Nat Prod Sci.
2017 Mar;23(1):40-45. 10.20307/nps.2017.23.1.40.
Protection Against Electroshock- and Pentylenetetrazol-induced Seizures by the Water Extract of Rehmannia glutinous can be Mediated through GABA Receptor-chloride Channel Complexes
- Affiliations
-
- 1Uimyung Research Institute for Neuroscience, Department of Pharmacy, Sahmyook University, Seoul 01795, Republic of Korea. cheongjh@syu.ac.kr
- 2Department of Pharmacology, College of Pharmacy, Duksung Women's University, Seoul 01369, Republic of Korea.
- 3Department of Oriental Pharmaceutical Science, College of Pharmacy, Kyung Hee University, Seoul 02447, Republic of Korea.
- KMID: 2376498
- DOI: http://doi.org/10.20307/nps.2017.23.1.40
Abstract
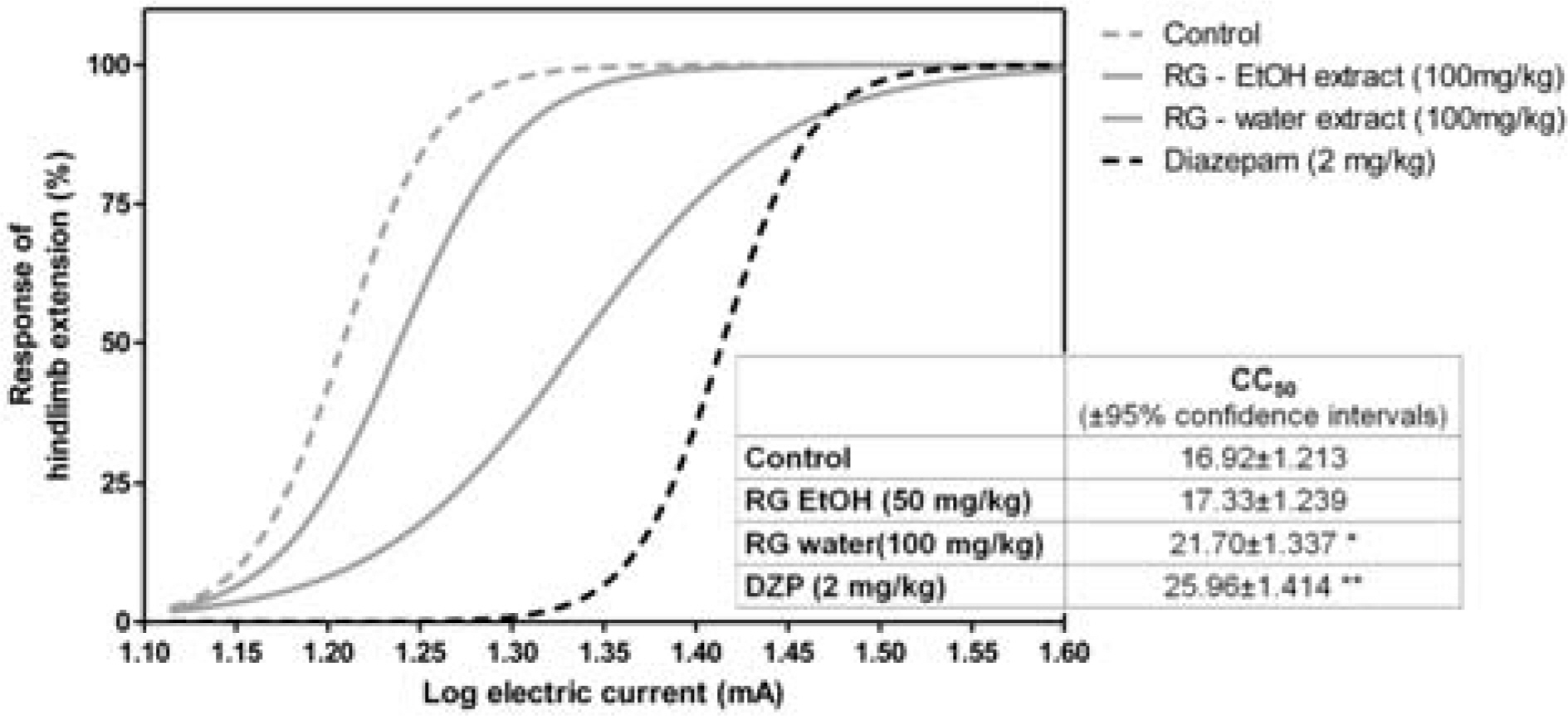
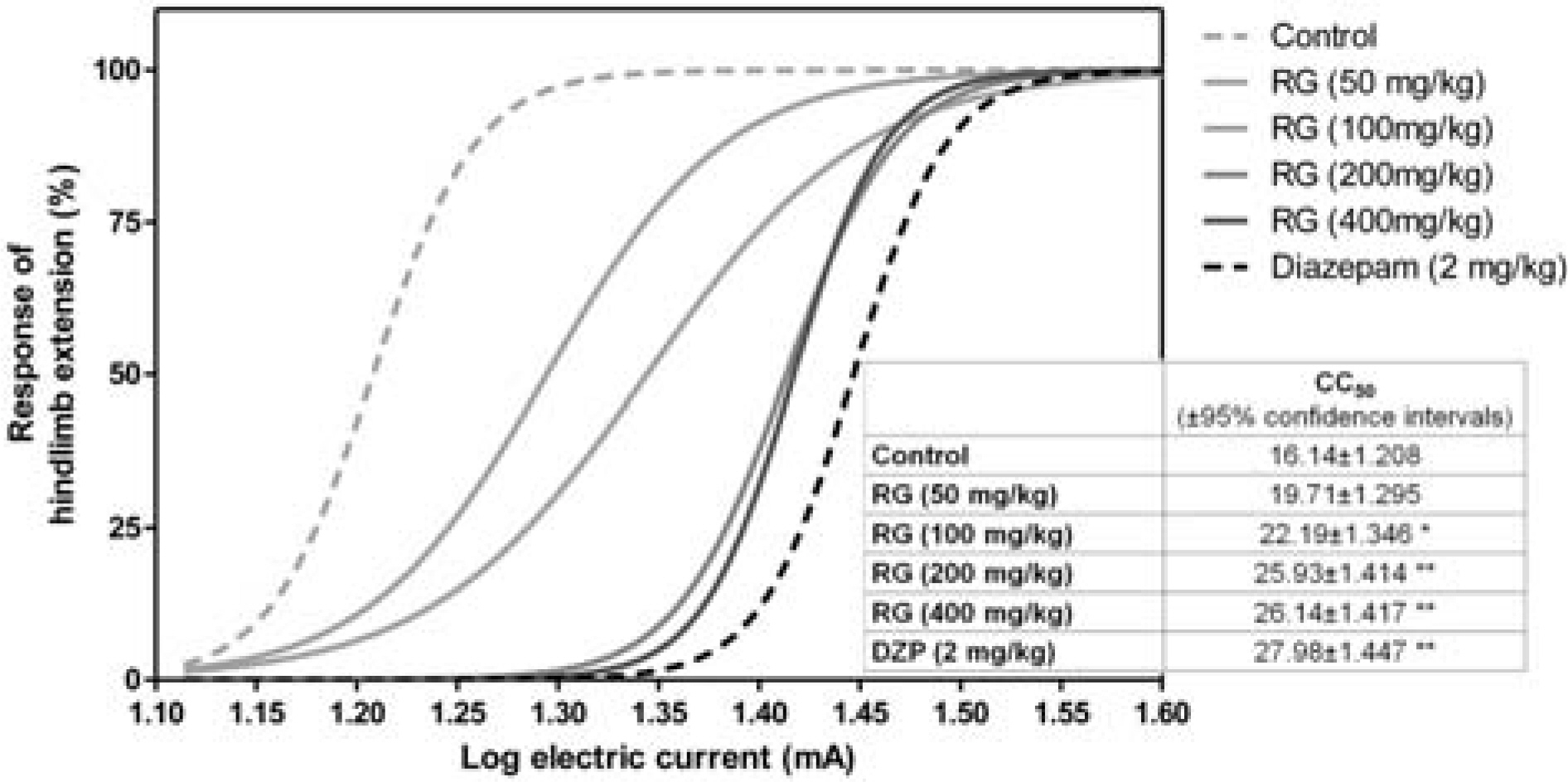
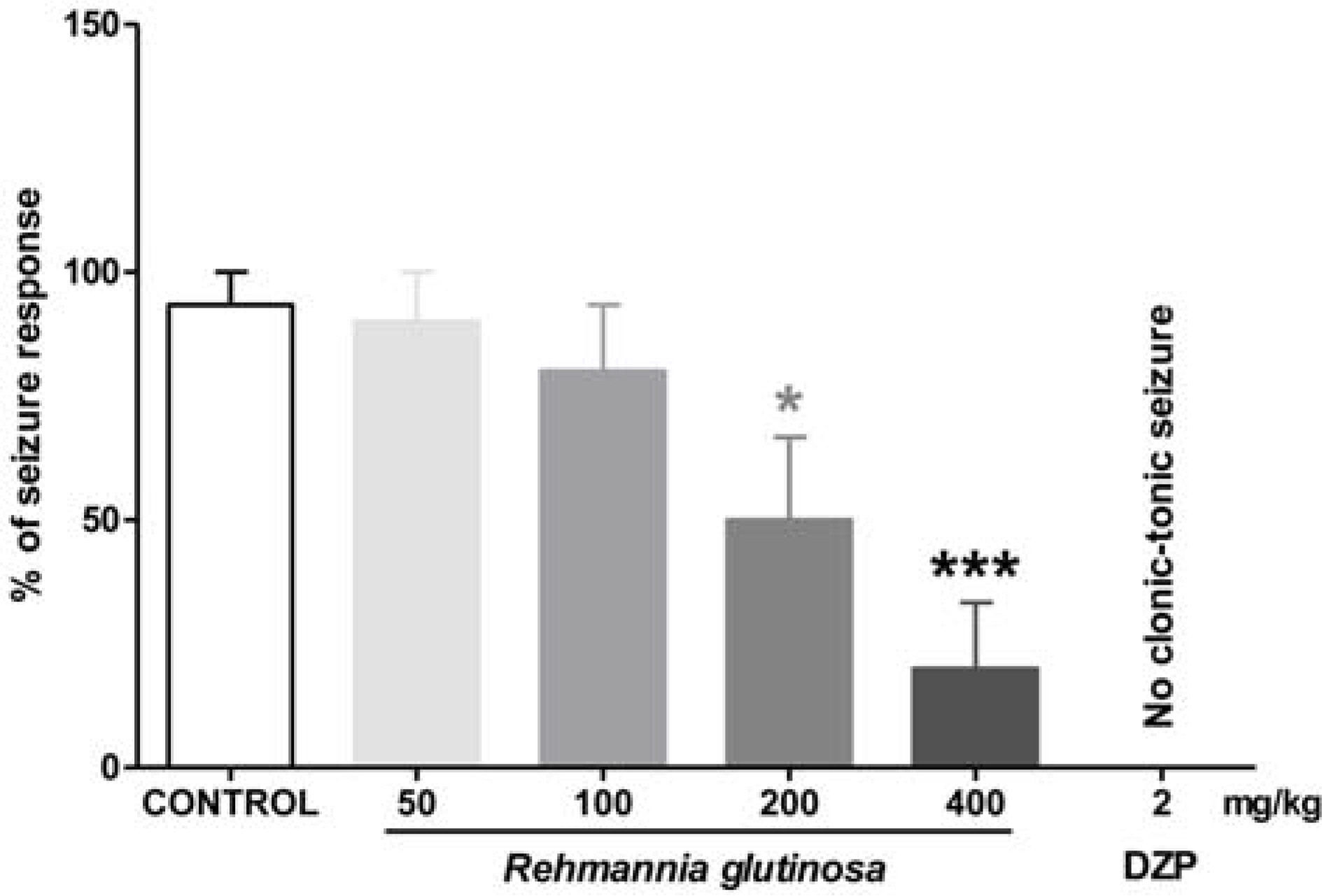
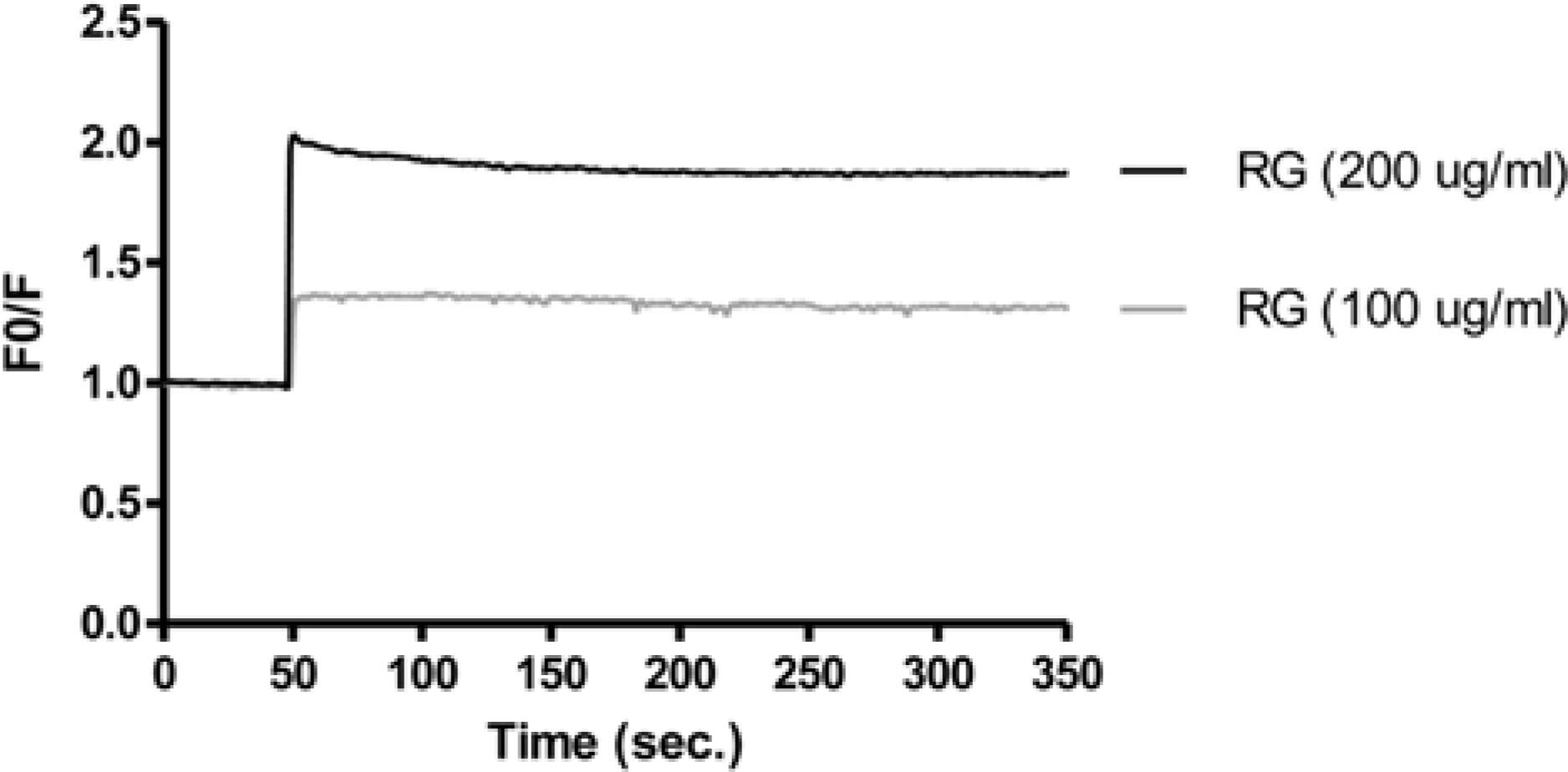
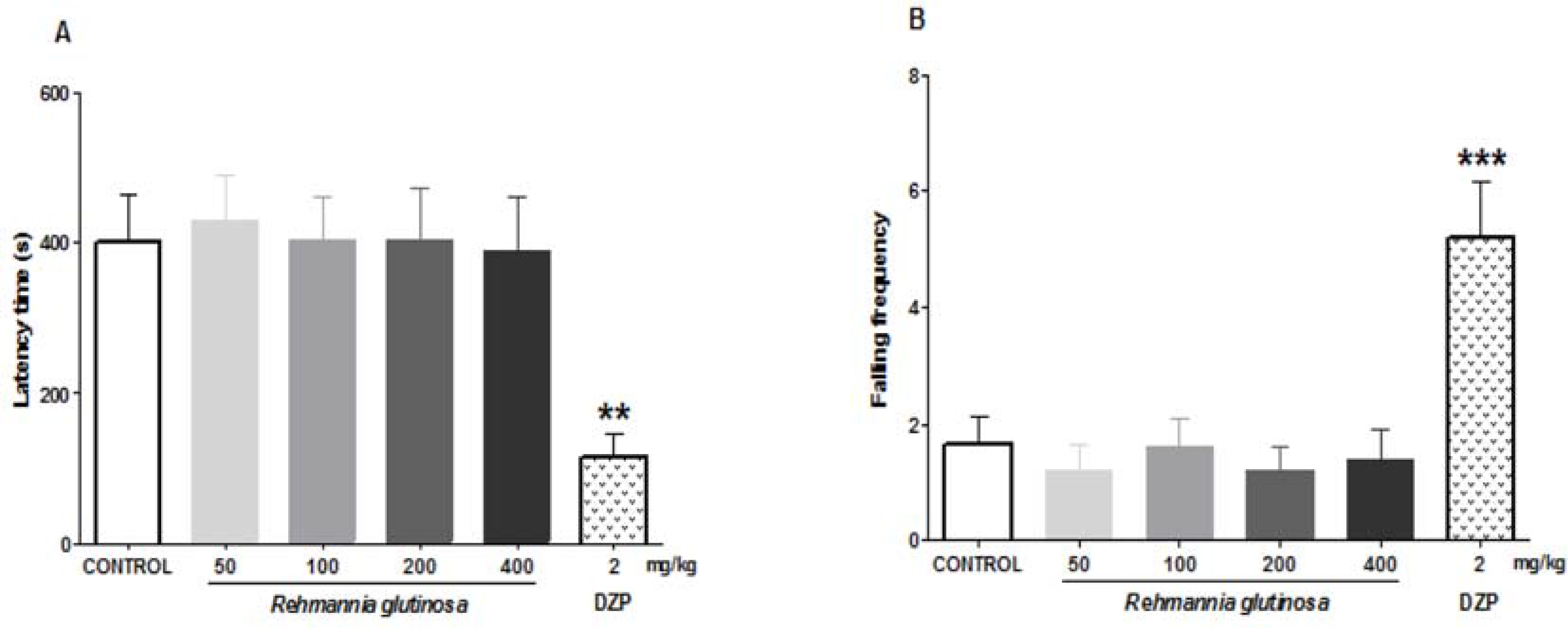
- Epilepsy is a brain disorder that affects millions of people worldwide. It is characterized by recurrent and unpredictable seizures that are usually controlled with antiepileptic/anticonvulsive drugs. However, most antiepileptic drugs produce various side effects such as tolerance and sedation. Thus, there is a growing interest for alternative anticonvulsive drugs, preferably from natural or herbal sources. In this study, we evaluated the anticonvulsive effects of Rehmannia glutinosa (RG). The anticonvulsive effect of RG extract was evaluated using electroshock- and chemical-induced seizure tests in mice. To identify its probable mechanism of action, the effects of RG extract on Cl− influx was measured in vitro. We found that RG extract has anticonvulsive effects against electroshock-induced seizures, as indicated by an increased seizure threshold in mice. The RG extract also decreased the percentage of seizure responses induced by the GABAergic antagonist, pentylenetetrazole. These results suggest that the anticonvulsive effects of RG extract are mediated through a GABAergic mechanism. In support of this mechanism, our in vitro test showed that RG extract increases intracellular Cl− influx. Furthermore, RG extract did not show sedative and/or muscle relaxant effects in the open-field and rota-rod tests. Altogether, these results confirm that RG extract could be a herbal anticonvulsant and a potential alternative for clinical use.
Keyword
MeSH Terms
Figure
Reference
-
References
(1). Fisher R.S.., van Emde Boas W.., Blume W.., Elger C.., Genton P.., Lee P.., Engel Jr J.Epilepsia. 2005. 46:470–472.(2). Blume W.T.., Lüders H.O.., Mizrahi E.., Tassinari C.., van Emde Boas W.., Engel Jr J.Epilepsia. 2001. 42:1212–1218.(3). Shorvon S.Handbook of epilepsy treatment (3rd ed); John Wiley & Sons: United Kingdom,. 2010.(4). Schmidt D.., Schachter S.C.BMJ. 2014. 348:g254.(5). Swann A.C. J.Clin. Psychiatry. 2001. 62:16–21.(6). Megiddo I.., Colson A.., Chisholm D.., Dua T.., Nandi A.., Laxminarayan R.Epilepsia. 2016. 57:464–474.(7). Samuels N.., Finkelstein Y.., Singer S.R.., Oberbaum M.Epilepsia. 2008. 49:373–380.(8). QuintansJúnior L.J.., Almeida J.R.., Lima J.T.., Nunes X.P.., Siqueira J.S.., Oliveira L.E.G.., Almeida R.N.., Athayde-Filho P.F.., Barbosa-Filho J.M.Rev. Bras. Farmacogn. 2008. 18:798–819.(9). Woo T.S.., Yoon S.Y.., dela Peña I.C.., Choi J.Y.., Lee H.L.., Choi Y.J.., Lee Y.S.., Ryu J.H.., Choi J.S.., Cheong J.H.Biomol. Ther. 2011. 19:342–347.(10). Hijikata Y.., Yasuhara A.., Yoshida Y.., Sento S. J.Altern. Complement. Med. 2006. 12:673–677.(11). Kwon B.H.., Gu B.S. J.Oriental Neuropsychiatry,. 1999. 10:1–27.(12). Jiao Z.., Cheng Y.., Wang H.., Lei C.., Wang G.G.., Han L.Appl. Plant Sci. 2015. 3:1500054.(13). Baek G.H.., Jang Y.S.., Jeong S.I.., Cha J.., Joo M.., Shin S.W.., Ha K.T.., Jeong H. S.Inflammation. 2012. 35:1232–1241.(14). Dingding C.., Dai Dezai Z. T.Pharmacology and Clinics of Chinese Materia Medica. 1996. 5:010.(15). Huang Y.., Jiang C.., Hu Y.., Zhao, X.;Shi C.., Yu Y.., Liu C.., Tao Y.., Pan H.., Feng Y.., Liu J.., Wu Y.., Wang D.Carbohydr. Polym. 2013. 96:516–521.(16). Kim H.M.; An, C.S.; Jung, K.Y.; Choo, Y.K.; Park, J.K.; Nam, S.Y. Pharmacol. Res. 1999. 40:171–176.(17). Kim S.S.; Son, Y.O.; Chun, J.C.; Kim, S.E.; Chung, G.H.; Hwang, K.J.; Lee, J.C. Redox. Rep. 2005. 10:311–318.(18). Wang Y.B.., Liu Y.F.., Lu X.T.., Yan F.F.., Wang B.., Bai W.W.., Zhao Y.X.PLoS One. 2013. 8:, e54303.(19). Yuan Y.., Hou S.., Lian T.., Han Y.Zhongguo Zhong Yao Za Zhi. 1992. 17:366–368.(20). Zhang R.X.., Li M.X.., Jia Z.P. J.Ethnopharmacol. 2008. 117:199–214.(21). Yoon S.Y.., dela Peña I.C.., Shin C.Y.., Son K.H.., Lee Y.S.., Ryu J.H.., Cheong, J.H.;Ko K.H.Eur. J. Pharmacol. 2011. 659:155–160.(22). Pellmar T. C.., Wilson W.A.Science. 1977. 197:912–914.(23). Larson A.A.., Beitz A. J. J.Neurosci. 1988. 8:3822–3826.(24). West M. R.., Molloy C. R.Anal. Biochem. 1996. 241:51–58.(25). Löscher W.., Fassbender C. P.., Nolting B.Epilepsy Res. 1991. 8:79–94.(26). Rogawski M.A.., Porter R.J.Pharmacol. Rev. 1990. 42:222–286.(27). De Deyn P.P.., Marescau B.., MacDonald R.L.Acta Neurol. Belg. 1989. 90:65–81.(28). Lynch J.W.Physiol. Rev. 2004. 84:1051–1095.
Article(29). Young A.B.., Zukin S.R.., Snyder S.H.Proc. Natl. Acad. Sci. U.S.A. 1974. 71:2246–2250.(30). Rho J.M.., Donevan S.D.., Rogawski M.A.Ann. Neurol. 1994. 35:229–234.(31). Crestani F.., Löw K.., Keist R.., Mandelli M.J.., Möhler H.., Rudolph U.Mol. Pharmacol. 2001. 59:442–445.(32). McBurney R.N.., Barker J. L.Nature. 1978. 274:596–597.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Catalpol and Mannitol, Two Components of Rehmannia glutinosa, Exhibit Anticonvulsant Effects Probably via GABA A Receptor Regulation
- Effect of beta-Adrenergic Blockers on Experimentally-induced Convulsion and Narcosis
- The Effect of Androsterone as the Metabolite of Testosterone to Seizure Suppression
- Effects of kainic Acid-induced seizures on GABA and GABA transporter in the cerebellum of the rat
- Recurrent Early-Life Seizures and Changes in GABAA Receptors Expression in Hippocampus