Diabetes Metab J.
2017 Apr;41(2):99-112. 10.4093/dmj.2017.41.2.99.
Diabetes Camp as Continuing Education for Diabetes Self-Management in Middle-Aged and Elderly People with Type 2 Diabetes Mellitus
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. sangman.jin@samsung.com
- 2Diabetes Education Unit, Diabetes Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jsmercy@naver.com
- KMID: 2376772
- DOI: http://doi.org/10.4093/dmj.2017.41.2.99
Abstract
- BACKGROUND
Despite the established benefits of diabetes camps for the continuing education of children with type 1 diabetes mellitus, little is known about the long-term metabolic benefits of diabetes camps for middle-aged and elderly people with type 2 diabetes mellitus (T2DM), especially in terms of glycosylated hemoglobin (HbA1c) variability.
METHODS
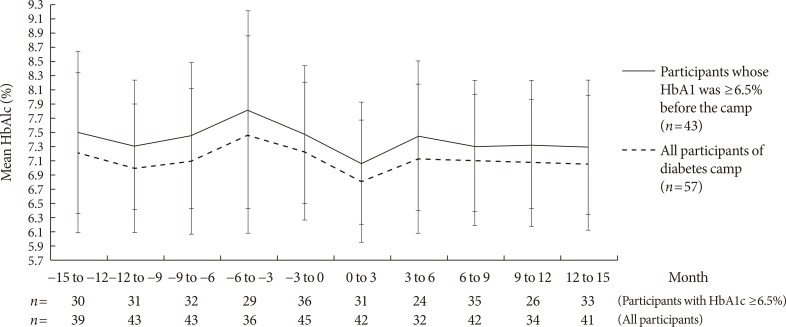
The 1-year mean and variability of HbA1c before and after the diabetes camp was compared between the participants of the diabetes camp (n=57; median age 65 years [range, 50 to 86 years]; median diabetes duration 14 years [range, 1 to 48 years]). Additional case-control analysis compared the metabolic outcomes of the participants of the diabetes camp and their propensity score-matched controls who underwent conventional diabetes education (n=93).
RESULTS
The levels of HbA1c during the first year after the diabetes camp were comparable to those of the matched controls (P=0.341). In an analysis of all participants of the diabetes camp, the 1-year mean±standard deviation (SD) of HbA1c decreased (P=0.010 and P=0.041) after the diabetes camp, whereas the adjusted SD and coefficient of variance (CV) of HbA1c did not decrease. The adjusted SD and CV significantly decreased after the diabetes camp in participants whose 1-year mean HbA1c was ≥6.5% before the diabetes camp (n=40) and those with a duration of diabetes less than 15 years (n=32).
CONCLUSION
The 1-year mean and SD of HbA1c decreased after the diabetes camp, with significant reduction in the adjusted SD and CV in those with higher baseline HbA1c and a shorter duration of diabetes.
Keyword
MeSH Terms
Figure
Reference
-
1. Gagliardino JJ, Aschner P, Baik SH, Chan J, Chantelot JM, Ilkova H, Ramachandran A. IDMPS investigators. Patients' education, and its impact on care outcomes, resource consumption and working conditions: data from the International Diabetes Management Practices Study (IDMPS). Diabetes Metab. 2012; 38:128–134. PMID: 22019715.
Article2. Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002; 25:1159–1171. PMID: 12087014.3. Kim MY, Suh S, Jin SM, Kim SW, Bae JC, Hur KY, Kim SH, Rha MY, Cho YY, Lee MS, Lee MK, Kim KW, Kim JH. Education as prescription for patients with type 2 diabetes mellitus: compliance and efficacy in clinical practice. Diabetes Metab J. 2012; 36:452–459. PMID: 23275939.
Article4. Choi MJ, Yoo SH, Kim KR, Bae YM, Ahn SH, Kim SS, Min SA, Choi JS, Lee SE, Moon YJ, Rhee EJ, Park CY, Lee WY, Oh KW, Park SW, Kim SW. Effect on glycemic, blood pressure, and lipid control according to education types. Diabetes Metab J. 2011; 35:580–586. PMID: 22247900.
Article5. Hermanns N, Schmitt A, Gahr A, Herder C, Nowotny B, Roden M, Ohmann C, Kruse J, Haak T, Kulzer B. The effect of a Diabetes-Specific Cognitive Behavioral Treatment Program (DIAMOS) for patients with diabetes and subclinical depression: results of a randomized controlled trial. Diabetes Care. 2015; 38:551–560. PMID: 25605812.
Article6. Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Hess Fischl A, Maryniuk MD, Siminerio L, Vivian E. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Care. 2015; 38:1372–1382. PMID: 26048904.
Article7. Carlson KT, Carlson GW Jr, Tolbert L, Demma LJ. Blood glucose levels in children with type 1 diabetes attending a residential diabetes camp: a 2-year review. Diabet Med. 2013; 30:e123–e126. PMID: 23157253.8. Dehayem MY, Takogue R, Choukem SP, Donfack OT, Katte JC, Sap S, Sobngwi E, Mbanya JC. Impact of a pioneer diabetes camp experience on glycemic control among children and adolescents living with type 1 diabetes in sub-Saharan Africa. BMC Endocr Disord. 2016; 16:5. PMID: 26791079.
Article9. American Diabetes Association. Diabetes management at camps for children with diabetes. Diabetes Care. 2012; 35(Suppl 1):S72–S75. PMID: 22187473.10. Stahl D, Sum CF, Lum SS, Liow PH, Chan YH, Verma S, Chua HC, Chong SA. Screening for depressive symptoms: validation of the center for epidemiologic studies depression scale (CES-D) in a multiethnic group of patients with diabetes in Singapore. Diabetes Care. 2008; 31:1118–1119. PMID: 18337303.11. Zhang Y, Ting RZ, Lam MH, Lam SP, Yeung RO, Nan H, Ozaki R, Luk AO, Kong AP, Wing YK, Sartorius N, Chan JC. Measuring depression with CES-D in Chinese patients with type 2 diabetes: the validity and its comparison to PHQ-9. BMC Psychiatry. 2015; 15:198. PMID: 26281832.
Article12. Hajos TR, Pouwer F, Skovlund SE, Den Oudsten BL, Geelhoed-Duijvestijn PH, Tack CJ, Snoek FJ. Psychometric and screening properties of the WHO-5 well-being index in adult outpatients with type 1 or type 2 diabetes mellitus. Diabet Med. 2013; 30:e63–e69. PMID: 23072401.13. Newnham EA, Hooke GR, Page AC. Monitoring treatment response and outcomes using the World Health Organization's Wellbeing Index in psychiatric care. J Affect Disord. 2010; 122:133–138. PMID: 19592116.
Article14. Kim TK, Kang YE, Kim JM, Hong WJ, Kim KS, Kim HJ, Kim YK, Ku BJ. Effects of diabetic camp in type 2 diabetic patients. Korean J Med. 2012; 83:210–215.
Article15. American Diabetes Association. 10. Older adults. Diabetes Care. 2016; 39(Suppl 1):S81–S85. PMID: 26696686.16. Bultas MW, Schmuke AD, Moran V, Taylor J. Psychosocial outcomes of participating in pediatric diabetes camp. Public Health Nurs. 2016; 33:295–302. PMID: 26223690.
Article17. Safren SA, Gonzalez JS, Wexler DJ, Psaros C, Delahanty LM, Blashill AJ, Margolina AI, Cagliero E. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in patients with uncontrolled type 2 diabetes. Diabetes Care. 2014; 37:625–633. PMID: 24170758.
Article18. Bultas MW, Budhathoki C, Balakas K. Evaluation of child and parent outcomes after a pediatric cardiac camp experience. J Spec Pediatr Nurs. 2013; 18:320–328. PMID: 24094127.
Article19. Baumeister H, Hutter N, Bengel J. Psychological and pharmacological interventions for depression in patients with diabetes mellitus and depression. Cochrane Database Syst Rev. 2012; 12:CD008381. PMID: 23235661.
Article20. Penno G, Solini A, Zoppini G, Orsi E, Fondelli C, Zerbini G, Morano S, Cavalot F, Lamacchia O, Trevisan R, Vedovato M, Pugliese G. Renal Insufficiency and Cardiovascular Events (RIACE) Study Group. Hemoglobin A1c variability as an independent correlate of cardiovascular disease in patients with type 2 diabetes: a cross-sectional analysis of the renal insufficiency and cardiovascular events (RIACE) Italian multicenter study. Cardiovasc Diabetol. 2013; 12:98. PMID: 23829205.
Article21. Penno G, Solini A, Bonora E, Fondelli C, Orsi E, Zerbini G, Morano S, Cavalot F, Lamacchia O, Laviola L, Nicolucci A, Pugliese G. Renal Insufficiency And Cardiovascular Events Study Group. HbA1c variability as an independent correlate of nephropathy, but not retinopathy, in patients with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicenter study. Diabetes Care. 2013; 36:2301–2310. PMID: 23491522.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Developing Strategies for Diabetes Education Program
- Management of Type 1 Diabetes Mellitus in Adults
- Discharge Planning for Elderly Diabetic Patients
- Effect of Self-care Education at a Diabetes Camp on Diabetes Management Behaviors, Knowledge and Self-efficacy in Children with Type 1 Diabetes
- Management of Type 2 Diabetes Mellitus in Older Adults