J Clin Neurol.
2017 Apr;13(2):162-169. 10.3988/jcn.2017.13.2.162.
Impact of Baseline Ischemia on Outcome in Older Patients Undergoing Endovascular Therapy for Acute Ischemic Stroke
- Affiliations
-
- 1Cerebrovascular Center, Kyungpook National University School of Medicine and Hospital, Daegu, Korea. yangha.hwang@gmail.com
- 2Department of Neurology, Kyungpook National University School of Medicine and Hospital, Daegu, Korea.
- 3Department of Radiology, Kyungpook National University School of Medicine and Hospital, Daegu, Korea.
- 4Department of Neurosurgery, Kyungpook National University School of Medicine and Hospital, Daegu, Korea.
- 5UCLA Stroke Center, University of California, Los Angeles, Los Angeles, CA, USA.
- KMID: 2376017
- DOI: http://doi.org/10.3988/jcn.2017.13.2.162
Abstract
- BACKGROUND AND PURPOSE
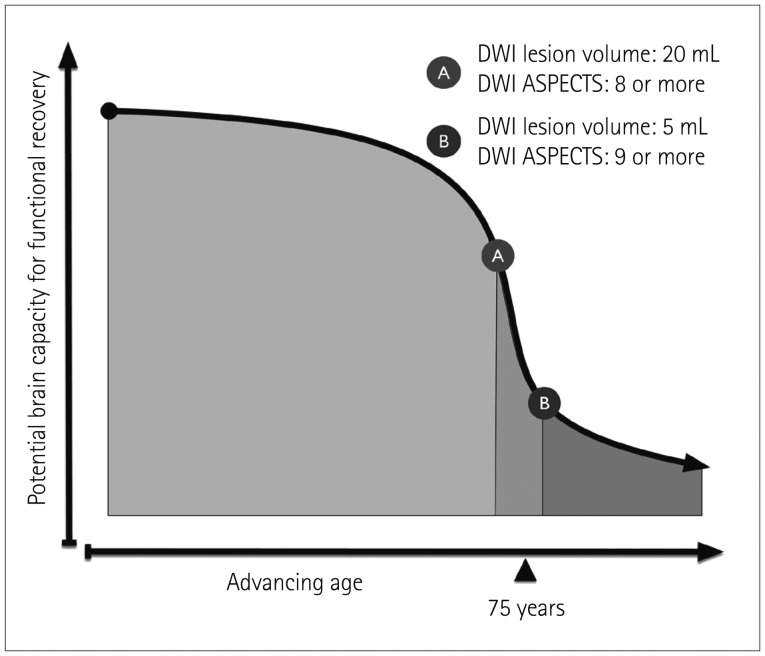
The outcome for older stroke patients who undergo endovascular revascularization remains unsatisfactory. We aimed to determine the effect of the extent of baseline ischemia on outcome according to age, testing the hypothesis that the restorative capacity for recovery is only marginal in older patients.
METHODS
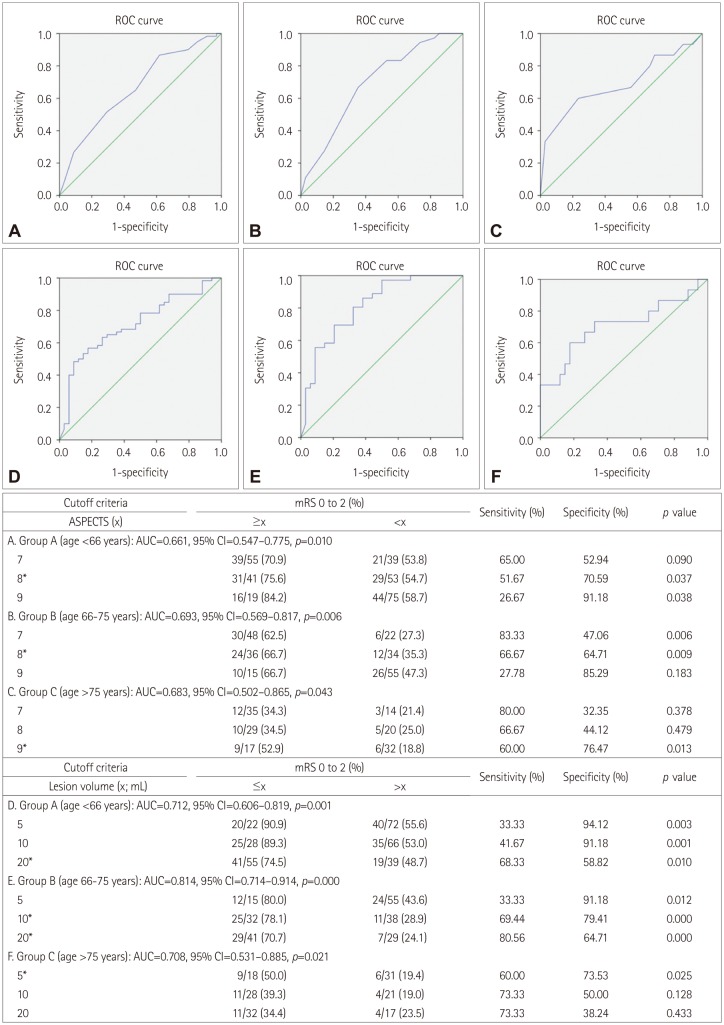
Two hundred and thirteen patients who underwent endovascular revascularization due to occlusion in the M1 segment of the middle cerebral artery (with or without internal carotid artery occlusions) were selected for analysis. Patients were categorized into three age groups: group A (<66 years), group B (66-75 years), and group C (>75 years). Using pretreatment diffusion-weighted imaging (DWI), the Alberta Stroke Program Early CT Score (ASPECTS) and lesion volume were independently measured and analyzed in relation to a favorable outcome.
RESULTS
A favorable outcome was achieved in 111 of 213 patients overall: in 60 of the 94 (63.8%) patients in group A, in 36 of the 70 (51.4%) patients in group B, and in 15 of the 49 (30.6%) patients in group C (p=0.001). In older stroke patients (group C), a DWI ASPECTS ≥9 and lesion volume ≤5 mL were found to predict a favorable outcome, which was more restrictive than the cutoffs for their younger counterparts (groups A and B; DWI ASPECTS ≥8 and lesion volume ≤20 mL).
CONCLUSIONS
The age-adjusted pretreatment DWI lesion volume and ASPECTS may represent useful surrogate markers for functional outcome according to age. The use of more-restrictive inclusion criteria for older stroke patients could be warranted, although larger studies are necessary to confirm these findings.
Keyword
MeSH Terms
Figure
Reference
-
1. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20. PMID: 25517348.2. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 372:1009–1018. PMID: 25671797.
Article3. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030. PMID: 25671798.4. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015; 372:2285–2295. PMID: 25882376.
Article5. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372:2296–2306. PMID: 25882510.
Article6. Hong KS, Bang OY, Kang DW, Yu KH, Bae HJ, Lee JS, et al. Stroke statistics in Korea: part I. Epidemiology and risk factors: a report from the Korean Stroke Society and Clinical Research Center for Stroke. J Stroke. 2013; 15:2–20. PMID: 24324935.
Article7. Kim D, Ford GA, Kidwell CS, Starkman S, Vinuela F, Duckwiler GR, et al. Intra-arterial thrombolysis for acute stroke in patients 80 and older: a comparison of results in patients younger than 80 years. AJNR Am J Neuroradiol. 2007; 28:159–163. PMID: 17213448.8. Qureshi AI, Suri MF, Georgiadis AL, Vazquez G, Janjua NA. Intra-arterial recanalization techniques for patients 80 years or older with acute ischemic stroke: pooled analysis from 4 prospective studies. AJNR Am J Neuroradiol. 2009; 30:1184–1189. PMID: 19342542.
Article9. Loh Y, Kim D, Shi ZS, Tateshima S, Vespa PM, Gonzalez NR, et al. Higher rates of mortality but not morbidity follow intracranial mechanical thrombectomy in the elderly. AJNR Am J Neuroradiol. 2010; 31:1181–1185. PMID: 20395387.
Article10. Mazighi M, Labreuche J, Meseguer E, Serfaty JM, Laissy JP, Lavallée PC, et al. Impact of a combined intravenous/intra-arterial approach in octogenarians. Cerebrovasc Dis. 2011; 31:559–565. PMID: 21487220.11. Mono ML, Romagna L, Jung S, Arnold M, Galimanis A, Fischer U, et al. Intra-arterial thrombolysis for acute ischemic stroke in octogenarians. Cerebrovasc Dis. 2012; 33:116–122. PMID: 22179504.
Article12. Chandra RV, Leslie-Mazwi TM, Oh DC, Chaudhry ZA, Mehta BP, Rost NS, et al. Elderly patients are at higher risk for poor outcomes after intra-arterial therapy. Stroke. 2012; 43:2356–2361. PMID: 22744644.
Article13. Johnson JN, Haussen DC, Elhammady MS, Pao CL, Yavagal DR, Aziz-Sultan MA. Poor outcomes of elderly patients undergoing multimodality intra-arterial therapy for acute ischemic stroke. Clin Neurol Neurosurg. 2014; 123:136–141. PMID: 25012026.
Article14. Parrilla G, Carreón E, Zamarro J, Espinosa de Rueda M, García-Villalba B, Marín F, et al. Recanalization and mortality rates of thrombectomy with stent-retrievers in octogenarian patients with acute ischemic stroke. Cardiovasc Intervent Radiol. 2015; 38:288–294. PMID: 24923241.
Article15. Singer OC, Haring HP, Trenkler J, Nolte CH, Bohner G, Reich A, et al. Age dependency of successful recanalization in anterior circulation stroke: the ENDOSTROKE study. Cerebrovasc Dis. 2013; 36:437–445. PMID: 24281318.
Article16. Petcu EB, Sfredel V, Platt D, Herndon JG, Kessler C, Popa-Wagner A. Cellular and molecular events underlying the dysregulated response of the aged brain to stroke: a mini-review. Gerontology. 2008; 54:6–17. PMID: 18160818.
Article17. Inoue M, Olivot JM, Labreuche J, Mlynash M, Tai W, Albucher JF, et al. Impact of diffusion-weighted imaging Alberta stroke program early computed tomography score on the success of endovascular reperfusion therapy. Stroke. 2014; 45:1992–1998. PMID: 24923724.
Article18. Yoo AJ, Zaidat OO, Chaudhry ZA, Berkhemer OA, González RG, Goyal M, et al. Impact of pretreatment noncontrast CT Alberta Stroke Program Early CT Score on clinical outcome after intra-arterial stroke therapy. Stroke. 2014; 45:746–751. PMID: 24503670.
Article19. Ribo M, Flores A, Mansilla E, Rubiera M, Tomasello A, Coscojuela P, et al. Age-adjusted infarct volume threshold for good outcome after endovascular treatment. J Neurointerv Surg. 2014; 6:418–422. PMID: 23832414.
Article20. Hwang YH, Kang DH, Kim YW, Kim YS, Park SP, Suh CK. Outcome of forced-suction thrombectomy in acute intracranial internal carotid occlusion. J Neurointerv Surg. 2013; 5(Suppl 1):i81–i84. PMID: 22544821.
Article21. Kang DH, Hwang YH, Kim YS, Park J, Kwon O, Jung C. Direct thrombus retrieval using the reperfusion catheter of the penumbra system: forced-suction thrombectomy in acute ischemic stroke. AJNR Am J Neuroradiol. 2011; 32:283–287. PMID: 21087940.
Article22. Kang DH, Kim YW, Hwang YH, Park J, Hwang JH, Kim YS. Switching strategy for mechanical thrombectomy of acute large vessel occlusion in the anterior circulation. Stroke. 2013; 44:3577–3579. PMID: 24021683.
Article23. Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003; 34:e109–e137. PMID: 12869717.
Article24. Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, et al. Second European-Australasian Acute Stroke Study Investigators. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Lancet. 1998; 352:1245–1251. PMID: 9788453.
Article25. Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet. 2012; 380:1241–1249. PMID: 22932715.
Article26. Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet. 2000; 355:1670–1674. PMID: 10905241.27. van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988; 19:604–607. PMID: 3363593.
Article28. Sharma JC, Fletcher S, Vassallo M. Strokes in the elderly-higher acute and 3-month mortality-an explanation. Cerebrovasc Dis. 1999; 9:2–9.29. Chandra RV, Leslie-Mazwi TM, Mehta BP, Yoo AJ, Simonsen CZ. Clinical outcome after intra-arterial stroke therapy in the very elderly: why is it so heterogeneous? Front Neurol. 2014; 5:60. PMID: 24808887.
Article30. Arsava EM, Vural A, Akpinar E, Gocmen R, Akcalar S, Oguz KK, et al. The detrimental effect of aging on leptomeningeal collaterals in ischemic stroke. J Stroke Cerebrovasc Dis. 2014; 23:421–426. PMID: 23583014.
Article31. McTaggart RA, Jovin TG, Lansberg MG, Mlynash M, Jayaraman MV, Choudhri OA, et al. Alberta stroke program early computed tomographic scoring performance in a series of patients undergoing computed tomography and MRI: reader agreement, modality agreement, and outcome prediction. Stroke. 2015; 46:407–412. PMID: 25538199.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Guideline for intra-arterial thrombolysis of hyperacute ischemic stroke patients: Preliminary Report
- Intravenous Versus Intra-arterial Thrombolysis for Acute Ischemic Stroke Secondary to Basilar Artery Occlusion
- Endovascular Mechanical Thrombectomy for Acute Ischemic Stroke: A New Standard of Care
- Reperfusion therapy in acute ischemic stroke
- Endovascular Treatment of Acute Ischemic Stroke