J Clin Neurol.
2017 Apr;13(2):187-195. 10.3988/jcn.2017.13.2.187.
Total Cerebral Small-Vessel Disease Score is Associated with Mortality during Follow-Up after Acute Ischemic Stroke
- Affiliations
-
- 1Department of Neurology, Yonsei University College of Medicine, Seoul, Korea. neuro05@yuhs.ac
- 2Department of Neurology, Ewha Womans University School of Medicine, Seoul, Korea.
- 3Department of Neurology, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- 4Department of Biostatistics, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2376021
- DOI: http://doi.org/10.3988/jcn.2017.13.2.187
Abstract
- BACKGROUND AND PURPOSE
The recently developed total cerebral small-vessel disease (CSVD) score might appropriately reflect the total burden or severity of CSVD. We investigated whether the total CSVD score is associated with long-term outcomes during follow-up in patients with acute ischemic stroke.
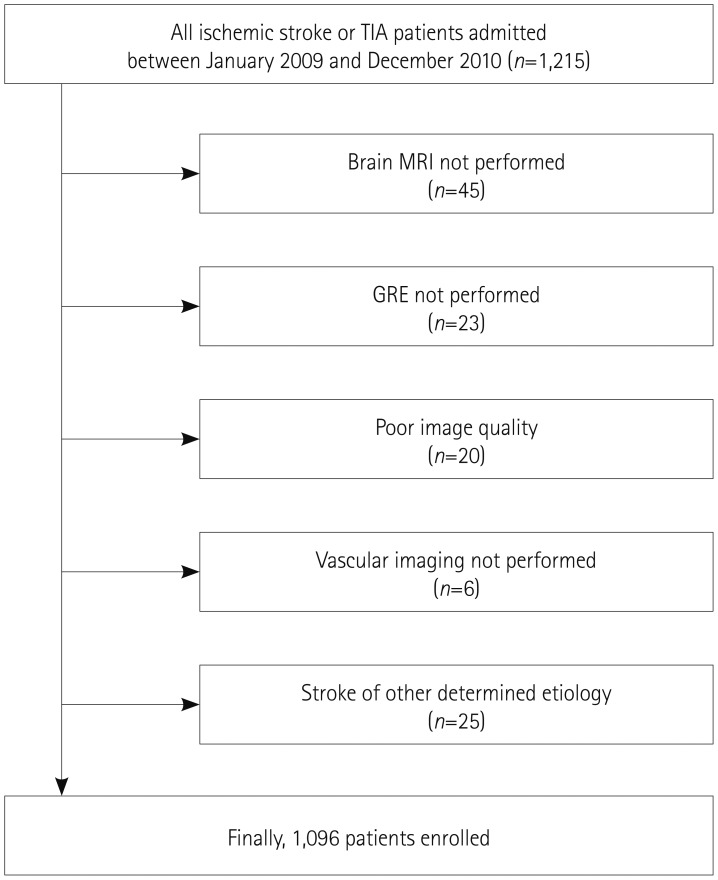
METHODS
In total, 1,096 consecutive patients with acute ischemic stroke who underwent brain magnetic resonance imaging were enrolled. We calculated the total CSVD score for each patient after determining the burden of cerebral microbleeds (CMBs), high-grade white-matter hyperintensities (HWHs), high-grade perivascular spaces (HPVSs), and asymptomatic lacunar infarctions (ALIs). We recorded the date and cause of death for all of the patients using data from the Korean National Statistical Office. We compared the long-term mortality rate with the total CSVD score using Cox proportional-hazards models.
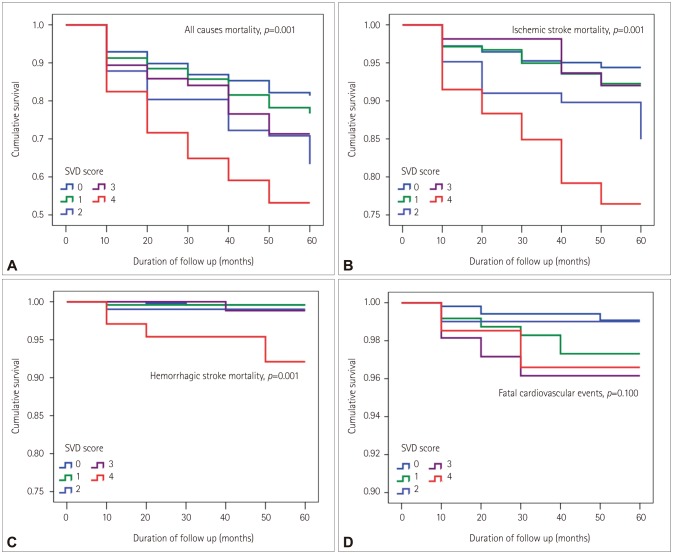
RESULTS
CMBs were found in 26.8% of the subjects (294/1,096), HWHs in 16.4% (180/1,096), HPVSs in 19.3% (211/1,096), and ALIs in 38.0% (416/1,096). After adjusting for age, sex, and variables that were significant at p<0.1 in the univariate analysis, the total CSVD score was independently associated with long-term death from all causes [hazard ratio (HR)=1.18 per point, 95% confidence interval (CI)=1.07-1.30], ischemic stroke (HR=1.20 per point, 95% CI=1.01-1.42), and hemorrhagic stroke (HR=2.05 per point, 95% CI=1.30-3.22), but not with fatal cardiovascular events (HR=1.17 per point, 95% CI=0.82-1.67).
CONCLUSIONS
The total CSVD score is a potential imaging biomarker for predicting mortality during follow-up in patients with acute ischemic stroke.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Interarm Blood Pressure Difference has Various Associations with the Presence and Burden of Cerebral Small-Vessel Diseases in Noncardioembolic Stroke Patients
Yoonkyung Chang, Seung Ah Lee, Sue Hyun Lee, Eun Hye Lee, Yong-Jae Kim, Tae-Jin Song
J Clin Neurol. 2019;15(2):159-167. doi: 10.3988/jcn.2019.15.2.159.
Reference
-
1. Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010; 9:689–701. PMID: 20610345.
Article2. Greenberg SM, Vernooij MW, Cordonnier C, Viswanathan A, Al-Shahi Salman R, Warach S, et al. Cerebral microbleeds: a guide to detection and interpretation. Lancet Neurol. 2009; 8:165–174. PMID: 19161908.
Article3. Doubal FN, MacLullich AM, Ferguson KJ, Dennis MS, Wardlaw JM. Enlarged perivascular spaces on MRI are a feature of cerebral small vessel disease. Stroke. 2010; 41:450–454. PMID: 20056930.
Article4. Kim BJ, Lee SH. Cerebral microbleeds: their associated factors, radiologic findings, and clinical implications. J Stroke. 2013; 15:153–163. PMID: 24396809.
Article5. Kalaria RN, Erkinjuntti T. Small vessel disease and subcortical vascular dementia. J Clin Neurol. 2006; 2:1–11. PMID: 20396480.
Article6. Staals J, Makin SD, Doubal FN, Dennis MS, Wardlaw JM. Stroke subtype, vascular risk factors, and total MRI brain small-vessel disease burden. Neurology. 2014; 83:1228–1234. PMID: 25165388.
Article7. Huijts M, Duits A, van Oostenbrugge RJ, Kroon AA, de Leeuw PW, Staals J. Accumulation of MRI markers of cerebral small vessel disease is associated with decreased cognitive function. A study in firstever lacunar stroke and hypertensive patients. Front Aging Neurosci. 2013; 5:72. PMID: 24223555.
Article8. Lee BI, Nam HS, Heo JH, Kim DI. Yonsei Stroke Registry. Analysis of 1,000 patients with acute cerebral infarctions. Cerebrovasc Dis. 2001; 12:145–151. PMID: 11641577.9. Choi HY, Seo JH, Yang JH, Kim YD, Jung YH, Cho HJ, et al. Beneficial effects of stroke-unit care in stroke patients with atrial fibrillation. Yonsei Med J. 2013; 54:301–305. PMID: 23364960.
Article10. Song TJ, Kim J, Lee HS, Nam CM, Nam HS, Kim EH, et al. Differential impact of unrecognised brain infarction on stroke outcome in non-valvular atrial fibrillation. Thromb Haemost. 2014; 112:1312–1318. PMID: 25231184.
Article11. Song TJ, Kim J, Song D, Nam HS, Kim YD, Lee HS, et al. Association of cerebral microbleeds with mortality in stroke patients having atrial fibrillation. Neurology. 2014; 83:1308–1315. PMID: 25186853.
Article12. Song TJ, Kim J, Kim YD, Nam HS, Lee HS, Nam CM, et al. The distribution of cerebral microbleeds determines their association with arterial stiffness in non-cardioembolic acute stroke patients. Eur J Neurol. 2014; 21:463–469. PMID: 24330330.
Article13. Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013; 12:822–838. PMID: 23867200.
Article14. Kim YD, Jung YH, Saposnik G. Traditional risk factors for stroke in East Asia. J Stroke. 2016; 18:273–285. PMID: 27733028.
Article15. Oh MS, Yu KH, Lee JH, Jung S, Ko IS, Shin JH, et al. Validity and reliability of a Korean version of the national institutes of health stroke scale. J Clin Neurol. 2012; 8:177–183. PMID: 23091526.
Article16. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41. PMID: 7678184.
Article17. Kim HC, Choi DP, Ahn SV, Nam CM, Suh I. Six-year survival and causes of death among stroke patients in Korea. Neuroepidemiology. 2009; 32:94–100. PMID: 19039241.
Article18. Adachi T, Kobayashi S, Yamaguchi S. Frequency and pathogenesis of silent subcortical brain infarction in acute first-ever ischemic stroke. Intern Med. 2002; 41:103–108. PMID: 11868595.
Article19. Vermeer SE, Longstreth WT Jr, Koudstaal PJ. Silent brain infarcts: a systematic review. Lancet Neurol. 2007; 6:611–619. PMID: 17582361.
Article20. Klarenbeek P, van Oostenbrugge RJ, Rouhl RP, Knottnerus IL, Staals J. Ambulatory blood pressure in patients with lacunar stroke: association with total MRI burden of cerebral small vessel disease. Stroke. 2013; 44:2995–2999. PMID: 23982717.21. Arsava EM, Rahman R, Rosand J, Lu J, Smith EE, Rost NS, et al. Severity of leukoaraiosis correlates with clinical outcome after ischemic stroke. Neurology. 2009; 72:1403–1410. PMID: 19380699.
Article22. Lim JS, Hong KS, Kim GM, Bang OY, Bae HJ, Kwon HM, et al. Cerebral microbleeds and early recurrent stroke after transient ischemic attack: results from the Korean Transient Ischemic Attack Expression Registry. JAMA Neurol. 2015; 72:301–308. PMID: 25580844.23. Soo YO, Yang SR, Lam WW, Wong A, Fan YH, Leung HH, et al. Risk vs benefit of anti-thrombotic therapy in ischaemic stroke patients with cerebral microbleeds. J Neurol. 2008; 255:1679–1686. PMID: 19156486.
Article24. Altmann-Schneider I, Trompet S, de Craen AJ, van Es AC, Jukema JW, Stott DJ, et al. Cerebral microbleeds are predictive of mortality in the elderly. Stroke. 2011; 42:638–644. PMID: 21233474.
Article25. Bokura H, Kobayashi S, Yamaguchi S, Iijima K, Nagai A, Toyoda G, et al. Silent brain infarction and subcortical white matter lesions increase the risk of stroke and mortality: a prospective cohort study. J Stroke Cerebrovasc Dis. 2006; 15:57–63. PMID: 17904049.
Article26. Montagne A, Pa J, Zlokovic BV. Vascular plasticity and cognition during normal aging and dementia. JAMA Neurol. 2015; 72:495–496. PMID: 25751405.
Article27. Kim YD, Song D, Kim EH, Lee KJ, Lee HS, Nam CM, et al. Long-term mortality according to the characteristics of early neurological deterioration in ischemic stroke patients. Yonsei Med J. 2014; 55:669–675. PMID: 24719133.
Article28. Kim J, Song TJ, Song D, Yoo J, Baek JH, Lee HS, et al. Prognostic value of urine dipstick proteinuria on mortality after acute ischemic stroke. Atherosclerosis. 2016; 253:118–123. PMID: 27599365.
Article29. Kim YD, Song D, Nam HS, Choi D, Kim JS, Kim BK, et al. Increased risk of cardiovascular events in stroke patients who had not undergone evaluation for coronary artery disease. Yonsei Med J. 2017; 58:114–122. PMID: 27873503.
Article30. Oh MS, Yu KH, Roh JK, Lee BC. Korean Stroke Registry Study Group. Gender differences in the mortality and outcome of stroke patients in Korea. Cerebrovasc Dis. 2009; 28:427–434. PMID: 19738370.
Article31. Wong KS, Li H. Long-term mortality and recurrent stroke risk among Chinese stroke patients with predominant intracranial atherosclerosis. Stroke. 2003; 34:2361–2366. PMID: 12947158.
Article32. Putaala J, Haapaniemi E, Kurkinen M, Salonen O, Kaste M, Tatlisumak T. Silent brain infarcts, leukoaraiosis, and long-term prognosis in young ischemic stroke patients. Neurology. 2011; 76:1742–1749. PMID: 21576692.
Article33. Charidimou A, Kakar P, Fox Z, Werring DJ. Cerebral microbleeds and recurrent stroke risk: systematic review and meta-analysis of prospective ischemic stroke and transient ischemic attack cohorts. Stroke. 2013; 44:995–1001. PMID: 23493732.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebral Small Vessel Disease and Chronic Kidney Disease
- Association between Aortic Atheroma and Cerebral Small Vessel Disease in Patients with Ischemic Stroke
- Influence of 3 Stigmas of Small Vessel Disease on FLAIR Change in Acute Ischemic Stroke: Case-Control Study
- Induced Hypertension Using Phenylephrine in Patients with Acute Ischemic Stroke: A Case Report
- Hemispheric Differences in Ischemic Stroke: Is Left-Hemisphere Stroke More Common?