Investig Magn Reson Imaging.
2017 Mar;21(1):34-37. 10.13104/imri.2017.21.1.34.
A Case of Widespread Cavernous Malformations of the Central Nervous System Associated with Acute Neurologic Deficit
- Affiliations
-
- 1Department of Neurology, College of Medicine, Kyung Hee University, Seoul, Korea.
- 2Department of Neurology, Chung Hospital, Seongnam-si, Gyeonggi-do, Korea. dkja111@gmail.com
- KMID: 2376267
- DOI: http://doi.org/10.13104/imri.2017.21.1.34
Abstract
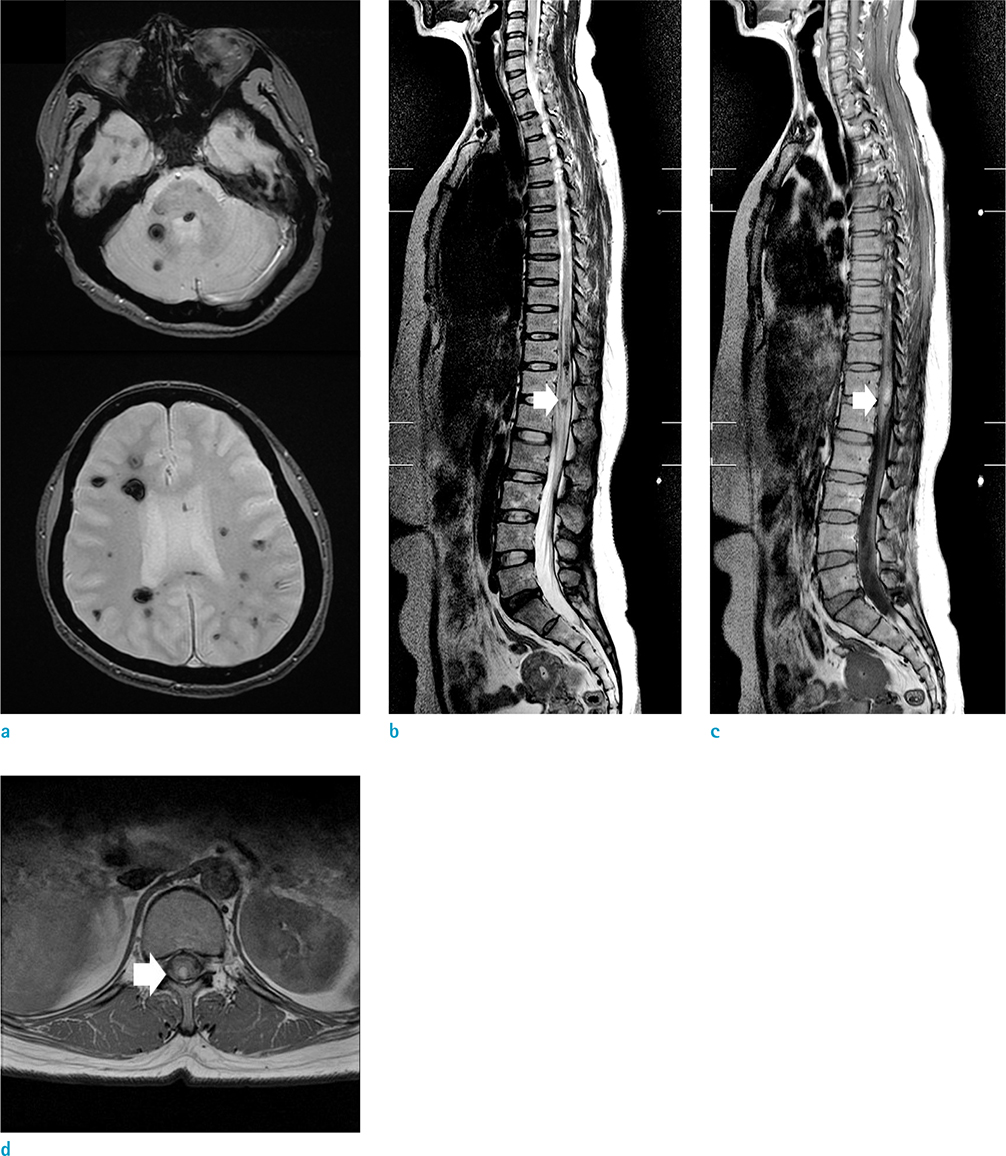
- A 45-year-old female visited our clinic due to sudden right leg weakness and sensory loss. Brain and spinal cord magnetic resonance imaging showed widespread cavernous malformations. Cavernous malformation in L1 spine area was accompanied by a subacute stage hematoma with perilesional edema. Sensory loss subsided after corticosteroid therapy. Usually, neurologic deficit by spinal cavernous malformation appears more chronically in the adults compared to children. Treatment options are difficult to establish in a case with multiple cavernous malformations. Identifying hemorrhagic lesions by extensive neuroimaging evaluation could be helpful to select the treatment target for cavernous malformation.
MeSH Terms
Figure
Reference
-
1. Zevgaridis D, Medele RJ, Hamburger C, Steiger HJ, Reulen HJ. Cavernous haemangiomas of the spinal cord. A review of 117 cases. Acta Neurochir (Wien). 1999; 141:237–245.2. Santoro A, Piccirilli M, Brunetto GM, Delfini R, Cantore G. Intramedullary cavernous angioma of the spinal cord in a pediatric patient, with multiple cavernomas, familial occurrence and partial spontaneous regression: case report and review of the literature. Childs Nerv Syst. 2007; 23:1319–1326.3. Cornips EM, Vinken PA, Ter Laak-Poort M, Beuls EA, Weber J, Vles JS. Intramedullary cavernoma presenting with hematomyelia: report of two girls. Childs Nerv Syst. 2010; 26:391–398.4. Labauge P, Bouly S, Parker F, et al. Outcome in 53 patients with spinal cord cavernomas. Surg Neurol. 2008; 70:176–181. discussion 181.5. Kondziolka D, Lunsford LD, Kestle JR. The natural history of cerebral cavernous malformations. J Neurosurg. 1995; 83:820–824.6. Robinson JR, Awad IA, Little JR. Natural history of the cavernous angioma. J Neurosurg. 1991; 75:709–714.7. Kim KM, Chung CK, Huh W, et al. Clinical outcomes of conservative management of spinal cord cavernous angiomas. Acta Neurochir (Wien). 2013; 155:1209–1214.8. Dubovsky J, Zabramski JM, Kurth J, et al. A gene responsible for cavernous malformations of the brain maps to chromosome 7q. Hum Mol Genet. 1995; 4:453–458.9. Mindea SA, Yang BP, Shenkar R, Bendok B, Batjer HH, Awad IA. Cerebral cavernous malformations: clinical insights from genetic studies. Neurosurg Focus. 2006; 21:e1.