Korean J Ophthalmol.
2016 Aug;30(4):243-250. 10.3341/kjo.2016.30.4.243.
Preoperative Computed Tomography Findings for Patients with Nasolacrimal Duct Obstruction or Stenosis
- Affiliations
-
- 1Myunggok Eye Research Institute, Department of Ophthalmology, Kim's Eye Hospital, Konyang University College of Medicine, Seoul, Korea. katejung2000@kimeye.com
- KMID: 2373983
- DOI: http://doi.org/10.3341/kjo.2016.30.4.243
Abstract
- PURPOSE
To identify and analyze the role of preoperative computed tomography (CT) in patients with tearing symptoms with nasolacrimal duct obstruction (NLDO).
METHODS
We retrospectively reviewed the medical records and CT results on 218 patients who complained of tearing symptoms with NLDO between January 2014 and December 2014. All patients were recruited from Kim's Eye Hospital's outpatient clinic and assessed by clinical history, examination, and CT to evaluate periocular pathology and nasolacrimal drainage system. Patients with abnormal findings assessed by preoperative CT were further reviewed.
RESULTS
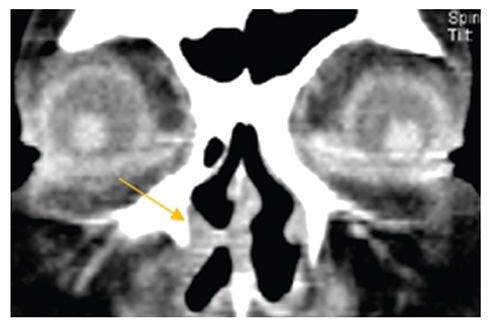
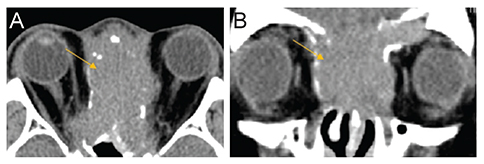
CT was performed on 218 patients (average age, 58.2 ± 11.9 years). Of these, 196 (89.9%) had endonasal dacryocystorhinostomy, 14 (6.4%) declined surgery, and 8 (3.7%) were inoperable due to abnormal CT findings. Soft tissue opacity was the most common finding which 243 cases (85.9%) of 283 obstructed nasolacrimal duct and 89 cases (81.7%) of 109 non-obstructed nasolacrimal duct showed it. Thirty-nine (17.8%) of 218 patients showed either maxillary sinusitis or ethmoidal sinusitis and 32 (14.7%) of 218 patients presented with periocular inflammation. Other abnormal CT findings included septal deviations, previous fractures, masses, and structural abnormalities of nasal cavity.
CONCLUSIONS
Preoperative CT imaging is useful in the assessment of both nasolacrimal drainage and nearby anatomical structures. This information will be helpful in planning surgical interventions and management of NLDO.
Keyword
MeSH Terms
Figure
Reference
-
1. Dalgleish R. Idiopathic acquired lacrimal drainage obstruction. Br J Ophthalmol. 1967; 51:463–468.2. Linberg JV, McCormick SA. Primary acquired nasolacrimal duct obstruction: a clinicopathologic report and biopsy technique. Ophthalmology. 1986; 93:1055–1063.3. Czyz CN, Bacon TS, Stacey AW, et al. Nasolacrimal system aeration on computed tomographic imaging: sex and age variation. Ophthal Plast Reconstr Surg. 2016; 32:11–16.4. Czyz CN, Bacon TS, Stacey AW, et al. Nasolacrimal system aeration on computed tomographic imaging: effects of patient positioning and scan orientation. Clin Ophthalmol. 2015; 9:469–473.5. Loftus WK, Kew J, Metreweli C. Nasolacrimal duct opacity on CT. Br J Radiol. 1996; 69:630–631.6. Francis IC, Kappagoda MB, Cole IE, et al. Computed tomography of the lacrimal drainage system: retrospective study of 107 cases of dacryostenosis. Ophthal Plast Reconstr Surg. 1999; 15:217–226.7. Lee KH, Han SH, Yoon JS. Case reports of lacrimal sac tumors discovered in patients with persistent epiphora following dacryocystorhinostomy. Korean J Ophthalmol. 2015; 29:66–67.8. Nagi KS, Meyer DR. Utilization patterns for diagnostic imaging in the evaluation of epiphora due to lacrimal obstruction: a national survey. Ophthal Plast Reconstr Surg. 2010; 26:168–171.9. Ibrahim HA, Batterbury M, Banhegyi G, McGalliard J. Endonasal laser dacryocystorhinostomy and external dacryocystorhinostomy outcome profile in a general ophthalmic service unit: a comparative retrospective study. Ophthalmic Surg Lasers. 2001; 32:220–227.10. Elner VM, Burnstine MA, Goodman ML, Dortzbach RK. Inverted papillomas that invade the orbit. Arch Ophthalmol. 1995; 113:1178–1183.11. Jung JH, Shin DH, Cho KS, Choi HY. Nasolacrimal duct obstruction caused by oncocytic carcinoma. Korean J Ophthalmol. 2013; 27:126–129.12. Roth SI, August CZ, Lissner GS, O'Grady RB. Hemangiopericytoma of the lacrimal sac. Ophthalmology. 1991; 98:925–927.13. Stefanyszyn MA, Hidayat AA, Pe'er JJ, Flanagan JC. Lacrimal sac tumors. Ophthal Plast Reconstr Surg. 1994; 10:169–184.14. Woog JJ, Kennedy RH, Custer PL, et al. Endonasal dacryocystorhinostomy: a report by the American Academy of Ophthalmology. Ophthalmology. 2001; 108:2369–2377.15. Russell EJ, Czervionke L, Huckman M, et al. CT of the inferomedial orbit and the lacrimal drainage apparatus: normal and pathologic anatomy. AJR Am J Roentgenol. 1985; 145:1147–1154.16. Merkonidis C, Brewis C, Yung M, Nussbaumer M. Is routine biopsy of the lacrimal sac wall indicated at dacryocystorhinostomy? A prospective study and literature review. Br J Ophthalmol. 2005; 89:1589–1591.17. Shams PN, Selva D. Acute post-operative rhinosinusitis following endonasal dacryocystorhinostomy. Eye (Lond). 2013; 27:1130–1136.18. Fayet B, Racy E, Assouline M. Complications of standardized endonasal dacryocystorhinostomy with unciformectomy. Ophthalmology. 2004; 111:837–845.19. Leong SC, Macewen CJ, White PS. A systematic review of outcomes after dacryocystorhinostomy in adults. Am J Rhinol Allergy. 2010; 24:81–90.20. Kenny TJ, Duncavage J, Bracikowski J, et al. Prospective analysis of sinus symptoms and correlation with paranasal computed tomography scan. Otolaryngol Head Neck Surg. 2001; 125:40–43.21. Bhattacharyya T, Piccirillo J, Wippold FJ 2nd. Relationship between patient-based descriptions of sinusitis and paranasal sinus computed tomographic findings. Arch Otolaryngol Head Neck Surg. 1997; 123:1189–1192.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Success Rate of Silicone Intubation Between Nasolacrimal Duct Obstruction and Stenosis According to Dacryocystography
- A Case of Nasolacrimal Duct Obstruction after Two-Jaw Surgery
- Silicone Intubation and Dacryocystographic Finding in Incomplete Nasolacrimal Duct Obstruction
- Nasolacrimal Duct Obstruction Following Midfacial Autologous Fat Injection
- A Case of Angioleiomyoma in Nasolacrimal Duct