Korean J Neurotrauma.
2017 Apr;13(1):15-23. 10.13004/kjnt.2017.13.1.15.
Comparison of Complications Following Cranioplasty Using a Sterilized Autologous Bone Flap or Polymethyl Methacrylate
- Affiliations
-
- 1Department of Neurosurgery, Seoul Medical Center, Seoul, Korea. kangds3436@daum.net
- 2Department of Neurosurgery, Hanyang University Guri Hospital, Guri, Korea.
- KMID: 2378245
- DOI: http://doi.org/10.13004/kjnt.2017.13.1.15
Abstract
OBJECTIVE
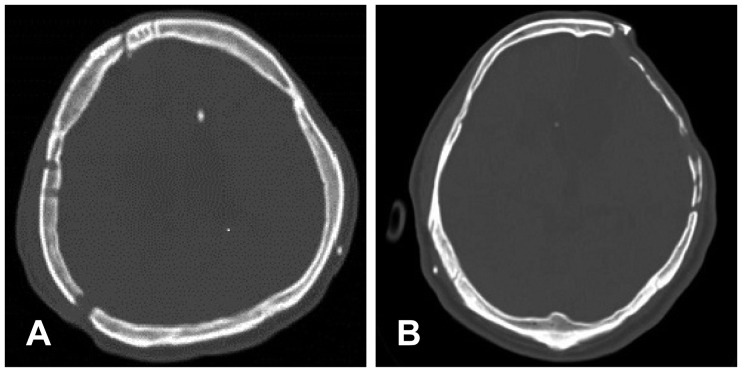
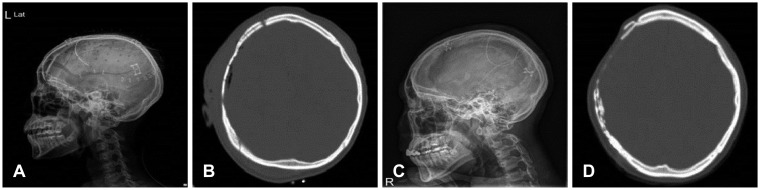
The aims of current study are to compare complications following cranioplasty (CP) using either sterilized autologous bone or polymethyl methacrylate (PMMA), and to identify the risk factors for two of the most common complications: bone flap resorption (BFR) and surgical site infection (SSI).
METHODS
Between January 2004 and December 2013, 127 patients underwent CP and were followed at least 12 months. Variables, including sex, age, initial diagnosis, time interval between decompressive craniectomy (DC) and CP, operation time, size of bone flap, and presence of ventriculo-peritoneal shunt, were analyzed to identify the risk factors for BFR and SSI.
RESULTS
A total of 97 (76.4%) patients underwent CP using PMMA (Group I) and 30 (23.6%) underwent CP using autologous bone (Group II). SSI occurred in 8 (8.2%) patients in Group I, and in 2 (6.7%) in Group II; there was no statistically significant difference between the groups (p=1.00). No statistically significant risk factors for SSI were found in either group. In Group I, there was no reported case of BFR. In Group II patients, BFR developed in 18 (60.0%) patients at the time of CP (Type 1 BFR), and at 12-month follow up (Type 2 BFR) in 4 (13.3%) patients. No statistically significant risk factors for BFR were found in Group II.
CONCLUSION
CP using sterilized autologous bone result in a significant rate of BFR. PMMA, however, is a safe alloplastic material for CP, as it has low complication rate.
MeSH Terms
Figure
Reference
-
1. Arun Kumar KV, Singla NK, Gowda ME, Kumar D, Legha VS. Current concepts in restoring acquired cranial defects. J Indian Prosthodont Soc. 2014; 14:14–17. PMID: 26199486.
Article2. Blum KS, Schneider SJ, Rosenthal AD. Methyl methacrylate cranioplasty in children: long-term results. Pediatr Neurosurg. 1997; 26:33–35. PMID: 9361115.
Article3. Bobinski L, Koskinen LO, Lindvall P. Complications following cranioplasty using autologous bone or polymethylmethacrylate--retrospective experience from a single center. Clin Neurol Neurosurg. 2013; 115:1788–1791. PMID: 23725651.
Article4. Bowers CA, Riva-Cambrin J, Hertzler DA 2nd, Walker ML. Risk factors and rates of bone flap resorption in pediatric patients after decompressive craniectomy for traumatic brain injury. J Neurosurg Pediatr. 2013; 11:526–532. PMID: 23473303.
Article5. Chang V, Hartzfeld P, Langlois M, Mahmood A, Seyfried D. Outcomes of cranial repair after craniectomy. J Neurosurg. 2010; 112:1120–1124. PMID: 19612971.
Article6. Cheng YK, Weng HH, Yang JT, Lee MH, Wang TC, Chang CN. Factors affecting graft infection after cranioplasty. J Clin Neurosci. 2008; 15:1115–1119. PMID: 18656363.
Article7. De Bonis P, Frassanito P, Mangiola A, Nucci CG, Anile C, Pompucci A. Cranial repair: how complicated is filling a “hole”? J Neurotrauma. 2012; 29:1071–1076. PMID: 22059899.
Article8. Dünisch P, Walter J, Sakr Y, Kalff R, Waschke A, Ewald C. Risk factors of aseptic bone resorption: a study after autologous bone flap reinsertion due to decompressive craniotomy. J Neurosurg. 2013; 118:1141–1147. PMID: 23451904.
Article9. Gooch MR, Gin GE, Kenning TJ, German JW. Complications of cranioplasty following decompressive craniectomy: analysis of 62 cases. Neurosurg Focus. 2009; 26:E9.
Article10. Grant GA, Jolley M, Ellenbogen RG, Roberts TS, Gruss JR, Loeser JD. Failure of autologous bone-assisted cranioplasty following decompressive craniectomy in children and adolescents. J Neurosurg. 2004; 100:163–168. PMID: 14758944.
Article11. Hallfeldt KK, Stutzle H, Puhlmann M, Kessler S, Schweiberer L. Sterilization of partially demineralized bone matrix: the effects of different sterilization techniques on osteogenetic properties. J Surg Res. 1995; 59:614–620. PMID: 7475009.
Article12. Hammon WM, Kempe LG. Methyl methacrylate cranioplasty. 13 years experience with 417 patients. Acta Neurochir (Wien). 1971; 25:69–77. PMID: 5135756.13. Kim H, Sung SO, Kim SJ, Kim SR, Park IS, Jo KW. Analysis of the factors affecting graft infection after cranioplasty. Acta Neurochir (Wien). 2013; 155:2171–2176. PMID: 24043415.
Article14. Kim JS, Cheong JH, Ryu JI, Kim JM, Kim CH. Bone flap resorption following cranioplasty after decompressive craniectomy: preliminary report. Korean J Neurotrauma. 2015; 11:1–5. PMID: 27169057.
Article15. Lee CH, Chung YS, Lee SH, Yang HJ, Son YJ. Analysis of the factors influencing bone graft infection after cranioplasty. J Trauma Acute Care Surg. 2012; 73:255–260. PMID: 22743392.
Article16. Martin KD, Franz B, Kirsch M, Polanski W, von der Hagen M, Schackert G, et al. Autologous bone flap cranioplasty following decompressive craniectomy is combined with a high complication rate in pediatric traumatic brain injury patients. Acta Neurochir (Wien). 2014; 156:813–824. PMID: 24532225.
Article17. Matsuno A, Tanaka H, Iwamuro H, Takanashi S, Miyawaki S, Nakashima M, et al. Analyses of the factors influencing bone graft infection after delayed cranioplasty. Acta Neurochir (Wien). 2006; 148:535–540. PMID: 16467959.
Article18. Meyer MJ, Megyesi J, Meythaler J, Murie-Fernandez M, Aubut JA, Foley N, et al. Acute management of acquired brain injury part I: an evidence-based review of non-pharmacological interventions. Brain Inj. 2010; 24:694–705. PMID: 20353284.
Article19. Moreira-Gonzalez A, Jackson IT, Miyawaki T, Barakat K, DiNick V. Clinical outcome in cranioplasty: critical review in long-term follow-up. J Craniofac Surg. 2003; 14:144–153. PMID: 12621283.
Article20. Mracek J, Hommerova J, Mork J, Richtr P, Priban V. Complications of cranioplasty using a bone flap sterilised by autoclaving following decompressive craniectomy. Acta Neurochir (Wien). 2015; 157:501–506. PMID: 25588749.
Article21. Osawa M, Hara H, Ichinose Y, Koyama T, Kobayashi S, Sugita Y. Cranioplasty with a frozen and autoclaved bone flap. Acta Neurochir (Wien). 1990; 102:38–41. PMID: 2305650.
Article22. Park JS, Lee KS, Shim JJ, Yoon SM, Choi WR, Doh JW. Large defect may cause infectious complications in cranioplasty. J Korean Neurosurg Soc. 2007; 42:89–91.23. Sahuquillo J, Arikan F. Decompressive craniectomy for the treatment of refractory high intracranial pressure in traumatic brain injury. Cochrane Database Syst Rev. 2006; (1):CD003983. PMID: 16437469.
Article24. Sakamoto S, Eguchi K, Kiura Y, Arita K, Kurisu K. CT perfusion imaging in the syndrome of the sinking skin flap before and after cranioplasty. Clin Neurol Neurosurg. 2006; 108:583–585. PMID: 15921849.
Article25. Schuss P, Vatter H, Marquardt G, Imöhl L, Ulrich CT, Seifert V, et al. Cranioplasty after decompressive craniectomy: the effect of timing on postoperative complications. J Neurotrauma. 2012; 29:1090–1095. PMID: 22201297.
Article26. Schuss P, Vatter H, Oszvald A, Marquardt G, Imöhl L, Seifert V, et al. risk factors for the development of a long-term complication following cranioplasty after decompressive craniectomy. J Neurotrauma. 2013; 30:91–95. PMID: 22970998.27. Schwab S, Steiner T, Aschoff A, Schwarz S, Steiner HH, Jansen O, et al. Early hemicraniectomy in patients with complete middle cerebral artery infarction. Stroke. 1998; 29:1888–1893. PMID: 9731614.
Article28. Schwarz F, Dunisch P, Walter J, Sakr Y, Kalff R, Ewald C. Cranioplasty after decompressive craniectomy: is there a rationale for an initial artificial bone-substitute implant? A single-center experience after 631 procedures. J Neurosurg. 2016; 124:710–715. PMID: 26406796.
Article29. Sobani ZA, Shamim MS, Zafar SN, Qadeer M, Bilal N, Murtaza SG, et al. Cranioplasty after decompressive craniectomy: An institutional audit and analysis of factors related to complications. Surg Neurol Int. 2011; 2:123. PMID: 22059118.
Article30. Sundseth J, Sundseth A, Berg-Johnsen J, Sorteberg W, Lindegaard KF. Cranioplasty with autologous cryopreserved bone after decompressive craniectomy: complications and risk factors for developing surgical site infection. Acta Neurochir (Wien). 2014; 156:805–811. discussion 811. PMID: 24493001.
Article31. Tokoro K, Chiba Y, Tsubone K. Late infection after cranioplasty-review of 14 cases. Neurol Med Chir (Tokyo). 1989; 29:196–201. PMID: 2477724.32. Walcott BP, Kwon CS, Sheth SA, Fehnel CR, Koffie RM, Asaad WF, et al. Predictors of cranioplasty complications in stroke and trauma patients. J Neurosurg. 2013; 118:757–762. PMID: 23394335.
Article33. Winkler PA, Stummer W, Linke R, Krishnan KG, Tatsch K. Influence of cranioplasty on postural blood flow regulation, cerebrovascular reserve capacity, and cerebral glucose metabolism. J Neurosurg. 2000; 93:53–61.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Large Defect May Cause Infectious Complications in Cranioplasty
- Cranioplasty Using Frozen Autologous Bone
- Comparison with Subcutaneous Abdominal Preservation and Cryoconservation Using Autologous Bone Flap after Decompressive Craniectomy
- Late seroma and infection in patients with cranioplasty implants after lateral suboccipital craniectomy
- Analysis of Cranioplasty Using Frozen Autologous Bone Following Post-Traumatic Decompressive Craniectomy