Infect Chemother.
2017 Mar;49(1):78-83. 10.3947/ic.2017.49.1.78.
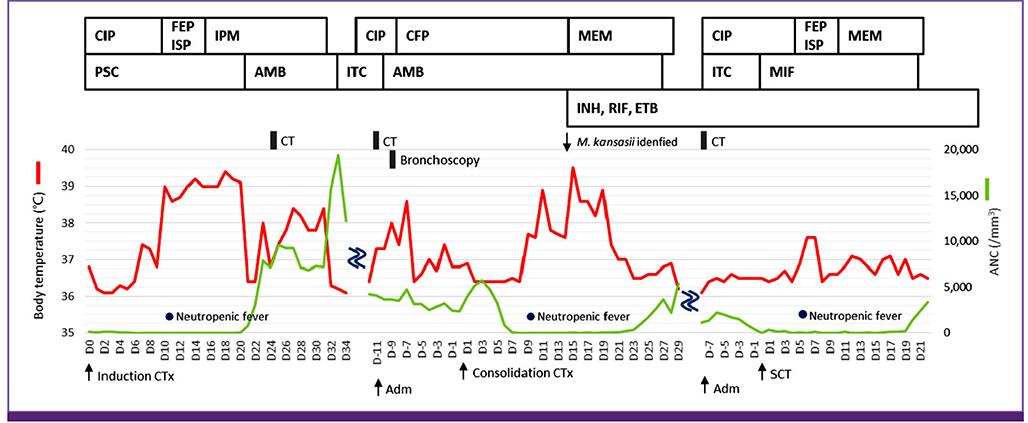
Mycobacterium kansasii Pneumonia with Mediastinal Lymphadenitis in a Patient with Acute Myeloid Leukemia: Successful Treatment to Stem Cell Transplantation
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. cho.sy@catholic.ac.kr
- 2Vaccine Bio Research Institute, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 3The Catholic Blood and Marrow Transplantation Center, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2375104
- DOI: http://doi.org/10.3947/ic.2017.49.1.78
Abstract
- Non-tuberculous mycobacterial (NTM) disease is a relatively rare cause of neutropenic fever in patients with hematologic malignancies. During the neutropenic period, performing invasive procedures for microbiological or pathological confirmation is difficult. In addition, the optimal treatment duration for NTM disease in patients with leukemia, especially prior to stem cell transplantation (SCT), has not been documented. Therefore, we report a case of pneumonia with necrotizing lymphadenitis caused by Mycobacterium kansasii diagnosed during chemotherapy being performed for acute myeloid leukemia. The radiologic findings were similar to those of invasive fungal pneumonia; however, a bronchoalveolar washing fluid culture confirmed that the pathogen was M. kansasii. After 70 days from starting NTM treatment, allogeneic SCT was performed without any complications. The patient fully recovered after 12 months of NTM treatment, and neither reactivation of M. kansasii infection nor related complications were reported.
Keyword
MeSH Terms
Figure
Reference
-
1. Anonymous . Diagnosis and treatment of disease caused by nontuberculous mycobacteria. This official statement of the American Thoracic Society was approved by the Board of Directors, March 1997. Medical Section of the American Lung Association. Am J Respir Crit Care Med. 1997; 156:S1–S25.2. Holland SM. Nontuberculous mycobacteria. Am J Med Sci. 2001; 321:49–55.
Article3. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, Holland SM, Horsburgh R, Huitt G, Iademarco MF, Iseman M, Olivier K, Ruoss S, von Reyn CF, Wallace RJ Jr, Winthrop K; ATS Mycobacterial Diseases Subcommittee. American Thoracic Society; Infectious Disease Society of America. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007; 175:367–416.
Article4. O'Brien RJ. The epidemiology of nontuberculous mycobacterial disease. Clin Chest Med. 1989; 10:407–418.5. Koh WJ, Kwon OJ, Jeon K, Kim TS, Lee KS, Park YK, Bai GH. Clinical significance of nontuberculous mycobacteria isolated from respiratory specimens in Korea. Chest. 2006; 129:341–348.
Article6. Park HK, Koh WJ, Shim TS, Kwon OJ. Clinical characteristics and treatment outcomes of Mycobacterium kansasii lung disease in Korea. Yonsei Med J. 2010; 51:552–556.
Article7. Shitrit D, Baum GL, Priess R, Lavy A, Shitrit AB, Raz M, Shlomi D, Daniele B, Kramer MR. Pulmonary Mycobacterium kansasii infection in Israel, 1999-2004: clinical features, drug susceptibility, and outcome. Chest. 2006; 129:771–776.
Article8. Lee DG, Kim SH, Kim SY, Kim CJ, Min CK, Park WB, Park YJ, Song YG, Jang JS, Jang JH, Jin JY, Choi JH. Evidence-based guidelines for empirical therapy of neutropenic fever in Korea. Infect Chemother. 2011; 43:258–321.
Article9. De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, Pappas PG, Maertens J, Lortholary O, Kauffman CA, Denning DW, Patterson TF, Maschmeyer G, Bille J, Dismukes WE, Herbrecht R, Hope WW, Kibbler CC, Kullberg BJ, Marr KA, Muñoz P, Odds FC, Perfect JR, Restrepo A, Ruhnke M, Segal BH, Sobel JD, Sorrell TC, Viscoli C, Wingard JR, Zaoutis T, Bennett JE; European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group. National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008; 46:1813–1821.
Article10. Arlotta A, Cefalo MG, Maurizi P, Ruggiero A, Dodi I, Riccardi R. Critical pulmonary infection due to nontuberculous mycobacterium in pediatric leukemia: report of a difficult diagnosis and review of pediatric series. J Pediatr Hematol Oncol. 2014; 36:66–70.
Article11. Shitrit D, Priess R, Peled N, Bishara G, Shlomi D, Kramer MR. Differentiation of Mycobacterium kansasii infection from Mycobacterium tuberculosis infection: comparison of clinical features, radiological appearance, and outcome. Eur J Clin Microbiol Infect Dis. 2007; 26:679–684.
Article12. Park SY, Lee GR, Min JW, Jung JY, Jeon YD, Shin HS, Chin BS. A case of Mycobacterium kansasii lymphadenitis in HIV-infected patient. Infect Chemother. 2012; 44:526–529.
Article13. Goldschmidt N, Nusair S, Gural A, Amir G, Izhar U, Laxer U. Disseminated Mycobacterium kansasii infection with pulmonary alveolar proteinosis in a patient with chronic myelogenous leukemia. Am J Hematol. 2003; 74:221–223.
Article14. Tempero MA, Smith PW. Disseminated Mycobacterium kansasii presenting with skin lesions in a patient with chronic lymphocytic leukemia. Med Pediatr Oncol. 1981; 9:283–288.
Article15. Lyons J, Vandenberghe E, Fahy R, McDonnell C, Keane J, McLaughlin AM. An unusual lung mass post stem cell transplantation. Transpl Infect Dis. 2014; 16:672–675.
Article16. Chou YH, Hsu MS, Sheng WH, Chang SC. Disseminated Mycobacterium kansasii infection associated with hemophagocytic syndrome. Int J Infect Dis. 2010; 14:e262–e264.17. Eom KS, Lee DG, Lee HJ, Cho SY, Choi SM, Choi JK, Kim YJ, Lee S, Kim HJ, Cho SG, Lee JW. Tuberculosis before hematopoietic stem cell transplantation in patients with hematologic diseases: report of a single-center experience. Transpl Infect Dis. 2015; 17:73–79.
Article18. Zellweger JP, Sotgiu G, Block M, Dore S, Altet N, Blunschi R, Bogyi M, Bothamley G, Bothe C, Codecasa L, Costa P, Dominguez J, Duarte R, Fløe A, Fresard I, García-García JM, Goletti D, Halm P, Hellwig D, Henninger E, Heykes-Uden H, Horn L, Kruczak K, Latorre I, Pache G, Rath H, Ringshausen FC, Ruiz AS, Solovic I, Souza-Galvão ML, Widmer U, Witte P, Lange C. TBNET. Risk assessment of tuberculosis in contacts by IFN-gamma release assays. A tuberculosis network European trials group study. Am J Respir Crit Care Med. 2015; 191:1176–1184.
Article19. Lee J, Lee SY, Yoo SS, Cha SI, Won DI, Park JY, Lee WK, Kim CH. Clinical value of whole-blood interferon-gamma assay in patients with suspected pulmonary tuberculosis and AFB smear- and polymerase chain reaction-negative bronchial aspirates. Diagn Microbiol Infect Dis. 2012; 73:252–256.
Article20. Finch CK, Chrisman CR, Baciewicz AM, Self TH. Rifampin and rifabutin drug interactions: an update. Arch Intern Med. 2002; 162:985–992.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Four cases of chloroma treated with hematopoietic stem cell transplantation
- A Case Report of the Second de Novo Acute Myeloid Leukemia (AML) Following Allogeneic Stem Cell Transplantation in a Patient with the First AML
- The impact of COVID-19 on acute myeloid leukemia patients undergoing allogeneic stem cell transplantation: a concise review
- Endobronchial Relapse of Acute Myeloid Leukemia after Allogeneic Stem Cell Transplantation
- A Case of Double-unit Cord Blood Transplantation in Primary Refractory Acute Myeloid Leukemia