Korean J Pain.
2017 Apr;30(2):104-115. 10.3344/kjp.2017.30.2.104.
The radiation safety education and the pain physicians' efforts to reduce radiation exposure
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Konkuk University School of Medicine, Seoul, Korea. painfree@kuh.ac.kr
- KMID: 2376046
- DOI: http://doi.org/10.3344/kjp.2017.30.2.104
Abstract
- BACKGROUND
C-arm fluoroscopy equipment is important for interventional pain management and can cause radiation injury to physicians and patients. We compared radiation safety education and efforts to reduce the radiation exposure of pain specialists.
METHODS
A survey of 49 pain specialists was conducted anonymously in 2016. The questionnaire had 16 questions. That questionnaire was about radiation safety knowledge and efforts to reduce exposure. We investigated the correlation between radiation safety education and efforts of radiation protection. We compared the results from 2016 and a published survey from 2011.
RESULTS
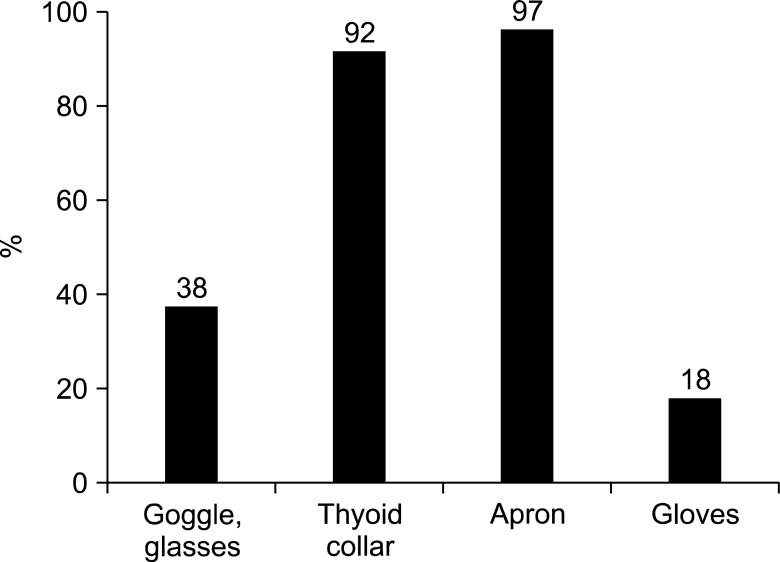
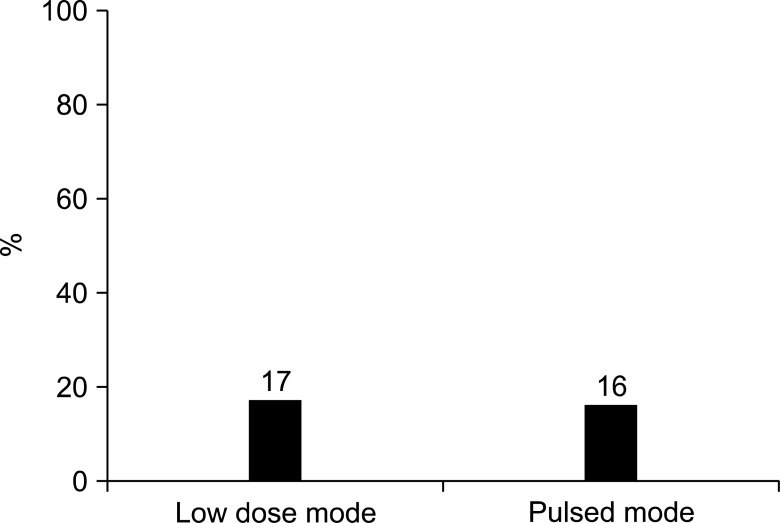
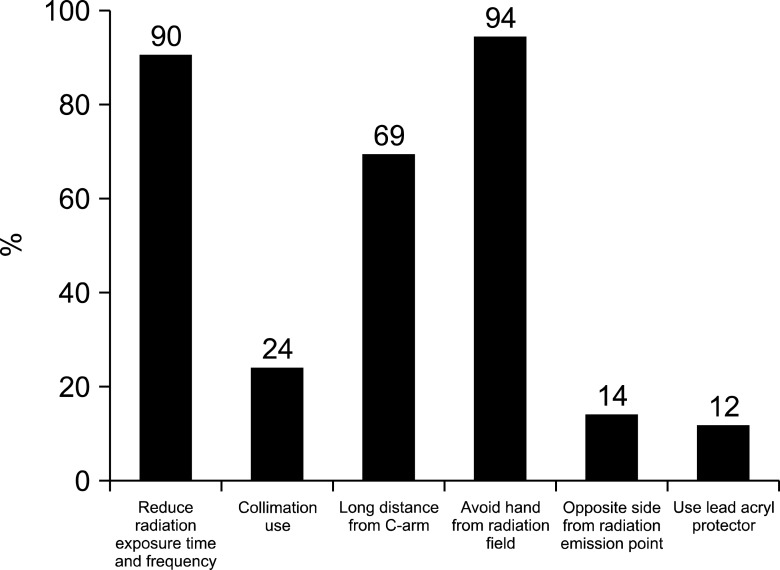
According to the 2016 survey, all respondents used C-arm fluoroscopy in pain interventions. Nineteen respondents (39%) had received radiation safety education. Physicians had insufficient knowledge about radiation safety. When the radiation safety education group and the non-education group are compared, there was no significant difference in efforts to reduce radiation exposure and radiation safety knowledge. When the 2011 and 2016 surveys were compared, the use of low dose mode (P = 0.000) and pulsed mode had increased significantly (P = 0.001). The number checking for damage to radiation protective garments (P = 0.000) and use of the dosimeter had also increased significantly (P = 0.009). But there was no significant difference in other efforts to reduce radiation exposure.
CONCLUSIONS
Pain physicians seem to lack knowledge of radiation safety and the number of physicians receiving radiation safety education is low. According to this study, education does not lead to practice. Therefore, pain physicians should receive regular radiation safety education and the education should be mandatory.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Three principles for radiation safety: time, distance, and shielding
Jae Hun Kim
Korean J Pain. 2018;31(3):145-146. doi: 10.3344/kjp.2018.31.3.145.Radiation safety: a focus on lead aprons and thyroid shields in interventional pain management
Bo Kyung Cheon, Cho Long Kim, Ka Ram Kim, Min Hye Kang, Jeong Ae Lim, Nam Sik Woo, Ka Young Rhee, Hae Kyoung Kim, Jae Hun Kim
Korean J Pain. 2018;31(4):244-252. doi: 10.3344/kjp.2018.31.4.244.Radiation safety for pain physicians: principles and recommendations
Sewon Park, Minjung Kim, Jae Hun Kim
Korean J Pain. 2022;35(2):129-139. doi: 10.3344/kjp.2022.35.2.129.
Reference
-
1. Sheyn DD, Racadio JM, Ying J, Patel MN, Racadio JM, Johnson ND. Efficacy of a radiation safety education initiative in reducing radiation exposure in the pediatric IR suite. Pediatr Radiol. 2008; 38:669–674. PMID: 18414841.
Article2. Kim S, Shin JH, Lee JW, Kang HS, Lee GY, Ahn JM. Factors affecting radiation exposure during lumbar epidural steroid injection: a prospective study in 759 patients. Korean J Radiol. 2016; 17:405–412. PMID: 27134528.
Article3. Fishman SM, Smith H, Meleger A, Seibert JA. Radiation safety in pain medicine. Reg Anesth Pain Med. 2002; 27:296–305. PMID: 12016604.
Article4. Broadman LM, Navalgund YA, Hawkinberry DW 2nd. Radiation risk management during fluoroscopy for interventional pain medicine physicians. Curr Pain Headache Rep. 2004; 8:49–55. PMID: 14731383.
Article5. Schueler BA. Operator shielding: how and why. Tech Vasc Interv Radiol. 2010; 13:167–171. PMID: 20723831.
Article6. Ryu JS, Baek SW, Jung CH, Cho SJ, Jung EG, Kim HK, et al. The survey about the degree of damage of radiation-protective shields in operation room. Korean J Pain. 2013; 26:142–147. PMID: 23614075.
Article7. Cho JH, Kim JY, Kang JE, Park PE, Kim JH, Lim JA, et al. A study to compare the radiation absorbed dose of the C-arm fluoroscopic modes. Korean J Pain. 2011; 24:199–204. PMID: 22220241.
Article8. Baek SW, Ryu JS, Jung CH, Lee JH, Kwon WK, Woo NS, et al. A randomized controlled trial about the levels of radiation exposure depends on the use of collimation C-arm fluoroscopic-guided medial branch block. Korean J Pain. 2013; 26:148–153. PMID: 23614076.
Article9. Kim AN, Chang YJ, Cheon BK, Kim JH. How effective are radiation reducing gloves in C-arm fluoroscopy-guided pain interventions? Korean J Pain. 2014; 27:145–151. PMID: 24748943.
Article10. Park PE, Park JM, Kang JE, Cho JH, Cho SJ, Kim JH, et al. Radiation safety and education in the applicants of the final test for the expert of pain medicine. Korean J Pain. 2012; 25:16–21. PMID: 22259711.
Article11. Cousins C, Sharp C. Medical interventional procedures-reducing the radiation risks. Clin Radiol. 2004; 59:468–473. PMID: 15145716.
Article12. Ploussi A, Efstathopoulos EP. Importance of establishing radiation protection culture in radiology department. World J Radiol. 2016; 8:142–147. PMID: 26981223.
Article13. Mahajan A, Samuel S, Saran AK, Mahajan MK, Mam MK. Occupational radiation exposure from C arm fluoroscopy during common orthopaedic surgical procedures and its prevention. J Clin Diagn Res. 2015; 9:RC01–RC04.
Article14. Wagner M, Duwenkamp C, Ludwig W, Dresing K, Bott OJ. An approach to simulate and visualize intraoperative scattered radiation exposure to improve radiation protection training. Stud Health Technol Inform. 2010; 160:625–628. PMID: 20841762.15. Yamashita K, Higashino K, Wada K, Morimoto M, Abe M, Takata Y, et al. Radiation exposure to the surgeon and patient during a fluoroscopic procedure: how high is the exposure dose? A cadaveric study. Spine (Phila Pa 1976). 2016; 41:1254–1256. PMID: 26953671.16. Meisinger QC, Stahl CM, Andre MP, Kinney TB, Newton IG. Radiation protection for the fluoroscopy operator and staff. AJR Am J Roentgenol. 2016; [in press].
Article17. Zhou Y, Singh N, Abdi S, Wu J, Crawford J, Furgang FA. Fluoroscopy radiation safety for spine interventional pain procedures in university teaching hospitals. Pain Physician. 2005; 8:49–53. PMID: 16850042.18. Nicol AL, Benzon HT, Liu BP. Radiation exposure in interventional pain management: we still have much to learn. Pain Pract. 2015; 15:389–392. PMID: 26037659.
Article19. Frazier TH, Richardson JB, Fabré VC, Callen JP. Fluoroscopy-induced chronic radiation skin injury: a disease perhaps often overlooked. Arch Dermatol. 2007; 143:637–640. PMID: 17515515.20. Mettler FA Jr, Koenig TR, Wagner LK, Kelsey CA. Radiation injuries after fluoroscopic procedures. Semin Ultrasound CT MR. 2002; 23:428–442. PMID: 12509113.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiation safety for pain physicians: principles and recommendations
- Radiation Safety and Education in the Applicants of the Final Test for the Expert of Pain Medicine
- Radiation exposure and protection for eyes in pain management
- Radiation safety: a focus on lead aprons and thyroid shields in interventional pain management
- Current status of medical radiation exposure and regulation efforts