hooks MA. Nationwide trends in mastectomy for early-stage breast cancer. JAMA Surg. 2015; 150:9–16.
Article3. Albornoz CR, Bach PB, Mehrara BJ, Disa JJ, Pusic AL, McCarthy CM, et al. A paradigm shift in U.S. breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013; 131:15–23.4. Toth BA, Lappert P. Modified skin incisions for mastectomy: the need for plastic surgical input in preoperative planning. Plast Reconstr Surg. 1991; 87:1048–1053.5. Duraes EF, Durand P, Duraes LC, Orra S, Moreira-Gonzalez A, Sousa JB, et al. Comparison of preoperative quality of life in breast reconstruction, breast aesthetic and non-breast plastic surgery patients: a cross-sectional study. J Plast Reconstr Aesthet Surg. 2016; 69:1478–1485.
Article6. Stanec Z, Žic R, Budi S, Stanec S, Milanović R, Vlajčić Z, et al. Skin and nipple-areola complex sparing mastectomy in breast cancer patients: 15-year experience. Ann Plast Surg. 2014; 73:485–491.
Article7. Ryu JM, Nam SJ, Kim SW, Lee SK, Bae SY, Yi HW, et al. Feasibility of nipple-sparing mastectomy with immediate breast reconstruction in breast cancer patients with tumor-nipple distance less than 2.0 cm. World J Surg. 2016; 40:2028–2035.
Article8. Krajewski AC, Boughey JC, Degnim AC, Jakub JW, Jacobson SR, Hoskin TL, et al. Expanded indications and improved outcomes for nipple-sparing mastectomy over time. Ann Surg Oncol. 2015; 22:3317–3323.
Article9. Coopey SB, Tang R, Lei L, Freer PE, Kansal K, Colwell AS, et al. Increasing eligibility for nipple-sparing mastectomy. Ann Surg Oncol. 2013; 20:3218–3222.
Article10. Lim W, Ko BS, Kim HJ, Lee JW, Eom JS, Son BH, et al. Oncological safety of skin sparing mastectomy followed by immediate reconstruction for locally advanced breast cancer. J Surg Oncol. 2010; 102:39–42.
Article11. Edge S, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC Cancer Staging Manual. 7th ed. New York: Springer;2010.12. Gradishar WJ, Anderson BO, Balassanian R, Blair SL, Burstein HJ, Cyr A, et al. Breast cancer version 2.2015. J Natl Compr Canc Netw. 2015; 13:448–475.
Article13. Zhang P, Li CZ, Wu CT, Jiao GM, Yan F, Zhu HC, et al. Comparison of immediate breast reconstruction after mastectomy and mastectomy alone for breast cancer: a meta-analysis. Eur J Surg Oncol. 2017; 43:285–293.
Article14. Kim HJ, Park EH, Lim WS, Seo JY, Koh BS, Lee TJ, et al. Nipple areola skin-sparing mastectomy with immediate transverse rectus abdominis musculocutaneous flap reconstruction is an oncologically safe procedure: a single center study. Ann Surg. 2010; 251:493–498.
Article15. De La Cruz L, Moody AM, Tappy EE, Blankenship SA, Hecht EM. Overall survival, disease-free survival, local recurrence, and nipple-areolar recurrence in the setting of nipple-sparing mastectomy: a meta-analysis and systematic review. Ann Surg Oncol. 2015; 22:3241–3249.
Article16. Sakurai T, Zhang N, Suzuma T, Umemura T, Yoshimura G, Sakurai T, et al. Long-term follow-up of nipple-sparing mastectomy without radiotherapy: a single center study at a Japanese institution. Med Oncol. 2013; 30:481.
Article17. Missana MC, Laurent I, Germain M, Lucas S, Barreau L. Long-term oncological results after 400 skin-sparing mastectomies. J Visc Surg. 2013; 150:313–320.
Article18. Platt J, Baxter NN, McLaughlin J, Semple JL. Does breast reconstruction after mastectomy for breast cancer affect overall survival? Long-term follow-up of a retrospective population-based cohort. Plast Reconstr Surg. 2015; 135:468e–476e.
Article19. Petit JY, Gentilini O, Rotmensz N, Rey P, Rietjens M, Garusi C, et al. Oncological results of immediate breast reconstruction: long term follow-up of a large series at a single institution. Breast Cancer Res Treat. 2008; 112:545–549.
Article20. Jeon YS, Kang SH, Bae YK, Lee SJ. The oncologic safety of skin sparing mastectomy with or without conservation of the nipple-areolar complex: 5 years follow up results. J Breast Cancer. 2010; 13:65–73.
Article21. Dragun AE, Huang B, Tucker TC, Spanos WJ. Increasing mastectomy rates among all age groups for early stage breast cancer: a 10-year study of surgical choice. Breast J. 2012; 18:318–325.
Article22. Agarwal J, Agarwal S, Pappas L, Neumayer L. A population-based study of breast cancer-specific survival following mastectomy and immediate or early-delayed breast reconstruction. Breast J. 2012; 18:226–232.
Article23. Agarwal S, Pappas L, Neumayer L, Agarwal J. An analysis of immediate postmastectomy breast reconstruction frequency using the surveillance, epidemiology, and end results database. Breast J. 2011; 17:352–358.
Article24. Wu W, Cheng S, Deng H, Wu J, Mao K, Cao M. Impact of breast cancer subtype defined by immunohistochemistry hormone receptor and HER2 status on the incidence of immediate postmastectomy reconstruction. Medicine (Baltimore). 2016; 95:e2547.
Article25. Bezuhly M, Temple C, Sigurdson LJ, Davis RB, Flowerdew G, Cook EF Jr. Immediate postmastectomy reconstruction is associated with improved breast cancer-specific survival: evidence and new challenges from the Surveillance, Epidemiology, and End Results database. Cancer. 2009; 115:4648–4654.
Article26. Eriksen C, Frisell J, Wickman M, Lidbrink E, Krawiec K, Sandelin K. Immediate reconstruction with implants in women with invasive breast cancer does not affect oncological safety in a matched cohort study. Breast Cancer Res Treat. 2011; 127:439–446.
Article27. Park SH, Han W, Yoo TK, Lee HB, Jin US, Chang H, et al. Oncologic safety of immediate breast reconstruction for invasive breast cancer patients: a matched case control study. J Breast Cancer. 2016; 19:68–75.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- How to optimize aesthetic outcomes in implant-based breast reconstruction
- Immediate Breast Reconstruction after a Mastectomy for Breast Cancer
- Bilateral Autologous Breast Reconstruction in a Patient with Unilateral Breast Cancer: A Case Report
- Oncologic Safety of Immediate Breast Reconstruction for Invasive Breast Cancer Patients: A Matched Case Control Study
- Study for the Efficacy and the Safety of Immediate Breast Reconstruction Following a Curative Mastectomy