Korean Circ J.
2017 Mar;47(2):201-208. 10.4070/kcj.2016.0194.
Clinical Outcomes after Anatomic Repair Including Hemi-Mustard Operation in Patients with Congenitally Corrected Transposition of the Great Arteries
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. tgjunsmc@gmail.com
- 2Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2377460
- DOI: http://doi.org/10.4070/kcj.2016.0194
Abstract
- BACKGROUND AND OBJECTIVES
The aims of this study were to determine the early and late outcomes of anatomic repair of congenitally corrected transposition of the great arteries (ccTGA) and to evaluate effectiveness of the hemi-Mustard procedure.
SUBJECTS AND METHODS
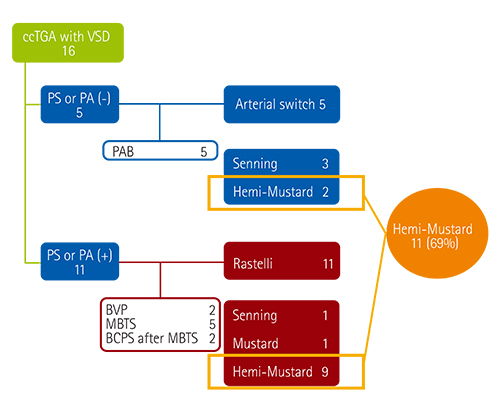
We conducted a retrospective, single-center study of patients who underwent anatomic repair for ccTGA between July 1996 and December 2013. Sixteen patients were included in the study. The median age at the time of the operation was 3.5 years (range: 0.5-29.7), and the median body weight was 13.3 kg (range: 5.8-54). The median follow-up duration was 7.7 years (range: 0.2-17.4).
RESULTS
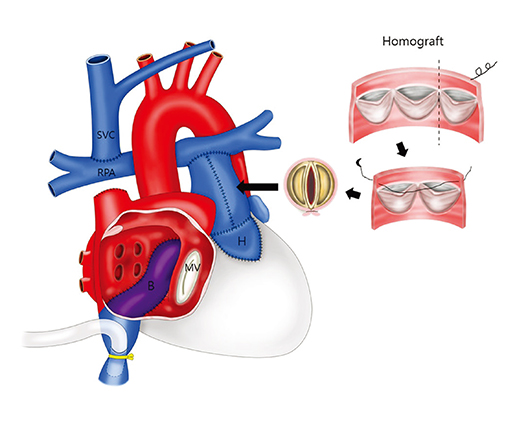
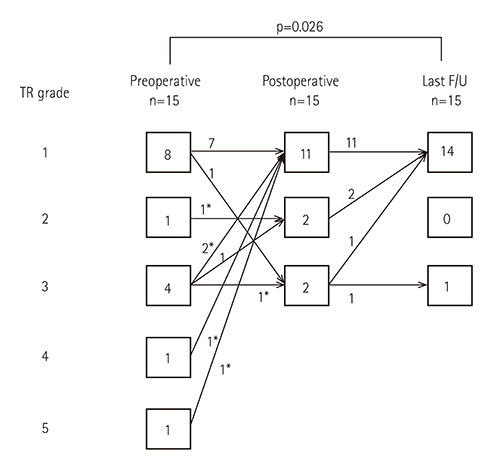
Atrial switch was achieved using the Mustard procedure in 12 patients (hemi-Mustard procedure in 11) or the Senning procedure in four patients. The ventriculoarterial procedure was performed using the Rastelli procedure in 11 patients and arterial switch in five patients. Six patients underwent tricuspid valvuloplasty. The survival rate was 93.8±6.1%. The rate of freedom from reoperation at 5 years was 92.3±7.4% in the Rastelli group. All patients except one were New York Heart Association class I. All patients except one had mild tricuspid regurgitation.
CONCLUSION
Anatomic repair can be performed with a low risk of in-hospital mortality. The hemi-Mustard strategy for selected patients is one solution for reducing early mortality and morbidity, and long-term complications such as venous pathway stenosis or sinus node dysfunction.
MeSH Terms
Figure
Reference
-
1. Wallis GA, Debich-Spicer D, Anderson RH. Congenitally corrected transposition. Orphanet J Rare Dis. 2011; 6:22.2. Yeh T Jr, Connelly MS, Coles JG, et al. Atrioventricular discordance: results of repair in 127 patients. J Thorac Cardiovasc Surg. 1999; 117:1190–1203.3. Biliciler-Denktas G, Feldt RH, Connolly HM, Weaver AL, Puga FJ, Danielson GK. Early and late results of operations for defects associated with corrected transposition and other anomalies with atrioventricular discordance in a pediatric population. J Thorac Cardiovasc Surg. 2001; 122:234–241.4. Hraska V, Duncan BW, Mayer JE Jr, Freed M, del Nido PJ, Jonas RA. Long-term outcome of surgically treated patients with corrected transposition of the great arteries. J Thorac Cardiovasc Surg. 2005; 129:182–191.5. Sharma R, Talwar S, Marwah A, et al. Anatomic repair for congenitally corrected transposition of the great arteries. J Thorac Cardiovasc Surg. 2009; 137:404–412.e4.6. Murtuza B, Barron DJ, Stumper O, et al. Anatomic repair for congenitally corrected transposition of the great arteries: a single-institution 19-year experience. J Thorac Cardiovasc Surg. 2011; 142:1348–1357.e1.7. Myers PO, Bautista-Hernandez V, Baird CW, Emani SM, Marx GR, del Nido PJ. Tricuspid regurgitation or Ebsteinoid dysplasia of the tricuspid valve in congenitally corrected transposition: is valvuloplasty necessary at anatomic repair? J Thorac Cardiovasc Surg. 2014; 147:576–580.8. Hiramatsu T, Matsumura G, Konuma T, Yamazaki K, Kurosawa H, Imai Y. Long-term prognosis of double-switch operation for congenitally corrected transposition of the great arteries. Eur J Cardiothorac Surg. 2012; 42:1004–1008.9. Malhotra SP, Reddy VM, Qiu M, et al. The hemi-Mustard/bidirectional Glenn atrial switch procedure in the double-switch operation for congenitally corrected transposition of the great arteries: rationale and midterm results. J Thorac Cardiovasc Surg. 2011; 141:162–170.10. Sojak V, Kuipers I, Koolbergen D, et al. Mid-term results of bidirectional cavopulmonary anastomosis and hemi-Mustard procedure in anatomical correction of congenitally corrected transposition of the great arteries. Eur J Cardiothorac Surg. 2012; 42:680–684.11. Yang JH, Jun TG, Sung K, Kim WS, Lee YT, Park PW. Midterm results of size-reduced cryopreserved homografts for right ventricular outflow tract reconstruction. Ann Thorac Surg. 2010; 89:1821–1826.12. Khairy P, Landzberg MJ, Lambert J, O'Donnell CP. Long-term outcomes after the atrial switch for surgical correction of transposition: a meta-analysis comparing the Mustard and Senning procedures. Cardiol Young. 2004; 14:284–292.13. Hoashi T, Kagisaki K, Miyazaki A, et al. Anatomic repair for corrected transposition with left ventricular outflow tract obstruction. Ann Thorac Surg. 2013; 96:611–620.14. Barron DJ, Jones TJ, Brawn WJ. The Senning procedure as part of the double-switch operations for congenitally corrected transposition of the great arteries. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2011; 14:109–115.15. Horer J, Schreiber C, Krane S, et al. Outcome after surgical repair/palliation of congenitally corrected transposition of the great arteries. Thorac Cardiovasc Surg. 2008; 56:391–397.16. DiBardino DJ, Heinle JS, Fraser CD Jr. The hemi-Mustard, bi-directional Glenn, and Rastelli operations used for correction of congenitally corrected transposition, achieving a “ventricle and a half“ repair. Cardiol Young. 2004; 14:330–332.17. Raisky O, Gaudin R. Anatomic repair for congenitally corrected transposition of the great arteries: easier is better? Eur J Cardiothorac Surg. 2012; 42:685–686.18. Gaies MG, Goldberg CS, Ohye RG, Devaney EJ, Hirsch JC, Bove EL. Early and intermediate outcome after anatomic repair of congenitally corrected transposition of the great arteries. Ann Thorac Surg. 2009; 88:1952–1960.19. Van Arsdell GS, Williams WG, Maser CM, et al. Superior vena cava to pulmonary artery anastomosis: an adjunct to biventricular repair. J Thorac Cardiovasc Surg. 1996; 112:1143–1148. discussion 1148-9.20. Reddy VM, McElhinney DB, Silverman NH, Marianeschi SM, Hanley FL. Partial biventricular repair for complex congenital heart defects: an intermediate option for complicated anatomy or functionally borderline right complex heart. J Thorac Cardiovasc Surg. 1998; 116:21–27.21. Hosseinpour AR, McCarthy KP, Griselli M, Sethia B, Ho SY. Congenitally corrected transposition: size of the pulmonary trunk and septal malalignment. Ann Thorac Surg. 2004; 77:2163–2166.22. Yagihara T, Kishimoto H, Isobe F, et al. Double switch operation in cardiac anomalies with atrioventricular and ventriculoarterial discordance. J Thorac Cardiovasc Surg. 1994; 107:351–358.23. Winlaw DS, McGuirk SP, Balmer C, et al. Intention-to-treat analysis of pulmonary artery banding in conditions with a morphological right ventricle in the systemic circulation with a view to anatomic biventricular repair. Circulation. 2005; 111:405–411.24. Quinn DW, McGuirk SP, Metha C, et al. The morphologic left ventricle that requires training by means of pulmonary artery banding before the double-switch procedure for congenitally corrected transposition of the great arteries is at risk of late dysfunction. J Thorac Cardiovasc Surg. 2008; 135:1137–1144. 1144.e1–1144.e2.25. Myers PO, del Nido PJ, Geva T, et al. Impact of age and duration of banding on left ventricular preparation before anatomic repair for congenitally corrected transposition of the great arteries. Ann Thorac Surg. 2013; 96:603–610.26. Shin'oka T, Kurosawa H, Imai Y, et al. Outcomes of definitive surgical repair for congenitally corrected transposition of the great arteries or double outlet right ventricle with discordant atrioventricular connections: risk analyses in 189 patients. J Thorac Cardiovasc Surg. 2007; 133:1318–1328. 1328.e1–1328.e4.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anatomic Repair Including Hemi-Mustard in Congenitally Corrected Transposition of the Great Arteries: What We know and Still Need to Know
- An Adult Case of Congenitally Corrected Transposition of the Great Arteries Associated with Paroxysmal Atrial Fibrillation and Heart Failure
- Right Ventricular Inflow Obstruction Caused by Supratricuspid Ring after the Conventional Biventricular Repair of Congenitally Corrected Transposition of Great Arteries: A case report
- Transposition of the Great Arteries: Historical Background
- Anatomical Repair of Congenitally Physiologically Corrected Transposition with Dextrocardia, Situs Inversus and the Interruption of Right Pulmonary Artery