Clin Orthop Surg.
2016 Sep;8(3):254-261. 10.4055/cios.2016.8.3.254.
Are Western Knee Designs Dimensionally Correct for Korean Women? A Morphometric Study of Resected Femoral Surfaces during Primary Total Knee Arthroplasty
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul NOW Hospital, Anyang, Korea. orthokim1@naver.com
- 2Orthopaedic Research Laboratories, Cleveland, OH, USA.
- 3Department of Orthopedic Surgery, Seoul NOW Hospital, Seongnam, Korea.
- KMID: 2374270
- DOI: http://doi.org/10.4055/cios.2016.8.3.254
Abstract
- BACKGROUND
The purpose of this study was to determine the shape of the distal femur of Korean women compared with the prostheses currently available in Korea.
METHODS
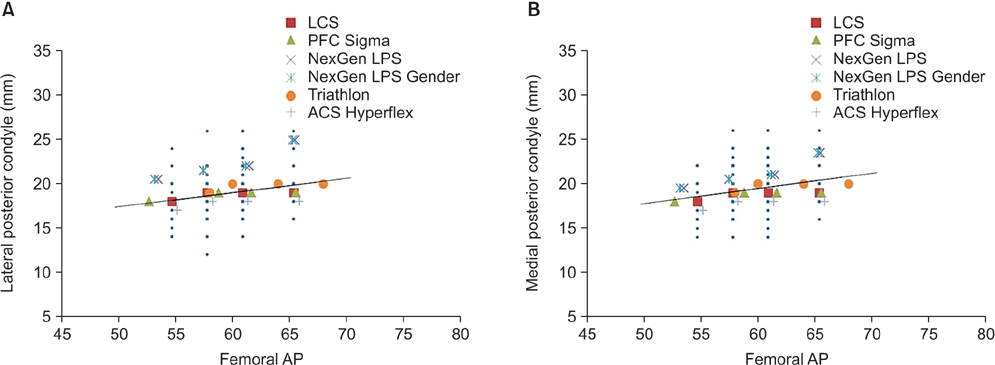
Morphometric data (5 parameters) were measured in 356 resected femurs of Korean women undergoing primary total knee arthroplasty (TKA) utilizing the LCS knee implant (DePuy). The data were then compared with 5 additional contemporary TKA implant systems.
RESULTS
Implant designs based on Caucasian population data do not ideally match the distal femoral morphology of Korean women. Overhang at the anterior mediolateral width was observed in 84.8% for the LCS while a gender-specific implant resulted in undercoverage of the bone in 86%. Posterior overhang was observed in up to 51.2%. Most implant designs have a narrower intercondylar notch than the morphologic data of Korean women.
CONCLUSIONS
Since there is some difference between the shape of distal femur of Korean women and that of the implants, surgeons should have this in mind when selecting an implant for a patient. These data may also be used as a guideline for future prosthetic design options for Korean women population.
Keyword
MeSH Terms
Figure
Reference
-
1. Dickstein R, Heffes Y, Shabtai EI, Markowitz E. Total knee arthroplasty in the elderly: patients' self-appraisal 6 and 12 months postoperatively. Gerontology. 1998; 44(4):204–210.
Article2. Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006; 452:35–43.
Article3. Barrett WP. The need for gender-specific prostheses in TKA: does size make a difference? Orthopedics. 2006; 29:9 Suppl. S53–S55.4. Rostlund T, Carlsson L, Albrektsson B, Albrektsson T. Morphometrical studies of human femoral condyles. J Biomed Eng. 1989; 11(6):442–448.
Article5. Chin KR, Dalury DF, Zurakowski D, Scott RD. Intraoperative measurements of male and female distal femurs during primary total knee arthroplasty. J Knee Surg. 2002; 15(4):213–217.6. Hitt K, Shurman JR 2nd, Greene K, et al. Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg Am. 2003; 85:Suppl 4. 115–122.7. Vaidya SV, Ranawat CS, Aroojis A, Laud NS. Anthropometric measurements to design total knee prostheses for the Indian population. J Arthroplasty. 2000; 15(1):79–85.8. Urabe K, Miura H, Kuwano T, et al. Comparison between the shape of resected femoral sections and femoral prostheses used in total knee arthroplasty in Japanese patients: simulation using three-dimensional computed tomography. J Knee Surg. 2003; 16(1):27–33.9. Ho WP, Cheng CK, Liau JJ. Morphometrical measurements of resected surface of femurs in Chinese knees: correlation to the sizing of current femoral implants. Knee. 2006; 13(1):12–14.10. Cheng FB, Ji XF, Lai Y, et al. Three dimensional morphometry of the knee to design the total knee arthroplasty for Chinese population. Knee. 2009; 16(5):341–347.11. Chaichankul C, Tanavalee A, Itiravivong P. Anthropometric measurements of knee joints in Thai population: correlation to the sizing of current knee prostheses. Knee. 2011; 18(1):5–10.
Article12. Cheng FB, Ji XF, Zheng WX, et al. Use of anthropometric data from the medial tibial and femoral condyles to design unicondylar knee prostheses in the Chinese population. Knee Surg Sports Traumatol Arthrosc. 2010; 18(3):352–358.
Article13. Lim HC, Bae JH, Yoon JY, Kim SJ, Kim JG, Lee JM. Gender differences of the morphology of the distal femur and proximal tibia in a Korean population. Knee. 2013; 20(1):26–30.
Article14. Chin PL, Tey TT, Ibrahim MY, Chia SL, Yeo SJ, Lo NN. Intraoperative morphometric study of gender differences in Asian femurs. J Arthroplasty. 2011; 26(7):984–988.
Article15. Dorr LD, Boiardo RA. Technical considerations in total knee arthroplasty. Clin Orthop Relat Res. 1986; (205):5–11.
Article16. Matsuda S, Matsuda H, Miyagi T, Sasaki K, Iwamoto Y, Miura H. Femoral condyle geometry in the normal and varus knee. Clin Orthop Relat Res. 1998; (349):183–188.
Article17. Matsuda S, Miura H, Nagamine R, et al. Anatomical analysis of the femoral condyle in normal and osteoarthritic knees. J Orthop Res. 2004; 22(1):104–109.
Article18. Guy SP, Farndon MA, Sidhom S, Al-Lami M, Bennett C, London NJ. Gender differences in distal femoral morphology and the role of gender specific implants in total knee replacement: a prospective clinical study. Knee. 2012; 19(1):28–31.
Article19. Mahoney OM, Kinsey T. Overhang of the femoral component in total knee arthroplasty: risk factors and clinical consequences. J Bone Joint Surg Am. 2010; 92(5):1115–1121.
Article20. Kim YH, Choi Y, Kim JS. Comparison of a standard and a gender-specific posterior cruciate-substituting high-flexion knee prosthesis: a prospective, randomized, short-term outcome study. J Bone Joint Surg Am. 2010; 92(10):1911–1920.
Article21. Kim YH, Choi Y, Kim JS. Comparison of standard and gender-specific posterior-cruciate-retaining high-flexion total knee replacements: a prospective, randomised study. J Bone Joint Surg Br. 2010; 92(5):639–645.22. Greene KA. Gender-specific design in total knee arthroplasty. J Arthroplasty. 2007; 22:7 Suppl 3. 27–31.
Article23. Bellemans J, Carpentier K, Vandenneucker H, Vanlauwe J, Victor J. The John Insall Award: both morphotype and gender influence the shape of the knee in patients undergoing TKA. Clin Orthop Relat Res. 2010; 468(1):29–36.
Article24. Harwin SF, Greene KA, Hitt K. Early experience with a new total knee implant: maximizing range of motion and function with gender-specific sizing. Surg Technol Int. 2007; 16:199–205.25. Choi YJ, Kang JH, Lee KW, Joo YS, Park JS, Choo HH. Early aseptic loosening after total knee replacement using legacy posterior stabilized-flex prosthesis. J Korean Orthop Assoc. 2012; 47(1):35–40.
Article26. King TV, Scott RD. Femoral component loosening in total knee arthroplasty. Clin Orthop Relat Res. 1985; (194):285–290.
Article27. Zelle J, Janssen D, Van Eijden J, De Waal Malefijt M, Verdonschot N. Does high-flexion total knee arthroplasty promote early loosening of the femoral component? J Orthop Res. 2011; 29(7):976–983.
Article28. Barnes CL, Scott RD. Popliteus tendon dysfunction following total knee arthroplasty. J Arthroplasty. 1995; 10(4):543–545.
Article29. Ryu J, Saito S, Yamamoto K, Sano S. Factors influencing the postoperative range of motion in total knee arthroplasty. Bull Hosp Jt Dis. 1993; 53(3):35–40.30. Mihalko W, Fishkin Z, Krackow K. Patellofemoral overstuff and its relationship to flexion after total knee arthroplasty. Clin Orthop Relat Res. 2006; 449:283–287.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Arterial Occlusion Following Primary Total Knee Arthroplasty
- Synovial Impingement after Total Knee Replacement Arthroplasty: A Case Report
- Repeated Periprosthethic Femoral Fracture in a Below Knee Amputee with Ipsilateral Cementless Total Hip Arthroplasty: A Case Report
- Is it useful to Get an Expected Tibio - femoral Angle using Overcorrection Method in Total Knee Arthroplasty?: Preliminary Report
- Resected femoral anthropometry for design of the femoral component of the total knee prosthesis in a Korean population