Clin Exp Otorhinolaryngol.
2017 Mar;10(1):109-114. 10.21053/ceo.2015.01284.
Evaluation of Neck Lymph Node Metastasis on Contrast-Enhanced Ultrasound: An Animal Study
- Affiliations
-
- 1Department of Ultrasound Diagnosis, East Hospital, Tongji University School of Medicine, Shanghai, China.
- 2Department of Otorhinolaryngology-Head and Neck Surgery, East Hospital, Tongji University School of Medicine, Shanghai, China. faust009@163.com mzhx114@163.com
- KMID: 2376417
- DOI: http://doi.org/10.21053/ceo.2015.01284
Abstract
OBJECTIVES
To assess the performance of contrast-enhanced ultrasound (CEUS) intended to differentiate hyperplastic from malignant neck lymph nodes in an animal model.
METHODS
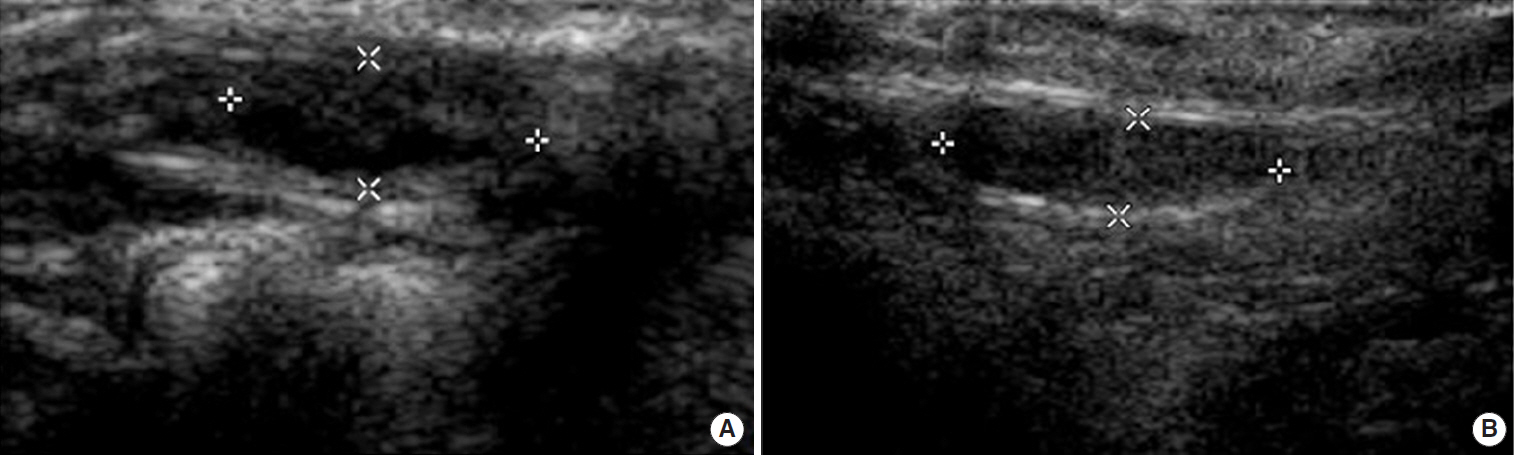
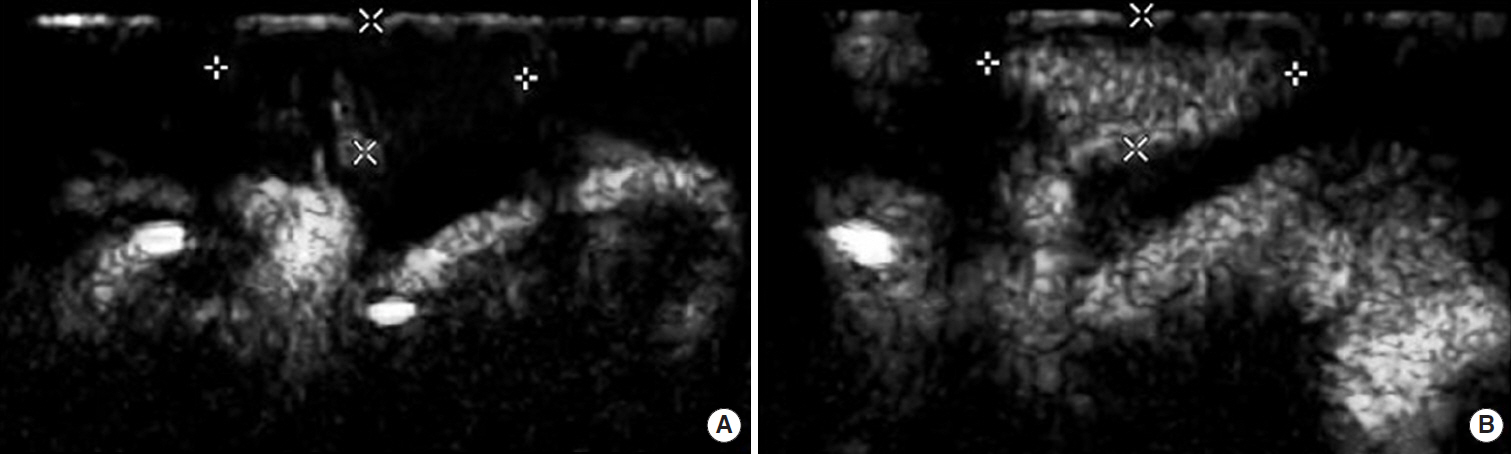
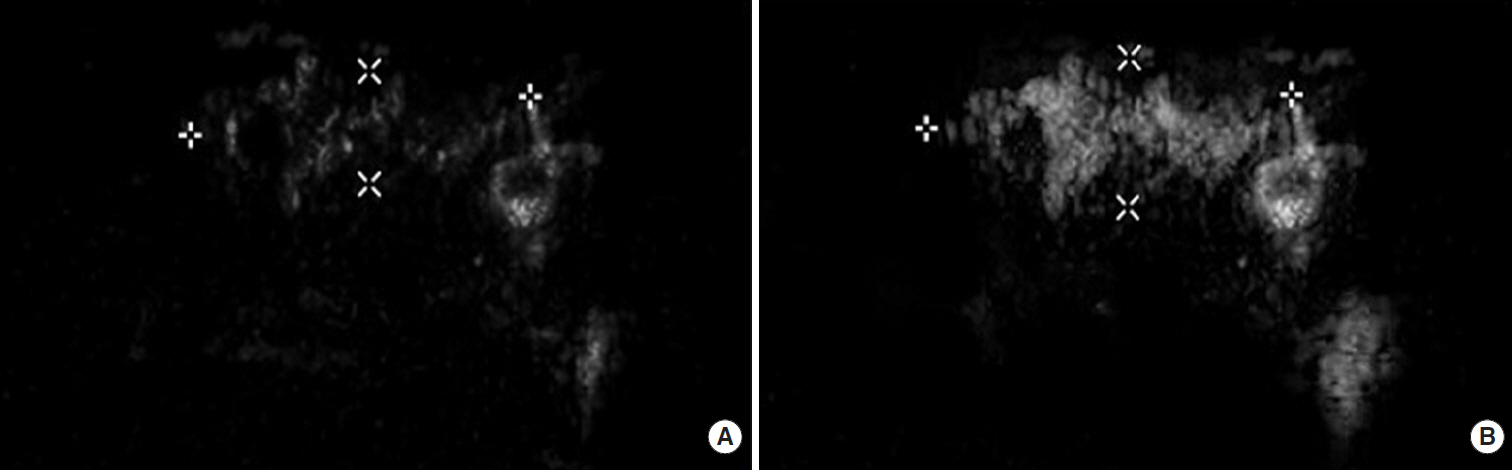
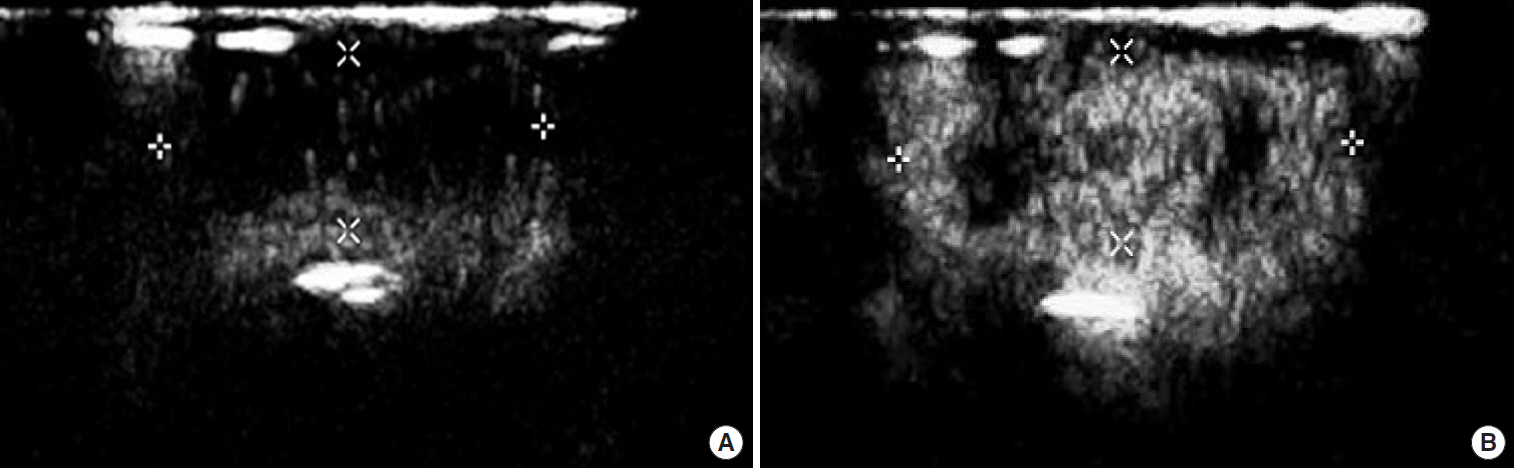
Twenty-four New Zealand rabbits were randomly divided into two groups: neck lymph node metastasis group (12 rabbits) and reactive hyperplastic lymph node group (12 rabbits). Tongue VX2 carcinoma with cervical lymph node metastasis was induced in 12 rabbits by injecting VX2 carcinoma suspension into the left tongue submucosa. Hyperplastic neck lymph nodes were induced by injecting egg yolk in the submandibular region of the rabbits in hyperplastic group. CEUS were performed in both groups before and after intravenous administration of SonoVue. The site, number, echogenicity, longitudinal and transverse nodal dimensions, patterns of enhancement of the neck lymph nodes were observed and recorded.
RESULTS
In both groups only one lymph node was found in the left (tumor) side of the neck. CEUS found 12 of 12 metastatic lymph nodes in metastasis group, and diagnosed 11 of 12 lymph nodes as metastatic. Histopathologic analysis revealed metastatic lesions in all 12 rabbits, each with one lymph node, and all 12 lymph nodes in hyperplastic group is inflammation lymph nodes. All 12 cases in the hyperplastic group showed centripetal homogeneous enhancement while in the metastasis group one case showed centripetal homogeneous enhancement, three cases showed centrifugal heterogeneous enhancement, and eight cases showed diffused heterogeneous enhancement. Only one lymph node was dissected on the left side of the neck in each rabbit in both groups.
CONCLUSION
CEUS can play a role in discriminating metastatic from hyperplastic lymph nodes in head and neck carcinoma.
MeSH Terms
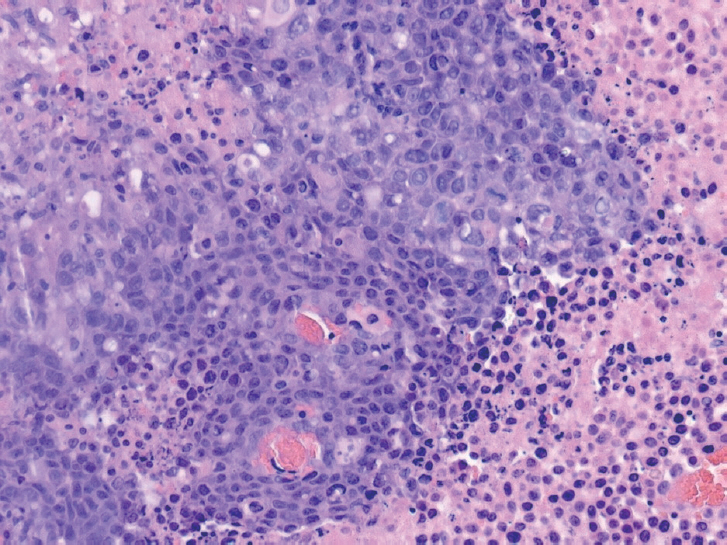
Figure
Reference
-
1. Shoaib T, Soutar DS, MacDonald DG, Camilleri IG, Dunaway DJ, Gray HW, et al. The accuracy of head and neck carcinoma sentinel lymph node biopsy in the clinically N0 neck. Cancer. 2001; Jun. 91(11):2077–83.
Article2. Ahuja A, Ying M. An overview of neck node sonography. Invest Radiol. 2002; Jun. 37(6):333–42.
Article3. Ahuja A, Ying M. Sonography of neck lymph nodes. Part II: abnormal lymph nodes. Clin Radiol. 2003; May. 58(5):359–66.
Article4. Sumi M, Ohki M, Nakamura T. Comparison of sonography and CT for differentiating benign from malignant cervical lymph nodes in patients with squamous cell carcinoma of the head and neck. AJR Am J Roentgenol. 2001; Apr. 176(4):1019–24.5. Rubaltelli L, Corradin S, Dorigo A, Tregnaghi A, Adami F, Rossi CR, et al. Automated quantitative evaluation of lymph node perfusion on contrast-enhanced sonography. AJR Am J Roentgenol. 2007; Apr. 188(4):977–83.
Article6. Santamaria G, Velasco M, Farre X, Vanrell JA, Cardesa A, Fernandez PL. Power Doppler sonography of invasive breast carcinoma: does tumor vascularization contribute to prediction of axillary status? Radiology. 2005; Feb. 234(2):374–80.
Article7. Rubaltelli L, Khadivi Y, Tregnaghi A, Stramare R, Ferro F, Borsato S, et al. Evaluation of lymph node perfusion using continuous mode harmonic ultrasonography with a second-generation contrast agent. J Ultrasound Med. 2004; Jun. 23(6):829–36.
Article8. Dunne AA, Mandic R, Ramaswamy A, Plehn S, Schulz S, Lippert BM, et al. Lymphogenic metastatic spread of auricular VX2 carcinoma in New Zealand white rabbits. Anticancer Res. 2002; Nov-Dec. 22(6A):3273–9.9. Ying HY, Wu HT, Zhou L. Establishment of the deep cervical lymph node metastasis model of tongue VX2 carcinoma and observation of its metastatic features. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2008; Oct. 43(10):778–81.10. Gorce JM, Arditi M, Schneider M. Influence of bubble size distribution on the echogenicity of ultrasound contrast agents: a study of SonoVue. Invest Radiol. 2000; Nov. 35(11):661–71.11. Yoshida K, Kashima K, Suenaga S, Nomi N, Shuto J, Suzuki M. Immunohistochemical detection of cervical lymph node micrometastases from T2N0 tongue cancer. Acta Otolaryngol. 2005; Jun. 125(6):654–8.
Article12. Kau RJ, Alexiou C, Stimmer H, Arnold W. Diagnostic procedures for detection of lymph node metastases in cancer of the larynx. ORL J Otorhinolaryngol Relat Spec. 2000; Jul-Aug. 62(4):199–203.
Article13. Gadre A, Briner W, O’Leary M. A scanning electron microscope study of the human cervical lymph node. Acta Otolaryngol. 1994; Jan. 114(1):87–90.
Article14. Steinkamp HJ, Wissgott C, Rademaker J, Felix R. Current status of power Doppler and color Doppler sonography in the differential diagnosis of lymph node lesions. Eur Radiol. 2002; Jul. 12(7):1785–93.
Article15. Yu M, Liu Q, Song HP, Han ZH, Su HL, He GB, et al. Clinical application of contrast-enhanced ultrasonography in diagnosis of superficial lymphadenopathy. J Ultrasound Med. 2010; May. 29(5):735–40.
Article16. Ouyang Q, Chen L, Zhao H, Xu R, Lin Q. Detecting metastasis of lymph nodes and predicting aggressiveness in patients with breast carcinomas. J Ultrasound Med. 2010; Mar. 29(3):343–52.
Article17. Yang WT, Metreweli C, Lam PK, Chang J. Benign and malignant breast masses and axillary nodes: evaluation with echo-enhanced color power Doppler US. Radiology. 2001; Sep. 220(3):795–802.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasonographic Evaluation of Cervical Lymph Nodes
- Supraclavicular Lymph Node Metastasis from Various Malignancies: Assessment with 18F-Fluorodeoxyglucose Positron Emission Tomography/CT, Contrast-Enhanced CT and Ultrasound
- Sentinel Lymph Node Biopsy in the Oral Cavity Cancer
- Ultrasonography for Staging Axillary Lymph Node in Breast Cancer Patients
- Retropharyngeal Lymph Node Metastasis of Thyroid Papillary Carcinoma