Yonsei Med J.
2017 Jan;58(1):158-164. 10.3349/ymj.2017.58.1.158.
Dose-Response Relationship between Alanine Aminotransferase Levels within the Reference Interval and Metabolic Syndrome in Chinese Adults
- Affiliations
-
- 1Department of Epidemiology, School of Public Health, Shandong University, Jinan, China. wshm@sdu.edu.cn
- 2Department of Prevention and Health Care, Dongying Shengli Oilfield Central Hospital, Dongying, China.
- 3Department of Nutrition and Food Safety, Zhejiang Center for Disease Control and Prevention, Hangzhou, China.
- 4Tianjin Entry-Exit Inspection and Quarantine Bureau, Tianjin, China.
- 5Department of Medical Records and Statistics, Zhejiang Hospital, Hangzhou, China.
- KMID: 2374202
- DOI: http://doi.org/10.3349/ymj.2017.58.1.158
Abstract
- PURPOSE
Elevation in serum alanine aminotransferase (ALT) levels is a biomarker for metabolic syndrome (MS); however, the relationship has not been fully investigated within the reference interval of ALT levels. Our objective was to explore the relationship between serum ALT levels within the reference interval and MS in Chinese adults.
MATERIALS AND METHODS
This cross-sectional study included 16028 adults, who attended routine health check-ups at Shengli Oilfield Central Hospital from January 2006 to March 2012. The reference interval of serum ALT level was defined as less than 40 U/L. Logistic regression models and restricted cubic spline were used to evaluate the association of ALT with MS.
RESULTS
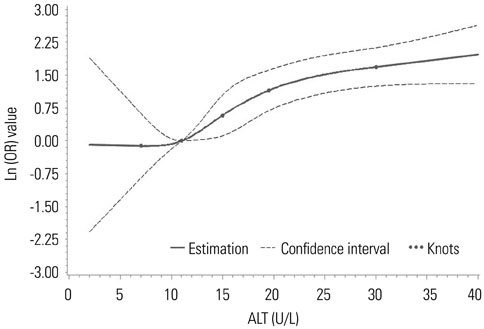
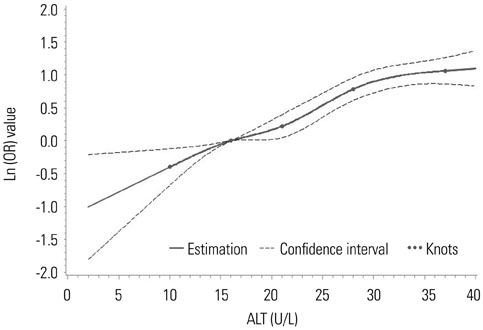
The prevalence of MS in the total population was 13.7% (6.4% for females and 18.4% for males). Multiple logistic regression showed that ALT levels were positively associated with MS after adjustment for potential confounding factors. The odds ratio of MS in the top quartile was 4.830 [95% confidence interval (CI): 2.980-7.829] in females and 3.168 (95% CI: 2.649-3.790) in males, compared with the ALT levels in the bottom quartile. The restricted cubic spline models revealed a positive non-linear dose-response relationship between ALT levels and the risk of MS in women (p for nonlinearity was 0.0327), but a positive linear dose-response relationship in men (p for nonlinearity was 0.0659).
CONCLUSION
Serum ALT levels within the reference interval are positively associated with MS in a dose-response manner. Elevated ALT levels, even within the reference interval, may reflect early dysmetabolic changes.
MeSH Terms
-
Adult
Aged
Alanine Transaminase/*blood
Asian Continental Ancestry Group
Biomarkers/blood
Confidence Intervals
Cross-Sectional Studies
Dose-Response Relationship, Drug
Female
Humans
Logistic Models
Male
Metabolic Syndrome X/*enzymology/epidemiology
Middle Aged
Odds Ratio
Prevalence
Reference Values
Alanine Transaminase
Biomarkers
Figure
Reference
-
1. Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009; 120:1640–1645.2. Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010; 56:1113–1132.3. Khang YH, Cho SI, Kim HR. Risks for cardiovascular disease, stroke, ischaemic heart disease, and diabetes mellitus associated with the metabolic syndrome using the new harmonised definition: findings from nationally representative longitudinal data from an Asian population. Atherosclerosis. 2010; 213:579–585.
Article4. Mozumdar A, Liguori G. Persistent increase of prevalence of metabolic syndrome among US adults: NHANES III to NHANES 1999-2006. Diabetes Care. 2011; 34:216–219.
Article5. Xi B, He D, Hu Y, Zhou D. Prevalence of metabolic syndrome and its influencing factors among the Chinese adults: the China Health and Nutrition Survey in 2009. Prev Med. 2013; 57:867–871.
Article6. Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010; 38:105–113.7. James PT. Obesity: the worldwide epidemic. Clin Dermatol. 2004; 22:276–280.
Article8. Schindhelm RK, Diamant M, Dekker JM, Tushuizen ME, Teerlink T, Heine RJ. Alanine aminotransferase as a marker of non-alcoholic fatty liver disease in relation to type 2 diabetes mellitus and cardiovascular disease. Diabetes Metab Res Rev. 2006; 22:437–443.
Article9. Goessling W, Massaro JM, Vasan RS, D’Agostino RB Sr, Ellison RC, Fox CS. Aminotransferase levels and 20-year risk of metabolic syndrome, diabetes, and cardiovascular disease. Gastroenterology. 2008; 135:1935–1944. 1944.e1
Article10. Janičko M, Veselìny E, Orenčák R, Husťak R, Fedačko J, Dražilová S, et al. Redefining the alanine aminotransferase upper limit of normal improves the prediction of metabolic syndrome risk. Eur J Gastroenterol Hepatol. 2015; 27:405–411.
Article11. Kim HC, Choi KS, Jang YH, Shin HW, Kim DJ. Normal serum aminotransferase levels and the metabolic syndrome: Korean National Health and Nutrition Examination Surveys. Yonsei Med J. 2006; 47:542–550.
Article12. Suh SY, Choi SE, Ahn HY, Yang HM, Kim YI, Sung NJ. The association between normal alanine aminotransferase levels and the metabolic syndrome: 2005 Korean National Health and Nutrition Examination Survey. Metabolism. 2009; 58:1731–1736.
Article13. Steinvil A, Shapira I, Ben-Bassat OK, Cohen M, Vered Y, Berliner S, et al. The association of higher levels of within-normal-limits liver enzymes and the prevalence of the metabolic syndrome. Cardiovasc Diabetol. 2010; 9:30.
Article14. Bethel MA, Deedwania P, Levitt NS, Schmitz O, Huntsman-Labed A, Califf RM, et al. Metabolic syndrome and alanine aminotransferase: a global perspective from the NAVIGATOR screening population. Diabet Med. 2009; 26:1204–1211.
Article15. Liu Z, Que S, Ning H, Wang L, Peng T. Elevated alanine aminotransferase is strongly associated with incident metabolic syndrome: a meta-analysis of prospective studies. PLoS One. 2013; 8:e80596.
Article16. WHO. Guidelines for controlling and monitoring the tobacco epidemic. Geneva: World Health Organization;1998.17. Ma G, Zhu D, Hu X, Luan D, Kong L, Yang X. [The drinking practice of people in China]. Acta Nutrimenta Sinica. 2005; 27:362–365.18. Wang X, Yang F, Bots ML, Guo WY, Zhao B, Hoes AW, et al. Prevalence of the metabolic syndrome among employees in Northeast China. Chin Med J. 2015; 128:1989–1993.
Article19. Desquilbet L, Mariotti F. Dose-response analyses using restricted cubic spline functions in public health research. Stat Med. 2010; 29:1037–1057.
Article20. Polotsky HN, Polotsky AJ. Metabolic implications of menopause. Semin Reprod Med. 2010; 28:426–434.
Article21. Murphy MJ, Metcalf BS, Voss LD, Jeffery AN, Kirkby J, Mallam KM, et al. Girls at five are intrinsically more insulin resistant than boys: The Programming Hypotheses Revisited--The EarlyBird Study (EarlyBird 6). Pediatrics. 2004; 113(1 Pt 1):82–86.
Article22. Ehm MG, Karnoub MC, Sakul H, Gottschalk K, Holt DC, Weber JL, et al. Genomewide search for type 2 diabetes susceptibility genes in four American populations. Am J Hum Genet. 2000; 66:1871–1881.
Article23. Clark JM, Brancati FL, Diehl AM. The prevalence and etiology of elevated aminotransferase levels in the United States. Am J Gastroenterol. 2003; 98:960–967.
Article24. Tarantino G, Finelli C. What about non-alcoholic fatty liver disease as a new criterion to define metabolic syndrome? World J Gastroenterol. 2013; 19:3375–3384.
Article25. Gariani K, Philippe J, Jornayvaz FR. Non-alcoholic fatty liver disease and insulin resistance: from bench to bedside. Diabetes Metab. 2013; 39:16–26.
Article26. Sookoian S, Pirola CJ. Alanine and aspartate aminotransferase and glutamine-cycling pathway: their roles in pathogenesis of metabolic syndrome. World J Gastroenterol. 2012; 18:3775–3781.
Article27. Hanley AJ, Wagenknecht LE, Festa A, D’Agostino RB Jr, Haffner SM. Alanine aminotransferase and directly measured insulin sensitivity in a multiethnic cohort: the Insulin Resistance Atherosclerosis Study. Diabetes Care. 2007; 30:1819–1827.
Article28. Yamada J, Tomiyama H, Yambe M, Koji Y, Motobe K, Shiina K, et al. Elevated serum levels of alanine aminotransferase and gamma glutamyltransferase are markers of inflammation and oxidative stress independent of the metabolic syndrome. Atherosclerosis. 2006; 189:198–205.
Article29. Lee SH, Kim KN, Kim KM, Joo NS. Irritable bowel syndrome may be associated with elevated alanine aminotransferase and metabolic syndrome. Yonsei Med J. 2016; 57:146–152.
Article30. Harrison SA. HCV therapy in 2006: down with ALT levels, in with awareness of co-existent metabolic syndrome. J Hepatol. 2006; 44:624–626.
Article31. Wu WC, Wu CY, Wang YJ, Hung HH, Yang HI, Kao WY, et al. Updated thresholds for serum alanine aminotransferase level in a large-scale population study composed of 34 346 subjects. Aliment Pharmacol Ther. 2012; 36:560–568.
Article32. Prati D, Taioli E, Zanella A, Della Torre E, Butelli S, Del Vecchio E, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med. 2002; 137:1–10.
Article33. Kunde SS, Lazenby AJ, Clements RH, Abrams GA. Spectrum of NAFLD and diagnostic implications of the proposed new normal range for serum ALT in obese women. Hepatology. 2005; 42:650–656.
Article34. Wei D, Chen T, Li J, Gao Y, Ren Y, Zhang X, et al. Association of serum gamma-glutamyl transferase and ferritin with the metabolic syndrome. J Diabetes Res. 2015; 2015:741731.
Article35. Lu YH, Lu JM, Wang SY, Li CL, Liu LS, Zheng RP, et al. [Comparison of the diagnostic criteria of metabolic syndrome by International Diabetes Federation and that by Chinese Medical Association Diabetes Branch]. Zhonghua Yi Xue Za Zhi. 2006; 86:386–389.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Metabolic Syndrome and Serum Alanine Aminotransferase Levels in Korean Adults : The Third Korea National Health and Nutrition Examination Survey (KNHANES III), 2005
- Relationship between Elevated Serum Alanine Aminotransferase Concentration and Metabolic Syndrome in Korean Adults
- Liver function tests as indicators of metabolic syndrome
- Association of serum alanine aminotransferase and gamma-glutamyltransferase levels within the reference range with metabolic syndrome and nonalcoholic fatty liver disease
- Normal Serum Aminotransferase Levels and the Metabolic Syndrome: Korean National Health and Nutrition Examination Surveys