J Cerebrovasc Endovasc Neurosurg.
2017 Mar;19(1):19-35. 10.7461/jcen.2017.19.1.19.
Surgical Approaches for Symptomatic Cerebral Cavernous Malformations of the Thalamus and Brainstem
- Affiliations
-
- 1Department of Neurosurgery, University of Virginia, Charlottesville, VA, USA. dmd7q@hscmail.mcc.virginia.edu
- 2Department of Neurological Surgery, University of Miami, Miami, FL, USA.
- 3Department of Neurological Surgery, Rush University, Chicago, IL, USA.
- 4Department of Radiology and Medical Imaging, University of Virginia, Charlottesville, VA, USA.
- KMID: 2377623
- DOI: http://doi.org/10.7461/jcen.2017.19.1.19
Abstract
OBJECTIVE
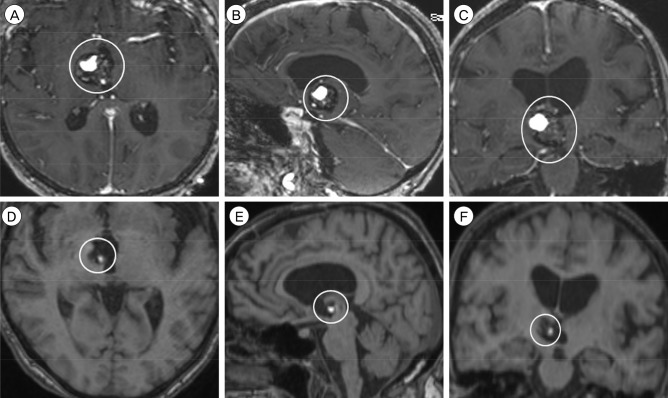
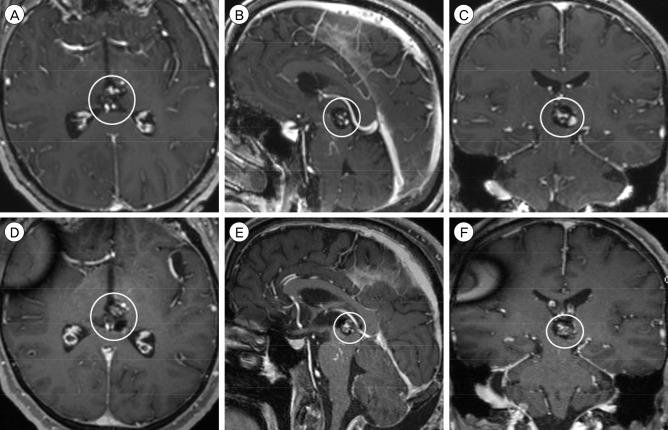
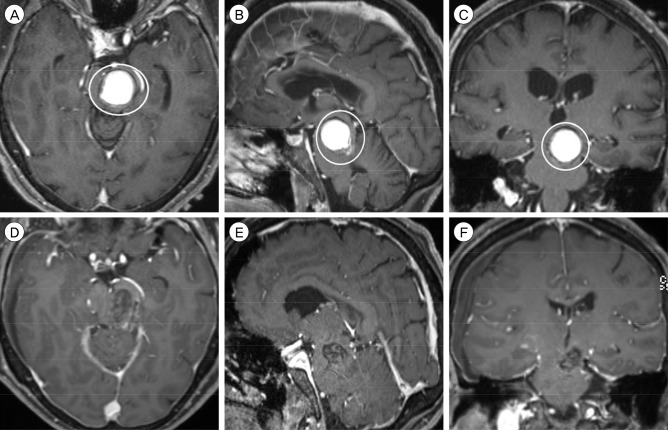
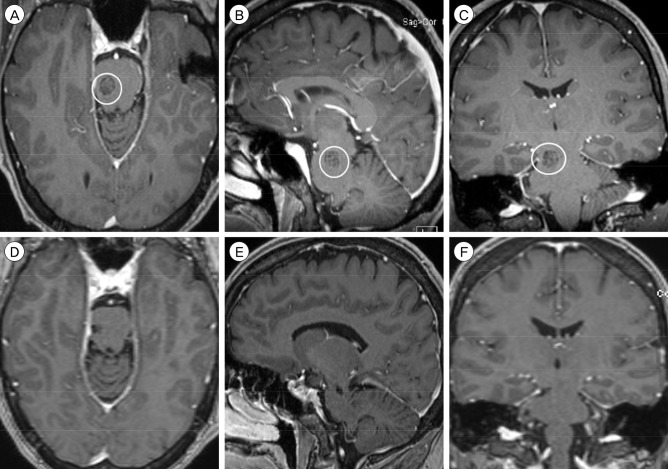
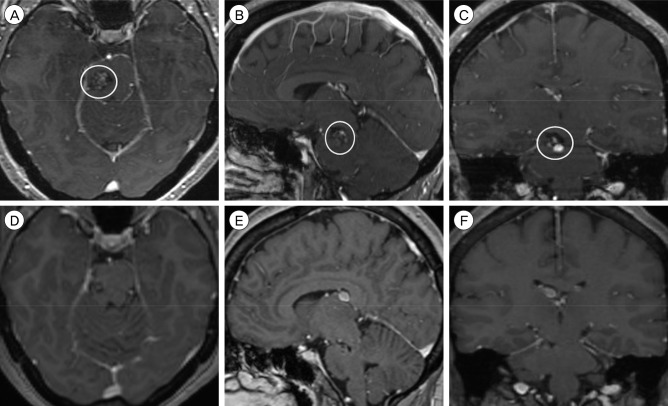
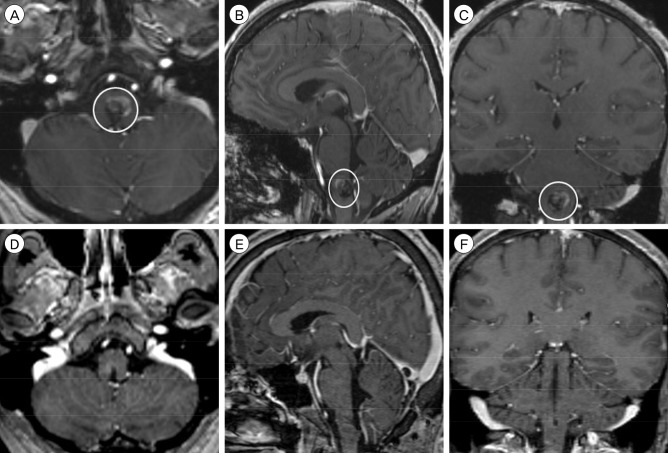
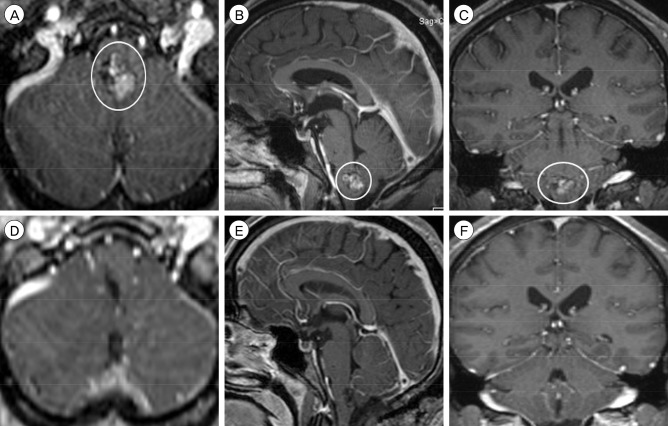
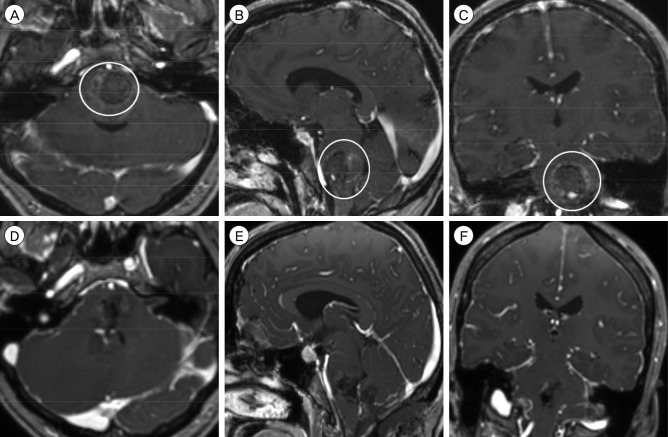
Surgical resection of thalamic and brainstem cerebral cavernous malformations (CCMs) is associated with significant operative morbidity, but it may be outweighed, in some cases, by the neurological damage from recurrent hemorrhage in these eloquent areas. The goals of this retrospective cohort study are to describe the technical nuances of surgical approaches and determine the postoperative outcomes for CCMs of the thalamus and brainstem.
MATERIALS AND METHODS
We reviewed an institutional database of patients harboring thalamic or brainstem CCMs, who underwent surgical resection from 2010 to 2014. The baseline and follow-up neuroimaging and clinical findings of each patient and the operative details of each case were evaluated.
RESULTS
A total of eight patients, including two with thalamic and six with brainstem CCMs, were included in the study cohort. All patients had progressive neurological deterioration from recurrent CCM hemorrhage, and the median modified Rankin Scale (mRS) at presentation was 3. The median CCM maximum diameter and volume were 1.7 cm and 1.8 cm³, respectively. The thalamic CCMs were resected using the anterior transcallosal transchoroidal and supracerebellar infratentorial approaches each in one case (13%). The brainstem CCMs were resected using the retrosigmoid and suboccipital trans-cerebellomedullary fissure approaches each in three cases (38%). After a median follow-up of 11.5 months, all patients were neurologically stable or improved, with a median mRS of 2. The rate of functional independence (mRS 0-2) was 63%.
CONCLUSION
Microneurosurgical techniques and approaches can be safely and effectively employed for the management of thalamic and brainstem CCMs in appropriately selected patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Abla AA, Turner JD, Mitha AP, Lekovic G, Spetzler RF. Surgical approaches to brainstem cavernous malformations. Neurosurg Focus. 2010; 9. 29(3):E8.
Article2. Aiba T, Tanaka R, Koike T, Kameyama S, Takeda N, Komata T. Natural history of intracranial cavernous malformations. J Neurosurg. 1995; 7. 83(1):56–59. PMID: 7782850.
Article3. Awad AJ, Walcott BP, Stapleton CJ, Ding D, Lee CC, Loeffler JS. Repeat radiosurgery for cerebral arteriovenous malformations. J Clin Neurosci. 2015; 6. 22(6):945–950. PMID: 25913746.
Article4. Barker FG 2nd, Amin-Hanjani S, Butler WE, Lyons S, Ojemann RG, Chapman PH, et al. Temporal clustering of hemorrhages from untreated cavernous malformations of the central nervous system. Neurosurgery. 2001; 7. 49(1):15–24. discussion 24-5. PMID: 11440436.
Article5. Buell TJ, Ding D, Starke RM, Webster Crowley R, Liu KC. Embolization-induced angiogenesis in cerebral arteriovenous malformations. J Clin Neurosci. 2014; 11. 21(11):1866–1871. PMID: 25001989.
Article6. Chen CJ, Chivukula S, Ding D, Starke RM, Lee CC, Yen CP, et al. Seizure outcomes following radiosurgery for cerebral arteriovenous malformations. Neurosurg Focus. 2014; 9. 37(3):E17.
Article7. Clatterbuck RE, Moriarity JL, Elmaci I, Lee RR, Breiter SN, Rigamonti D. Dynamic nature of cavernous malformations: a prospective magnetic resonance imaging study with volumetric analysis. J Neurosurg. 2000; 12. 93(6):981–986. PMID: 11117871.
Article8. Cohen-Inbar O, Ding D, Chen CJ, Sheehan JP. Stereotactic radiosurgery for deep intracranial arteriovenous malformations, part 1: brainstem arteriovenous malformations. J Clin Neurosci. 2016; 2. 24:30–36. PMID: 26740034.
Article9. Cohen-Inbar O, Ding D, Sheehan JP. Stereotactic radiosurgery for deep intracranial arteriovenous malformations, part 2 basal ganglia and thalamus arteriovenous malformations. J Clin Neurosci. 2016; 2. 24:37–42. PMID: 26732284.
Article10. Conger JR, Ding D, Raper DM, Starke RM, Durst CR, Liu KC, et al. Preoperative embolization of cerebral arteriovenous malformations with silk suture and particles: technical considerations and outcomes. J Cerebrovasc Endovasc Neurosurg. 2016; 6. 18(2):90–99. PMID: 27790398.
Article11. de Oliveira JG, Lekovic GP, Safavi-Abbasi S, Reis CV, Hanel RA, Porter RW, et al. Supracerebellar infratentorial approach to cavernous malformations of the brainstem: surgical variants and clinical experience with 45 patients. Neurosurgery. 2010; 2. 66(2):389–399. PMID: 20042987.12. Ding D. Mechanisms of cyst formation after radiosurgery for intracranial arteriovenous malformations. Clin Neurol Neurosurg. 2014; 9. 124:192–193. PMID: 25070227.
Article13. Ding D. Pathogenesis of radiosurgery-induced cyst formation in patients with cerebral arteriovenous malformations. Acta Neurochir (Wien). 2015; 5. 157(5):775–777. PMID: 25749841.
Article14. Ding D, Liu KC. Predictive capability of the Spetzler-Martin versus supplementary grading scale for microsurgical outcomes of cerebellar arteriovenous malformations. J Cerebrovasc Endovasc Neurosurg. 2013; 12. 15(4):307–310. PMID: 24729957.
Article15. Ding D, Quigg M, Starke RM, Xu Z, Yen CP, Przybylowski CJ, et al. Radiosurgery for temporal lobe arteriovenous malformations: effect of temporal location on seizure outcomes. J Neurosurg. 2015; 10. 123(4):924–934. PMID: 25884262.
Article16. Ding D, Quigg M, Starke RM, Yen CP, Przybylowski CJ, Dodson BK, et al. Cerebral arteriovenous malformations and epilepsy, part 2: predictors of seizure outcomes following radiosurgery. World Neurosurg. 2015; 9. 84(3):653–662. PMID: 26026628.
Article17. Ding D, Sheehan JP, Starke RM, Durst CR, Raper DM, Conger JR, et al. Embolization of cerebral arteriovenous malformations with silk suture particles prior to stereotactic radiosurgery. J Clin Neurosci. 2015; 10. 22(10):1643–1649. PMID: 26186966.
Article18. Ding D, Starke RM, Kano H, Lee JY, Mathieu D, Pierce J, et al. Stereotactic radiosurgery for Spetzler-Martin Grade III arteriovenous malformations: an international multicenter study. J Neurosurg. 2017; 3. 126(3):859–871. PMID: 27081906.
Article19. Ding D, Starke RM, Kano H, Mathieu D, Huang P, Kondziolka D, et al. Radiosurgery for cerebral arteriovenous malformations in a randomized trial of unruptured brain arteriovenous malformations (ARUBA)-eligible patients: a multicenter study. Stroke. 2016; 2. 47(2):342–349. PMID: 26658441.20. Ding D, Starke RM, Kano H, Mathieu D, Huang PP, Feliciano C, et al. International multicenter cohort study of pediatric brain arteriovenous malformations. Part 1: predictors of hemorrhagic presentation. J Neurosurg Pediatr. 2017; 2. 19(2):127–135. PMID: 27911248.
Article21. Ding D, Starke RM, Kano H, Mathieu D, Huang PP, Kondziolka D, et al. Stereotactic radiosurgery for a randomized trial of unruptured brain arteriovenous malformations (ARUBA)-Eligible Spetzler-Martin Grade I and II arteriovenous malformations: a multicenter study. World Neurosurg. 2017; 3. 23. [Epub ahead of print].22. Ding D, Starke RM, Liu KC, Crowley RW. Cortical plasticity in patients with cerebral arteriovenous malformations. J Clin Neurosci. 2015; 12. 22(12):1857–1861. PMID: 26256067.
Article23. Ding D, Starke RM, Quigg M, Yen CP, Przybylowski CJ, Dodson BK, et al. Cerebral arteriovenous malformations and epilepsy, part 1: predictors of seizure presentation. World Neurosurg. 2015; 9. 84(3):645–652. PMID: 25753234.
Article24. Ding D, Starke RM, Crowley RW, Liu KC. Endoport-assisted microsurgical resection of cerebral cavernous malformations. J Clin Neurosci. 2015; 6. 22(6):1025–1029. PMID: 25769248.
Article25. Ding D, Starke RM, Yen CP, Sheehan JP. Radiosurgery for cerebellar arteriovenous malformations: does infratentorial location affect outcome? World Neurosurg. 2014; Jul-Aug. 82(1-2):e209–e217. PMID: 24530455.
Article26. Ding D, Xu Z, Shih HH, Starke RM, Yen CP, Cohen-Inbar O, et al. Worse outcomes after repeat vs initial stereotactic radiosurgery for cerebral arteriovenous malformations: a retrospective matched-cohort study. Neurosurgery. 2016; 11. 79(5):690–700. PMID: 27759676.27. Ding D, Xu Z, Shih HH, Starke RM, Yen CP, Sheehan JP. Stereotactic radiosurgery for partially resected cerebral arteriovenous malformations. World Neurosurg. 2016; 1. 85:263–272. PMID: 26459698.
Article28. Ding D, Xu Z, Starke RM, Yen CP, Shih HH, Buell TJ, et al. Radiosurgery for cerebral arteriovenous malformations with associated arterial aneurysms. World Neurosurg. 2016; 3. 87:77–90. PMID: 26732956.
Article29. Ding D, Xu Z, Yen CP, Starke RM, Sheehan JP. Radiosurgery for cerebral arteriovenous malformations in elderly patients: effect of advanced age on outcomes after intervention. World Neurosurg. 2015; 9. 84(3):795–804. PMID: 25997797.
Article30. Ding D, Xu Z, Yen CP, Starke RM, Sheehan JP. Radiosurgery for unruptured cerebral arteriovenous malformations in pediatric patients. Acta Neurochir (Wien). 2015; 2. 157(2):281–291. PMID: 25514868.
Article31. Ding D, Yen CP, Starke RM, Xu Z, Sheehan JP. Effect of prior hemorrhage on intracranial arteriovenous malformation radiosurgery outcomes. Cerebrovasc Dis. 2015; 39(1):53–62. PMID: 25547253.
Article32. Ding D, Yen CP, Starke RM, Xu Z, Sheehan JP. Radiosurgery for ruptured intracranial arteriovenous malformations. J Neurosurg. 2014; 8. 121(2):470–481. PMID: 24655098.
Article33. Ding D, Yen CP, Starke RM, Xu Z, Sun X, Sheehan JP. Outcomes following single-session radiosurgery for high-grade intracranial arteriovenous malformations. Br J Neurosurg. 2014; 10. 28(5):666–674. PMID: 24372542.
Article34. Ding D, Yen CP, Starke RM, Xu Z, Sun X, Sheehan JP. Radiosurgery for Spetzler-Martin Grade III arteriovenous malformations. J Neurosurg. 2014; 4. 120(4):959–969. PMID: 24460487.
Article35. Ding D, Yen CP, Xu Z, Starke RM, Sheehan JP. Radiosurgery for low-grade intracranial arteriovenous malformations. J Neurosurg. 2014; 8. 121(2):457–467. PMID: 24605839.
Article36. Ding D, Yen CP, Xu Z, Starke RM, Sheehan JP. Radiosurgery for patients with unruptured intracranial arteriovenous malformations. J Neurosurg. 2013; 5. 118(5):958–966. PMID: 23530863.
Article37. Ding D, Yen CP, Xu Z, Starke RM, Sheehan JP. Radiosurgery for primary motor and sensory cortex arteriovenous malformations: outcomes and the effect of eloquent location. Neurosurgery. 2013; 11. 73(5):816–824. PMID: 23867301.38. Garcia RM, Ivan ME, Lawton MT. Brainstem cavernous malformations: surgical results in 104 patients and a proposed grading system to predict neurological outcomes. Neurosurgery. 2015; 3. 76(3):265–277. discussion 277-8. PMID: 25599205.39. Garrett M, Spetzler RF. Surgical treatment of brainstem cavernous malformations. Surg Neurol. 2009; 12. 72(Suppl 2):S3–S9. discussion S9-10. PMID: 19665186.
Article40. Giliberto G, Lanzino DJ, Diehn FE, Factor D, Flemming KD, Lanzino G. Brainstem cavernous malformations: anatomical, clinical, and surgical considerations. Neurosurg Focus. 2010; 9. 29(3):E9.
Article41. Gross BA, Batjer HH, Awad IA, Bendok BR. Brainstem cavernous malformations. Neurosurgery. 2009; 5. 64(5):E805–E818. discussion E818. PMID: 19404127.
Article42. Gross BA, Batjer HH, Awad IA, Bendok BR. Cavernous malformations of the basal ganglia and thalamus. Neurosurgery. 2009; 7. 65(1):7–18. discussion 18-9. PMID: 19574821.
Article43. Hong CS, Peterson EC, Ding D, Sur S, Hasan D, Dumont AS, et al. Intervention for a randomized trial of unruptured brain arteriovenous malformations (ARUBA) - Eligible patients: an evidence-based review. Clin Neurol Neurosurg. 2016; 11. 150:133–138. PMID: 27656780.
Article44. Ilyas A, Chen CJ, Ding D, Taylor DG, Moosa S, Lee CC, et al. Volume-staged versus dose-staged stereotactic radiosurgery outcomes for large brain arteriovenous malformations: a systematic review. J Neurosurg. 2017; 1. 1–11. [Epub ahead of print].
Article45. Kawashima M, Matsushima T, Nakahara Y, Takase Y, Masuoka J, Ohata K. Trans-cerebellomedullary fissure approach with special reference to lateral route. Neurosurg Rev. 2009; 10. 32(4):457–464. PMID: 19609581.
Article46. Leslie K, Hui R, Kaye AH. Venous air embolism and the sitting position: a case series. J Clin Neurosci. 2006; 5. 13(4):419–422. PMID: 16678719.
Article47. Li D, Zhang J, Hao S, Tang J, Xiao X, Wu Z, et al. Surgical treatment and long-term outcomes of thalamic cavernous malformations. World Neurosurg. 2013; May-Jun. 79(5-6):704–713. PMID: 22381871.
Article48. Matsushima T, Abe H, Kawashima M, Inoue T. Exposure of the wide interior of the fourth ventricle without splitting the vermis: importance of cutting procedures for the tela choroidea. Neurosurg Rev. 2012; 10. 35(4):563–571. discussion 571-2. PMID: 22527626.
Article49. Moosa S, Chen CJ, Ding D, Lee CC, Chivukula S, Starke RM, et al. Volume-staged versus dose-staged radiosurgery outcomes for large intracranial arteriovenous malformations. Neurosurg Focus. 2014; 9. 37(3):E18.
Article50. Mouchtouris N, Jabbour PM, Starke RM, Hasan DM, Zanaty M, Theofanis T, et al. Biology of cerebral arteriovenous malformations with a focus on inflammation. J Cereb Blood Flow Metab. 2015; 2. 35(2):167–175. PMID: 25407267.
Article51. Moultrie F, Horne MA, Josephson CB, Hall JM, Counsell CE, Bhattacharya JJ, et al. Outcome after surgical or conservative management of cerebral cavernous malformations. Neurology. 2014; 8. 83(7):582–589. PMID: 24994841.
Article52. Oermann EK, Ding D, Yen CP, Starke RM, Bederson JB, Kondziolka D, et al. Effect of prior embolization on cerebral arteriovenous malformation radiosurgery outcomes: a case-control study. Neurosurgery. 2015; 9. 77(3):406–417. discussion 417. PMID: 25875580.53. Oermann EK, Rubinsteyn A, Ding D, Mascitelli J, Starke RM, Bederson JB, et al. Using a machine learning approach to predict outcomes after radiosurgery for cerebral arteriovenous malformations. Sci Rep. 2016; 2. 09. 6:21161. PMID: 26856372.
Article54. Ohue S, Fukushima T, Friedman AH, Kumon Y, Ohnishi T. Retrosigmoid suprafloccular transhorizontal fissure approach for resection of brainstem cavernous malformation. Neurosurgery. 2010; 6. 66(6 Suppl Operative):306–312. discussion 312-3. PMID: 20489521.
Article55. Pandey P, Westbroek EM, Gooderham PA, Steinberg GK. Cavernous malformation of brainstem, thalamus, and basal ganglia: a series of 176 patients. Neurosurgery. 2013; 4. 72(4):573–589. discussion 588-9. PMID: 23262564.56. Patibandla MR, Ding D, Xu Z, Sheehan JP. Stereotactic radiosurgery for pediatric high-grade brain arteriovenous malformations: our experience and review of literature. World Neurosurg. 2017; 3. 23. [Epub ahead of print].
Article57. Porter PJ, Willinsky RA, Harper W, Wallace MC. Cerebral cavernous malformations: natural history and prognosis after clinical deterioration with or without hemorrhage. J Neurosurg. 1997; 8. 87(2):190–197. PMID: 9254081.
Article58. Porter RW, Detwiler PW, Spetzler RF, Lawton MT, Baskin JJ, Derksen PT, et al. Cavernous malformations of the brainstem: experience with 100 patients. J Neurosurg. 1999; 1. 90(1):50–58. PMID: 10413155.
Article59. Przybylowski CJ, Ding D, Starke RM, Yen CP, Quigg M, Dodson B, et al. Seizure and anticonvulsant outcomes following stereotactic radiosurgery for intracranial arteriovenous malformations. J Neurosurg. 2015; 6. 122(6):1299–1305. PMID: 25614948.
Article60. Recalde RJ, Figueiredo EG, de Oliveira E. Microsurgical anatomy of the safe entry zones on the anterolateral brainstem related to surgical approaches to cavernous malformations. Neurosurgery. 2008; 3. 62(3 Suppl 1):9–15. discussion 15-7. PMID: 18424962.
Article61. Samii M, Eghbal R, Carvalho GA, Matthies C. Surgical management of brainstem cavernomas. J Neurosurg. 2001; 11. 95(5):825–832. PMID: 11702873.
Article62. Sinson G, Zager EL, Grossman RI, Gennarelli TA, Flamm ES. Cavernous malformations of the third ventricle. Neurosurgery. 1995; 7. 37(1):37–42. PMID: 8587688.
Article63. Starke RM, Ding D, Kano H, Mathieu D, Huang PP, Feliciano C, et al. International multicenter cohort study of pediatric brain arteriovenous malformations. Part 2: Outcomes after stereotactic radiosurgery. J Neurosurg Pediatr. 2017; 2. 19(2):136–148. PMID: 27911249.
Article64. Starke RM, Kano H, Ding D, Lee JY, Mathieu D, Whitesell J, et al. Stereotactic radiosurgery for cerebral arteriovenous malformations: evaluation of long-term outcomes in a multicenter cohort. J Neurosurg. 2017; 1. 126(1):36–44. PMID: 26943847.
Article65. Starke RM, Sheehan JP, Ding D, Liu KC, Kondziolka D, Crowley RW, et al. Conservative management or intervention for unruptured brain arteriovenous malformations. World Neurosurg. 2014; 11. 82(5):e668–e669. PMID: 25053376.
Article66. Starke RM, Yen CP, Chen CJ, Ding D, Mohila CA, Jensen ME, et al. An updated assessment of the risk of radiation-induced neoplasia after radiosurgery of arteriovenous malformations. World Neurosurg. 2014; Sep-Oct. 82(3-4):395–401. PMID: 23403354.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Abnormal Eye Movements in Brainstem Cavernous Malformations
- Cavernous Hemangioma on the Frontal Lobe
- Contralateral Interhemispheric Transcallosal Approach for Thalamic Cystic Cavernous Malformation
- Cavernous Hemangioma of the Cauda Equina
- Clinical Analysis of Microsurgery for Brainstem Cavernous Malformations: Surgical Indications, Optimal Approaches, and Clinical Outcomes