Yonsei Med J.
2017 Jan;58(1):90-98. 10.3349/ymj.2017.58.1.90.
Impact of Diltiazem Alone versus Diltiazem with Nitrate on Five-Year Clinical Outcomes in Patients with Significant Coronary Artery Spasm
- Affiliations
-
- 1Department of Internal Medicine, Weiss Memorial Hospital, Chicago, IL, USA.
- 2Cardiovascular Center, Eulji University Eulji General Hospital, Seoul, Korea.
- 3Cardiovascular Center, Korea University Guro Hospital, Seoul, Korea. swrha617@yahoo.co.kr
- 4KU-KIST Graduate School Converging Science and Technology, Seoul, Korea. mdhsseo@korea.ac.kr
- 5Department of Medicine, Korea University Graduate School, Seoul, Korea.
- 6Cardiology Department, Soonchunhyang University Cheonan Hospital, Cheonan, Korea.
- KMID: 2374193
- DOI: http://doi.org/10.3349/ymj.2017.58.1.90
Abstract
- PURPOSE
Calcium channel blockers diltiazem and nitrate have been used as selective coronary vasodilators for patients with significant coronary artery spasm (CAS). However, no study has compared the efficacy of diltiazem alone versus diltiazem with nitrate for long-term clinical outcomes in patients with CAS.
MATERIALS AND METHODS
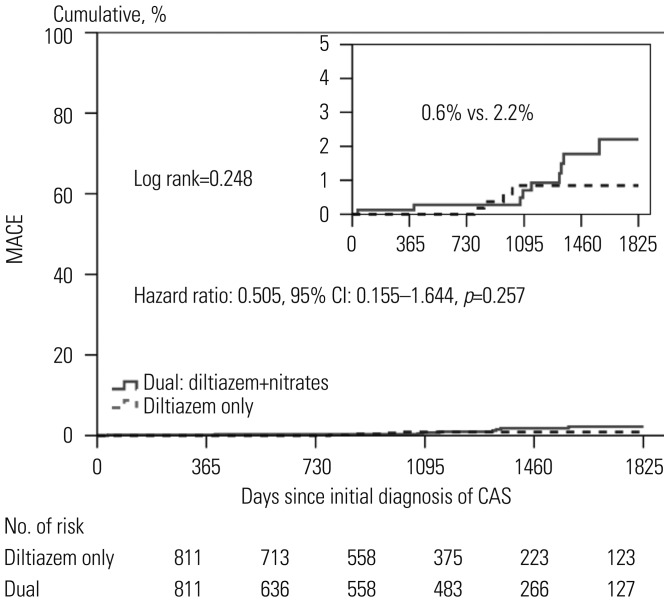
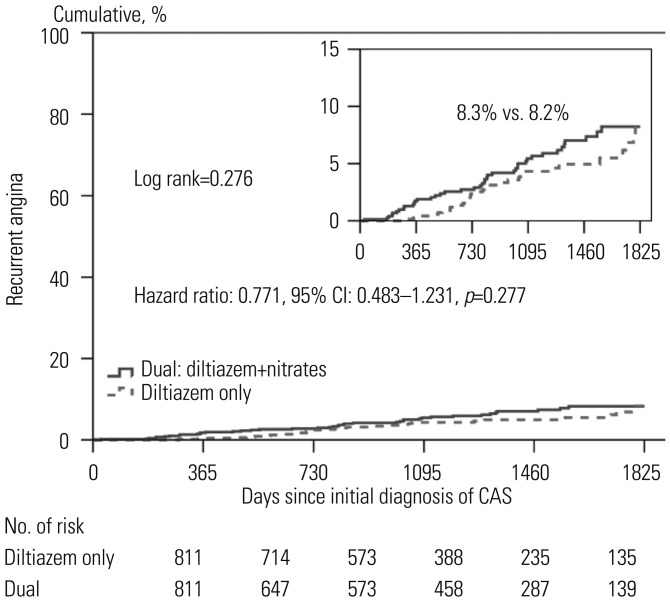
A total of 2741 consecutive patients without significant coronary artery disease with positive CAS by acetylcholine (Ach) provocation test between November 2004 and May 2014 were enrolled. Significant CAS was defined as a narrowing of >70% by incremental intracoronary injection of 20, 50, and 100 µg of Ach into the left coronary artery. Patients were assigned to either the diltiazem group (n=842) or the dual group (diltiazem with nitrate, n=1899) at physician discretion. To adjust for potential confounders, a propensity score matching (PSM) analysis was performed using the logistic regression model. After PSM analysis, two well-balanced groups (811 pairs, n=1622, C-statistic=0.708) were generated.
RESULTS
At 5 years, there were similar incidences in primary endpoints, including mortality, myocardial infarction, revascularization, and recurrent angina requiring repeat coronary angiography between the two groups. Diltiazem alone was not an independent predictor for major adverse cardiovascular events or recurrent angina requiring repeat coronary angiography.
CONCLUSION
Despite the expected improvement of endothelial function and the relief of CAS, the combination of diltiazem and nitrate treatment was not superior to diltiazem alone in reducing mortality and cardiovascular events up to 5 years in patients with significant CAS.
Keyword
MeSH Terms
-
Acetylcholine
Aged
Angina Pectoris/diagnosis
Calcium Channel Blockers/therapeutic use
Cardiovascular Agents/*therapeutic use
Coronary Angiography/adverse effects
Coronary Artery Disease/prevention & control
Coronary Vasospasm/diagnosis/*drug therapy
Diltiazem/*therapeutic use
Drug Therapy, Combination
Female
Humans
Incidence
Male
Middle Aged
Myocardial Infarction/prevention & control
Nitrates/*therapeutic use
Propensity Score
Time Factors
Vasodilator Agents/therapeutic use
Acetylcholine
Calcium Channel Blockers
Cardiovascular Agents
Diltiazem
Nitrates
Vasodilator Agents
Figure
Cited by 1 articles
-
Characteristics of Patients with Vasospastic Angina in Korea: Data from a Large Cohort (VA-KOREA)
Sung Eun Kim, Sang-Ho Jo, Won-Woo Seo, Min-Ho Lee, Hyun-Jin Kim, Seong-Sik Cho, Kwan Yong Lee, Dong-Soo Kim, Tae-Hyun Yang, Sung-Ho Her, Seung Hwan Han, Byoung-Kwon Lee, Youngkeun Ahn, Seung-Woon Rha, Hyeon-Cheol Gwon, Dong-Ju Choi, Sang Hong Baek
Cardiovasc Prev Pharmacother. 2021;3(3):47-53. doi: 10.36011/cpp.2021.3.e8.
Reference
-
1. Yamashina Y, Yagi T, Ishida A, Mibiki Y, Sato H, Nakagawa T, et al. Differentiating between comatose patients resuscitated from acute coronary syndrome-associated and subarachnoid hemorrhage-associated out-of-hospital cardiac arrest. J Cardiol. 2015; 65:508–513. PMID: 25192593.
Article2. Ajani AE, Yan BP. The mystery of coronary artery spasm. Heart Lung Circ. 2007; 16:10–15. PMID: 17196430.
Article3. Tanabe K, Kawai Y, Kitayama M, Akao H, Ishida R, Motoyama A, et al. Increased levels of the oxidative stress marker, nitrotyrosine in patients with provocation test-induced coronary vasospasm. J Cardiol. 2014; 64:86–90. PMID: 24393614.
Article4. Park JY, Rha SW, Li YJ, Chen KY, Choi BG, Choi SY, et al. The impact of high sensitivity C-reactive protein level on coronary artery spasm as assessed by intracoronary acetylcholine provocation test. Yonsei Med J. 2013; 54:1299–1304. PMID: 24142631.
Article5. Park JY, Rha SW, Jin Z, Poddar KL, Ramasamy S, Chen KY, et al. Multivessel versus single vessel spasm, as assessed by the intracoronary acetylcholine provocation test, in Korean patients. Clin Exp Pharmacol Physiol. 2011; 38:819–823. PMID: 21933225.
Article6. Murad F. Shattuck Lecture. Nitric oxide and cyclic GMP in cell signaling and drug development. N Engl J Med. 2006; 355:2003–2011. PMID: 17093251.7. Moncada S, Palmer RM, Higgs EA. Nitric oxide: physiology, pathophysiology, and pharmacology. Pharmacol Rev. 1991; 43:109–142. PMID: 1852778.8. Kugiyama K, Ohgushi M, Sugiyama S, Motoyama T, Kawano H, Hirashima O, et al. Supersensitive dilator response to nitroglycerin but not to atrial natriuretic peptide in spastic coronary arteries in coronary spastic angina. Am J Cardiol. 1997; 79:606–610. PMID: 9068517.
Article9. Boulanger C, Lüscher TF. Release of endothelin from the porcine aorta. Inhibition by endothelium-derived nitric oxide. J Clin Invest. 1990; 85:587–590. PMID: 2153712.
Article10. Takemoto M, Egashira K, Usui M, Numaguchi K, Tomita H, Tsutsui H, et al. Important role of tissue angiotensin-converting enzyme activity in the pathogenesis of coronary vascular and myocardial structural changes induced by long-term blockade of nitric oxide synthesis in rats. J Clin Invest. 1997; 99:278–287. PMID: 9005996.
Article11. Kaneda H, Taguchi J, Kuwada Y, Hangaishi M, Aizawa T, Yamakado M, et al. Coronary artery spasm and the polymorphisms of the endothelial nitric oxide synthase gene. Circ J. 2006; 70:409–413. PMID: 16565556.
Article12. Vanhoutte PM, Shimokawa H. Endothelium-derived relaxing factor and coronary vasospasm. Circulation. 1989; 80:1–9. PMID: 2661051.
Article13. Lanza GA, Careri G, Crea F. Mechanisms of coronary artery spasm. Circulation. 2011; 124:1774–1782. PMID: 22007100.
Article14. Takahashi J, Nihei T, Takagi Y, Miyata S, Odaka Y, Tsunoda R, et al. Prognostic impact of chronic nitrate therapy in patients with vasospastic angina: multicentre registry study of the Japanese coronary spasm association. Eur Heart J. 2015; 36:228–237. PMID: 25189599.
Article15. Pristipino C, Beltrame JF, Finocchiaro ML, Hattori R, Fujita M, Mongiardo R, et al. Major racial differences in coronary constrictor response between japanese and caucasians with recent myocardial infarction. Circulation. 2000; 101:1102–1108. PMID: 10715255.
Article16. Kimura E, Kishida H. Treatment of variant angina with drugs: a survey of 11 cardiology institutes in Japan. Circulation. 1981; 63:844–848. PMID: 6110492.
Article17. Choi BG, Park SH, Rha SW, Park JY, Choi SY, Park Y, et al. Five-year clinical outcomes in patients with significant coronary artery spasm: a propensity score-matched analysis. Int J Cardiol. 2015; 184:533–539. PMID: 25767010.
Article18. Ong P, Athanasiadis A, Sechtem U. Patterns of coronary vasomotor responses to intracoronary acetylcholine provocation. Heart. 2013; 99:1288–1295. PMID: 23442537.
Article19. Ong P, Athanasiadis A, Borgulya G, Vokshi I, Bastiaenen R, Kubik S, et al. Clinical usefulness, angiographic characteristics, and safety evaluation of intracoronary acetylcholine provocation testing among 921 consecutive white patients with unobstructed coronary arteries. Circulation. 2014; 129:1723–1730. PMID: 24573349.
Article20. Ong P, Athanasiadis A, Borgulya G, Voehringer M, Sechtem U. 3-year follow-up of patients with coronary artery spasm as cause of acute coronary syndrome: the CASPAR (coronary artery spasm in patients with acute coronary syndrome) study follow-up. J Am Coll Cardiol. 2011; 57:147–152. PMID: 21211685.21. JCS Joint Working Group. Guidelines for diagnosis and treatment of patients with vasospastic angina (Coronary Spastic Angina) (JCS 2013). Circ J. 2014; 78:2779–2801. PMID: 25273915.22. Li YJ, Hyun MH, Rha SW, Chen KY, Jin Z, Dang Q, et al. Diabetes mellitus is not a risk factor for coronary artery spasm as assessed by an intracoronary acetylcholine provocation test: angiographic and clinical characteristics of 986 patients. J Invasive Cardiol. 2014; 26:234–239. PMID: 24907077.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preventive Effect of Conduit Vessel Spasm after Coronary Artery Bypass Grafting Surgery
- Clinical and Hypotensive Experiences with Diltiazem Hydrochloride(Herben(R))in Essential Hypertension
- Effects of Botulinum Toxin Combined with Diltiazem on Blepharospasm and Hemifacial Spasm
- A Clinical Study on the Therapeutic Effect of Diltiazem(Herben(R)) in Angina Pectoris
- Clinical Observation on Effect of Diltiazem(Herben(R)) in Angina Pectoris