Yonsei Med J.
2017 Jan;58(1):105-113. 10.3349/ymj.2017.58.1.105.
Efficacy and Safety of Intravenous Urapidil for Older Hypertensive Patients with Acute Heart Failure: A Multicenter Randomized Controlled Trial
- Affiliations
-
- 1Department of Geriatrics, Xuanwu Hospital, Capital Medical University, Beijing, China.
- 2Department of Cardiology, An Zhen Hospital affiliated with Capital Medical University, Beijing, China.
- 3Fu Yan Emergency Department, Tong Ren Hospital affiliated with Capital Medical University, Beijing, China.
- 4Department of Cardiology, Xuanwu Hospital, Capital Medical University, Beijing, China. huaqi5371@medmail.com.cn
- 5Department of Cardiology, First Hospital affiliated with Chongqing University, Chongqing, China.
- 6Department of Cardiology, Ningbo First Hospital, Ningbo, China.
- 7Department of Cardiology, Luhe Hospital of Beijing Tongzhou District, Beijing, China.
- 8Department of Cardiology, Mentougou District Hospital of Beijing City, Beijing, China.
- 9Emergency Department, First Hospital affiliated with Sun Yat-sen University, Guangzhou, China.
- 10Emergency Department, Xuanwu Hospital, Capital Medical University, Beijing, China.
- KMID: 2374195
- DOI: http://doi.org/10.3349/ymj.2017.58.1.105
Abstract
- PURPOSE
Urapidil is putatively effective for patients with hypertension and acute heart failure, although randomized controlled trials thereon are lacking. We investigated the efficacy and safety of intravenous urapidil relative to that of nitroglycerin in older patients with hypertension and heart failure in a randomized controlled trial.
MATERIALS AND METHODS
Patients (>60 y) with hypertension and heart failure were randomly assigned to receive intravenous urapidil (n=89) or nitroglycerin (n=91) for 7 days. Hemodynamic parameters, cardiac function, and safety outcomes were compared.
RESULTS
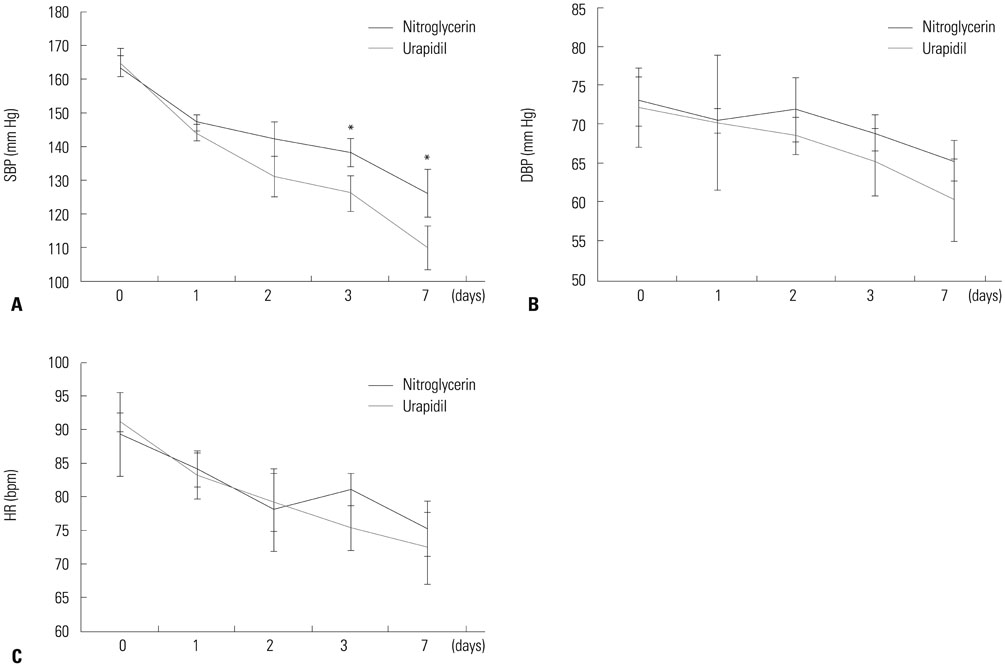
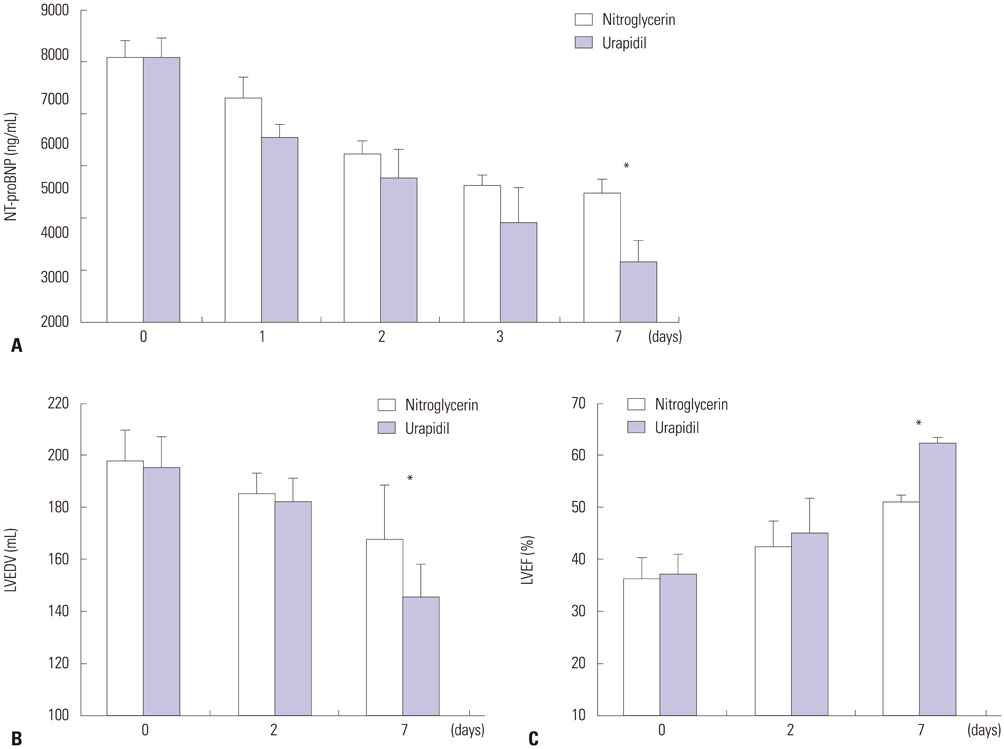
Patients in the urapidil group had significantly lower mean systolic blood pressure (110.1±6.5 mm Hg) than those given nitroglycerin (126.4±8.1 mm Hg, p=0.022), without changes in heart rate. Urapidil was associated with improved cardiac function as reflected by lower N terminal-pro B type natriuretic peptide after 7 days (3311.4±546.1 ng/mL vs. 4879.1±325.7 ng/mL, p=0.027) and improved left ventricular ejection fraction (62.2±3.4% vs. 51.0±2.4%, p=0.032). Patients given urapidil had fewer associated adverse events, specifically headache (p=0.025) and tachycardia (p=0.004). The one-month rehospitalization and all-cause mortality rates were similar.
CONCLUSION
Intravenous administration of urapidil, compared with nitroglycerin, was associated with better control of blood pressure and preserved cardiac function, as well as fewer adverse events, for elderly patients with hypertension and acute heart failure.
MeSH Terms
-
Acute Disease
Aged
Antihypertensive Agents/*administration & dosage
Blood Pressure/drug effects
Cause of Death
Female
Heart Failure/*drug therapy/physiopathology
Heart Rate/drug effects/physiology
Hemodynamics
Humans
Hypertension/*drug therapy/physiopathology
Injections, Intravenous
Male
Middle Aged
Natriuretic Peptide, Brain/blood
Nitroglycerin/administration & dosage
Peptide Fragments/blood
Piperazines/*administration & dosage
Ventricular Function, Left/drug effects/physiology
Antihypertensive Agents
Peptide Fragments
Piperazines
Natriuretic Peptide, Brain
Nitroglycerin
Figure
Reference
-
1. McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the european society of cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012; 33:1787–1847.2. Writing committee members, Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013; 128:e240–e327.3. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015; 131:e29–e322.4. Alexander P, Alkhawam L, Curry J, Levy P, Pang PS, Storrow AB, et al. Lack of evidence for intravenous vasodilators in ED patients with acute heart failure: a systematic review. Am J Emerg Med. 2015; 33:133–141.
Article5. Cicci JD, Reed BN, McNeely EB, Oni-Orisan A, Patterson JH, Rodgers JE. Acute decompensated heart failure: evolving literature and implications for future practice. Pharmacotherapy. 2014; 34:373–388.
Article6. Felker GM, Adams KF Jr, Konstam MA, O’Connor CM, Gheorghiade M. The problem of decompensated heart failure: nomenclature, classification, and risk stratification. Am Heart J. 2003; 145:2 Suppl. S18–S25.
Article7. Adams KF Jr, Fonarow GC, Emerman CL, LeJemtel TH, Costanzo MR, Abraham WT, et al. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J. 2005; 149:209–216.
Article8. Zannad F, Mebazaa A, Juillière Y, Cohen-Solal A, Guize L, Alla F, et al. Clinical profile, contemporary management and one-year mortality in patients with severe acute heart failure syndromes: the EFICA study. Eur J Heart Fail. 2006; 8:697–705.
Article9. Piper S, McDonagh T. The role of intravenous vasodilators in acute heart failure management. Eur J Heart Fail. 2014; 16:827–834.
Article10. Levy PD, Laribi S, Mebazaa A. Vasodilators in acute heart failure: review of the latest studies. Curr Emerg Hosp Med Rep. 2014; 2:126–132.
Article11. Cherney D, Straus S. Management of patients with hypertensive urgencies and emergencies: a systematic review of the literature. J Gen Intern Med. 2002; 17:937–945.
Article12. Elkayam U, Bitar F, Akhter MW, Khan S, Patrus S, Derakhshani M. Intravenous nitroglycerin in the treatment of decompensated heart failure: potential benefits and limitations. J Cardiovasc Pharmacol Ther. 2004; 9:227–241.
Article13. den Uil CA, Brugts JJ. Impact of intravenous nitroglycerin in the management of acute decompensated heart failure. Curr Heart Fail Rep. 2015; 12:87–93.
Article14. Alijotas-Reig J, Bove-Farre I, de Cabo-Frances F, Angles-Coll R. Effectiveness and safety of prehospital urapidil for hypertensive emergencies. Am J Emerg Med. 2001; 19:130–133.
Article15. Buch J. Urapidil, a dual-acting antihypertensive agent: current usage considerations. Adv Ther. 2010; 27:426–443.
Article16. Yang W, Zhou YJ, Fu Y, Qin J, Qin S, Chen XM, et al. A multicenter, randomized, trial comparing urapidil and nitroglycerin in multifactor heart failure in the elderly. Am J Med Sci. 2015; 350:109–115.
Article17. Liu LS. Writing Group of 2010 Chinese Guidelines for the Management of Hypertension. [2010 Chinese guidelines for the management of hypertension]. Zhonghua Xin Xue Guan Bing Za Zhi. 2011; 39:579–615.18. Chinese Society of Cardiology of Chinese Medical Association. Editorial Board of Chinese Journal of Cardiology. [Chinese guidelines for the diagnosis and treatment of heart failure 2014]. Zhonghua Xin Xue Guan Bing Za Zhi. 2014; 42:98–122.19. Carlson MD, Eckman PM. Review of vasodilators in acute decompensated heart failure: the old and the new. J Card Fail. 2013; 19:478–493.
Article20. Mebazaa A, Longrois D, Metra M, Mueller C, Richards AM, Roessig L, et al. Agents with vasodilator properties in acute heart failure: how to design successful trials. Eur J Heart Fail. 2015; 17:652–664.
Article21. Wang RY, Chow JS, Chan KH, Pan HY, Wong RP. Acute haemodynamic and myocardial metabolic effects of intravenous urapidil in severe heart failure. Eur Heart J. 1984; 5:745–751.
Article22. Carlyle PF, Cohn JN. Systemic and regional hemodynamic effects of alpha-adrenoceptor blockade in chronic left ventricular dysfunction in the conscious dog. Am Heart J. 1990; 120:619–624.
Article23. Tebbe U, Wurst W, Neuhaus KL. Acute haemodynamic effects of urapidil in patients with chronic left ventricular failure. Eur J Clin Pharmacol. 1988; 35:305–308.
Article24. Zink M, Gombotz H, Wasler A, Grasser B, Rehak P, Metzler H. Urapidil reduces elevated pulmonary vascular resistance in patients before heart transplantation. J Heart Lung Transplant. 2002; 21:347–353.
Article25. Kozàkovà M, Marco J, Heusch G, Bernies M, Bossi IM, Palombo C, et al. The alpha1-adrenergic blocker urapidil improves contractile function in patients 3 months after coronary stenting: a randomized, double-blinded study. Am Heart J. 2004; 147:E6.26. Yao DK, Jia SQ, Wang L, Li HW, Zhang YC, Wang YL, et al. Therapeutic effect of urapidil on myocardial perfusion in patients with ST-elevation acute coronary syndrome. Eur J Intern Med. 2009; 20:152–157.
Article27. van Veldhuisen DJ, Linssen GC, Jaarsma T, van Gilst WH, Hoes AW, Tijssen JG, et al. B-type natriuretic peptide and prognosis in heart failure patients with preserved and reduced ejection fraction. J Am Coll Cardiol. 2013; 61:1498–1506.
Article28. Jhund PS, Anand IS, Komajda M, Claggett BL, McKelvie RS, Zile MR, et al. Changes in N-terminal pro-B-type natriuretic peptide levels and outcomes in heart failure with preserved ejection fraction: an analysis of the I-Preserve study. Eur J Heart Fail. 2015; 17:809–817.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Urapidil on Changes of Arterial Blood Pressure and Heart Rate to Endotracheal Intubation
- Cardiac Rehabilitation of Heart Failure
- Safety and Effect of Continuous Intravenous Urokinase Therapy in Acute Ischemic Stroke ( Open Clinical Trial )
- Treatment of acute respiratory failure: extracorporeal membrane oxygenation
- Efficacy and safety of rapid intermittent bolus compared with slow continuous infusion in patients with severe hypernatremia (SALSA II trial): a study protocol for a randomized controlled trial