Obstet Gynecol Sci.
2017 May;60(3):283-288. 10.5468/ogs.2017.60.3.283.
Primiparous singleton women with endometriosis have an increased risk of preterm birth: Meta-analyses
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Soonchunhyang University Cheonan Hospital, University of Soonchunhyang College of Medicine, Cheonan, Korea. drsook@schmc.ac.kr
- KMID: 2378590
- DOI: http://doi.org/10.5468/ogs.2017.60.3.283
Abstract
OBJECTIVE
The objective of this study was to assess the association between women with endometriosis and risk of preterm birth.
METHODS
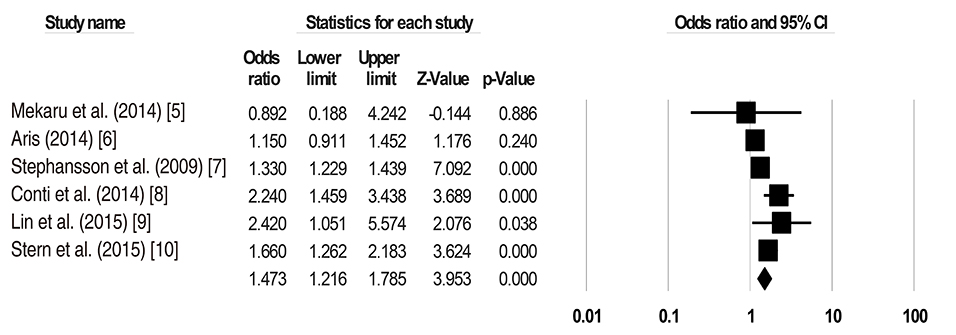
Two reviewers independently determined all prospective cohort study, retrospective cohort study, large population based cohort study, retrospective secondary analysis, and double blinded, multicentric, observational and cohort study, placebo-controlled, randomized clinical trial published using PubMed, Medline, Korea Education and Research Information Service, and Scopus from March 1994 through February 2016 without language restrictions comparing obstetric outcomes women with endometriosis and women without endometriosis. The meta-analysis was performed following the Preferred Reporting Items for Systematic Reviews and Meta-analyses statement. Six studies met inclusion criteria, including 50,472 women. Among 50,472 pregnancies, 39,659 had endometriosis and 10,813 had no endometriosis. Meta-analyses were estimated with odds ratios and 95% confidence intervals using random effect analysis according to heterogeneity of studies.
RESULTS
Data from six effect sizes from six studies involving 50,472 patients were enrolled. These meta-analyses showed women with endometriosis have an increased risk of preterm birth (odds ratio, 1.473; 95% confidence interval, 1.216 to 1.785).
CONCLUSION
These meta-analyses demonstrate women with endometriosis at pregnancy have an increased risk of preterm birth. Therefore, it is worthy for obstetrics to increase the careful inspection in women with endometriosis during pregnancy.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Women with Endometriosis, Especially Those Who Conceived with Assisted Reproductive Technology, Have Increased Risk of Placenta Previa: Meta-analyses
Hyeji Jeon, Jiwon Min, Deok Kyeong Kim, Heekyung Seo, Sunkyung Kim, Yun-Sook Kim
J Korean Med Sci. 2018;33(34):. doi: 10.3346/jkms.2018.33.e234.
Reference
-
1. Giudice LC, Kao LC. Endometriosis. Lancet. 2004; 364:1789–1799.2. Buck Louis GM, Hediger ML, Peterson CM, Croughan M, Sundaram R, Stanford J, et al. Incidence of endometriosis by study population and diagnostic method: the ENDO study. Fertil Steril. 2011; 96:360–365.3. Stratton P, Berkley KJ. Chronic pelvic pain and endometriosis: translational evidence of the relationship and implications. Hum Reprod Update. 2011; 17:327–346.4. May KE, Villar J, Kirtley S, Kennedy SH, Becker CM. Endometrial alterations in endometriosis: a systematic review of putative biomarkers. Hum Reprod Update. 2011; 17:637–653.5. Mekaru K, Masamoto H, Sugiyama H, Asato K, Heshiki C, Kinjyo T, et al. Endometriosis and pregnancy outcome: are pregnancies complicated by endometriosis a high-risk group? Eur J Obstet Gynecol Reprod Biol. 2014; 172:36–39.6. Aris A. A 12-year cohort study on adverse pregnancy outcomes in Eastern Townships of Canada: impact of endometriosis. Gynecol Endocrinol. 2014; 30:34–37.7. Stephansson O, Kieler H, Granath F, Falconer H. Endometriosis, assisted reproduction technology, and risk of adverse pregnancy outcome. Hum Reprod. 2009; 24:2341–2347.8. Conti N, Cevenini G, Vannuccini S, Orlandini C, Valensise H, Gervasi MT, et al. Women with endometriosis at first pregnancy have an increased risk of adverse obstetric outcome. J Matern Fetal Neonatal Med. 2015; 28:1795–1798.9. Lin H, Leng JH, Liu JT, Lang JH. Obstetric outcomes in Chinese women with endometriosis: a retrospective cohort study. Chin Med J (Engl). 2015; 128:455–458.10. Stern JE, Luke B, Tobias M, Gopal D, Hornstein MD, Diop H. Adverse pregnancy and birth outcomes associated with underlying diagnosis with and without assisted reproductive technology treatment. Fertil Steril. 2015; 103:1438–1445.11. Fernando S, Breheny S, Jaques AM, Halliday JL, Baker G, Healy D. Preterm birth, ovarian endometriomata, and assisted reproduction technologies. Fertil Steril. 2009; 91:325–330.12. Omland AK, Abyholm T, Fedorcsak P, Ertzeid G, Oldereid NB, Bjercke S, et al. Pregnancy outcome after IVF and ICSI in unexplained, endometriosis-associated and tubal factor infertility. Hum Reprod. 2005; 20:722–727.13. Vercellini P, Parazzini F, Pietropaolo G, Cipriani S, Frattaruolo MP, Fedele L. Pregnancy outcome in women with peritoneal, ovarian and rectovaginal endometriosis: a retrospective cohort study. BJOG. 2012; 119:1538–1543.14. Kortelahti M, Anttila MA, Hippelainen MI, Heinonen ST. Obstetric outcome in women with endometriosis--a matched case-control study. Gynecol Obstet Invest. 2003; 56:207–212.15. Benaglia L, Bermejo A, Somigliana E, Scarduelli C, Ragni G, Fedele L, et al. Pregnancy outcome in women with endometriomas achieving pregnancy through IVF. Hum Reprod. 2012; 27:1663–1667.16. Brosens I, Brosens JJ, Fusi L, Al-Sabbagh M, Kuroda K, Benagiano G. Risks of adverse pregnancy outcome in endometriosis. Fertil Steril. 2012; 98:30–35.17. Reis FM, Petraglia F, Taylor RN. Endometriosis: hormone regulation and clinical consequences of chemotaxis and apoptosis. Hum Reprod Update. 2013; 19:406–418.18. Zanatta A, Pereira RM, Rocha AM, Cogliati B, Baracat EC, Taylor HS, et al. The relationship among HOXA10, estrogen receptor α, progesterone receptor, and progesterone receptor B proteins in rectosigmoid endometriosis: a Tissue Microarray Study. Reprod Sci. 2015; 22:31–37.19. Leone Roberti Maggiore U, Ferrero S, Mangili G, Bergamini A, Inversetti A, Giorgione V, et al. A systematic review on endometriosis during pregnancy: diagnosis, misdiagnosis, complications and outcomes. Hum Reprod Update. 2016; 22:70–103.20. Hayashi M, Nakai A, Satoh S, Matsuda Y. Adverse obstetric and perinatal outcomes of singleton pregnancies may be related to maternal factors associated with infertility rather than the type of assisted reproductive technology procedure used. Fertil Steril. 2012; 98:922–928.21. Aznaurova YB, Zhumataev MB, Roberts TK, Aliper AM, Zhavoronkov AA. Molecular aspects of development and regulation of endometriosis. Reprod Biol Endocrinol. 2014; 12:50.22. Vigano P, Corti L, Berlanda N. Beyond infertility: obstetrical and postpartum complications associated with endometriosis and adenomyosis. Fertil Steril. 2015; 104:802–812.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Women with Endometriosis, Especially Those Who Conceived with Assisted Reproductive Technology, Have Increased Risk of Placenta Previa: Meta-analyses
- Effect of First Birth Interval Length on Preterm of Singleton Birth in Korea; 2010-2013
- Cervical Length Measurement to Predict Preterm Birth: Clinical Application and Treatment Modalities
- How to screen the cervix and reduce the risk of spontaneous preterm birth in asymptomatic women without a prior preterm birth
- Analysis of Preterm Birth Rate based on Birth Certificate Data: from 1995 to 2003