Emergency Department Crowding Disparity: a Nationwide Cross-Sectional Study
- Affiliations
-
- 1Department of Emergency Medicine, Samsung Medical Center, Seoul, Korea.
- 2Department of Emergency Medicine, Seoul National University Hospital, Seoul, Korea. arendt75@gmail.com
- 3Department of Emergency Medicine, Gachon University Gil Hospital, Incheon, Korea.
- 4Laboratory of Emergency Medical Service, Biomedical Research Institute, Seoul National University Hospital, Seoul, Korea.
- KMID: 2373764
- DOI: http://doi.org/10.3346/jkms.2016.31.8.1331
Abstract
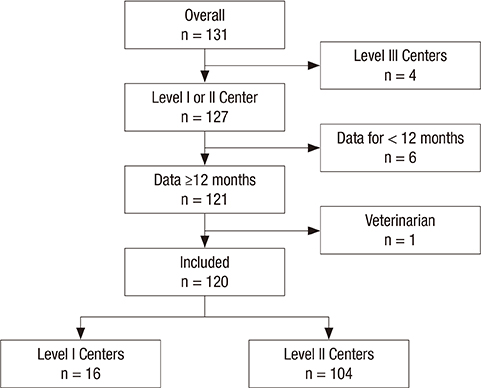
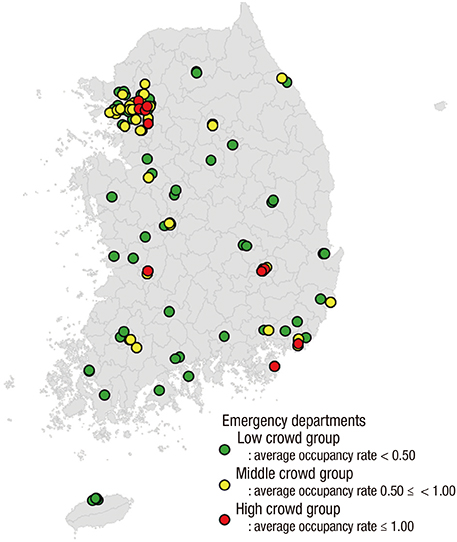
- In this study, we evaluated national differences in emergency department (ED) crowding to identify factors significantly associated with crowding in institutes and communities across Korea. This was a cross-sectional nationwide observational study using data abstracted from the National Emergency Department Information System (NEDIS). We calculated mean occupancy rates to quantify ED crowding status and divided EDs into three groups according to their occupancy rates (cutoffs: 0.5 and 1.0). Factors potentially related to ED crowding were collected from the NEDIS. We performed a multivariate regression analysis to identify variables significantly associated with ED crowding. A total of 120 EDs were included in the final analysis. Of these, 73 were categorized as 'low crowded' (LC, occupancy rate < 0.50), 37 as 'middle crowded' (MC, 0.50 ≤ occupancy rate < 1.00), 10 EDs as 'high crowded' (HC, 1.00 ≤ occupancy rate). The mean ED occupancy rate varied widely, from 0.06 to 2.33. The median value was 0.39 with interquartile ranges (IQRs) from 0.20 to 0.71. Multivariate analysis revealed that after adjustment, ED crowding was significantly associated with the number of visits, percentage of patients referred, number of nurses, and ED disposition. This nationwide study observed significant variety in ED crowding. Several input, throughput, and output factors were associated with crowding.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Interaction Effects between COVID-19 Outbreak and Community Income Levels on Excess Mortality among Patients Visiting Emergency Departments
Eujene Jung, Young Sun Ro, Hyun Ho Ryu, Sang Do Shin, Sungwoo Moon
J Korean Med Sci. 2021;36(13):e100. doi: 10.3346/jkms.2021.36.e100.Analysis of Patients with Acute Toxic Exposure between 2009 and 2013: Data from the Korea Health Insurance Review and Assessment Service and the National Emergency Department Information System
Young-Hoon Yoon, Jung-Youn Kim, Sung-Hyuk Choi
J Korean Med Sci. 2018;33(39):. doi: 10.3346/jkms.2018.33.e254.Impact of the COVID-19 Outbreak on Emergency Care Utilization in Patients with Acute Myocardial Infarction: a Nationwide Population-based Study
Ho Kyung Sung, Jin Hui Paik, Yu Jin Lee, Soo Kang
J Korean Med Sci. 2021;36(16):e111. doi: 10.3346/jkms.2021.36.e111.
Reference
-
1. Institute of Medicine Committee on the Future of Emergency Care in the United States Health System (US). Hospital-Based Emergency Care: at the Breaking Point. Washington, D.C.: National Academies Press;2007.2. Sun BC, Binstadt ES, Pelletier A, Camargo CA Jr. Characteristics and temporal trends of “left before being seen” visits in US emergency departments, 1995-2002. J Emerg Med. 2007; 32:211–215.3. Asaro PV, Lewis LM, Boxerman SB. Emergency department overcrowding: analysis of the factors of renege rate. Acad Emerg Med. 2007; 14:157–162.4. Pines JM, Localio AR, Hollander JE, Baxt WG, Lee H, Phillips C, Metlay JP. The impact of emergency department crowding measures on time to antibiotics for patients with community-acquired pneumonia. Ann Emerg Med. 2007; 50:510–516.5. Pines JM, Hollander JE. Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008; 51:1–5.6. Krochmal P, Riley TA. Increased health care costs associated with ED overcrowding. Am J Emerg Med. 1994; 12:265–266.7. Bayley MD, Schwartz JS, Shofer FS, Weiner M, Sites FD, Traber KB, Hollander JE. The financial burden of emergency department congestion and hospital crowding for chest pain patients awaiting admission. Ann Emerg Med. 2005; 45:110–117.8. Cameron PA. Hospital overcrowding: a threat to patient safety? Med J Aust. 2006; 184:203–204.9. Weber EJ, Mason S, Carter A, Hew RL. Emptying the corridors of shame: organizational lessons from England's 4-hour emergency throughput target. Ann Emerg Med. 2011; 57:79–88.e1.10. Hatamabady HR. 291: causes of length of stay in a typical crowded emergency department of a teaching hospital in Tehran capital city. Ann Emerg Med. 2008; 52:Suppl. S131.11. Miró O. State of emergency medicine in Spain. Int J Emerg Med. 2010; 3:219–226.12. American College of Emergency Physicians. Emergency department crowding information paper [Internet]. accessed on 24 Feburary 2016. Available at http://www.acep.org/workarea/DownloadAsset.aspx?id=8872.13. Derlet RW, Richards JR. Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000; 35:63–68.14. Derlet RW. Overcrowding in emergency departments: increased demand and decreased capacity. Ann Emerg Med. 2002; 39:430–432.15. Pham JC, Ho GK, Hill PM, McCarthy ML, Pronovost PJ. National study of patient, visit, and hospital characteristics associated with leaving an emergency department without being seen: predicting LWBS. Acad Emerg Med. 2009; 16:949–955.16. Hsia RY, Asch SM, Weiss RE, Zingmond D, Liang LJ, Han W, McCreath H, Sun BC. Hospital determinants of emergency department left without being seen rates. Ann Emerg Med. 2011; 58:24–32.e3.17. McCabe JB. Emergency department overcrowding: a national crisis. Acad Med. 2001; 76:672–674.18. Espinosa G, Miró O, Sánchez M, Coll-Vinent B, Millá J. Effects of external and internal factors on emergency department overcrowding. Ann Emerg Med. 2002; 39:693–695.19. Hoot NR, Leblanc LJ, Jones I, Levin SR, Zhou C, Gadd CS, Aronsky D. Forecasting emergency department crowding: a prospective, real-time evaluation. J Am Med Inform Assoc. 2009; 16:338–345.20. Han JH, Zhou C, France DJ, Zhong S, Jones I, Storrow AB, Aronsky D. The effect of emergency department expansion on emergency department overcrowding. Acad Emerg Med. 2007; 14:338–343.21. Solberg LI, Asplin BR, Weinick RM, Magid DJ. Emergency department crowding: consensus development of potential measures. Ann Emerg Med. 2003; 42:824–834.22. Ospina MB, Bond K, Schull M, Innes G, Blitz S, Rowe BH. Key indicators of overcrowding in Canadian emergency departments: a Delphi study. CJEM. 2007; 9:339–346.23. McCarthy ML, Aronsky D, Jones ID, Miner JR, Band RA, Baren JM, Desmond JS, Baumlin KM, Ding R, Shesser R. The emergency department occupancy rate: a simple measure of emergency department crowding? Ann Emerg Med. 2008; 51:15–24. 24.e1–24.e2.24. Hoot NR, Zhou C, Jones I, Aronsky D. Measuring and forecasting emergency department crowding in real time. Ann Emerg Med. 2007; 49:747–755.25. Asplin BR, Magid DJ, Rhodes KV, Solberg LI, Lurie N, Camargo CA Jr. A conceptual model of emergency department crowding. Ann Emerg Med. 2003; 42:173–180.26. Hwang U, McCarthy ML, Aronsky D, Asplin B, Crane PW, Craven CK, Epstein SK, Fee C, Handel DA, Pines JM, et al. Measures of crowding in the emergency department: a systematic review. Acad Emerg Med. 2011; 18:527–538.27. Bullard MJ, Villa-Roel C, Bond K, Vester M, Holroyd BR, Rowe BH. Tracking emergency department overcrowding in a tertiary care academic institution. Healthc Q. 2009; 12:99–106.28. Schull MJ, Slaughter PM, Redelmeier DA. Urban emergency department overcrowding: defining the problem and eliminating misconceptions. CJEM. 2002; 4:76–83.29. Schull MJ, Morrison LJ, Vermeulen M, Redelmeier DA. Emergency department gridlock and out-of-hospital delays for cardiac patients. Acad Emerg Med. 2003; 10:709–716.30. Asaro PV, Lewis LM, Boxerman SB. The impact of input and output factors on emergency department throughput. Acad Emerg Med. 2007; 14:235–242.31. Steele R, Kiss A. EMDOC (Emergency Department overcrowding) Internet-based safety net research. J Emerg Med. 2008; 35:101–107.32. Jones SS, Evans RS, Allen TL, Thomas A, Haug PJ, Welch SJ, Snow GL. A multivariate time series approach to modeling and forecasting demand in the emergency department. J Biomed Inform. 2009; 42:123–139.33. Park HA, Ahn KO, Shin SD, Cha WC, Ro YS. The Effect of emergency medical service use and inter-hospital transfer on prehospital delay among ischemic stroke patients: a multicenter observational study. J Korean Med Sci. 2016; 31:139–146.34. Kwak YH, Kim DK, Jang HY. Utilization of emergency department by children in Korea. J Korean Med Sci. 2012; 27:1222–1228.35. Kang SW, Park HS. Emergency department visit volume variability. Clin Exp Emerg Med. 2015; 2:150–154.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A study on the change of posterior availble space and the relationship between posterior available space and crowding
- Parental satisfaction with pediatric emergency care: a nationwide, cross-sectional survey in Korea
- Emergency department and hospital crowding: causes, consequences, and cures
- Improving emergency department patient flow
- An Experience of Operating the Pediatric Emergency Room