J Korean Med Sci.
2016 Aug;31(8):1266-1272. 10.3346/jkms.2016.31.8.1266.
Clinical Outcomes of Cryopreserved Arterial Allograft Used as a Vascular Conduit for Hemodialysis
- Affiliations
-
- 1Department of Surgery, University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea. ypcho@amc.seoul.kr
- 2Department of Internal Medicine University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea.
- 3Department of Pathology, University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea.
- KMID: 2373755
- DOI: http://doi.org/10.3346/jkms.2016.31.8.1266
Abstract
- This single center cohort study aimed to test the hypothesis that use of a cryopreserved arterial allograft could avoid the maturation or healing process of a new vascular access and to evaluate the patency of this technique compared with that of vascular access using a prosthetic graft. Between April 2012 and March 2013, 20 patients underwent an upper arm vascular access using a cryopreserved arterial allograft for failed or failing vascular accesses and 53 using a prosthetic graft were included in this study. The mean duration of catheter dependence, calculated as the time interval from upper arm access placement to removal of the tunneled central catheter after successful cannulation of the access, was significantly longer for accesses using a prosthetic graft than a cryopreserved arterial allograft (34.4 ± 11.39 days vs. 4.9 ± 8.5 days, P < 0.001). In the allograft group, use of vascular access started within 7 days in 16 patients (80%), as soon as from the day of surgery in 10 patients. Primary (unassisted; P = 0.314) and cumulative (assisted; P = 0.673) access survivals were similar in the two groups. There were no postoperative complications related to the use of a cryopreserved iliac arterial allograft except for one patient who experienced wound hematoma. In conclusion, upper arm vascular access using a cryopreserved arterial allograft may permit immediate hemodialysis without the maturation or healing process, resulting in access survival comparable to that of an access using a prosthetic graft.
MeSH Terms
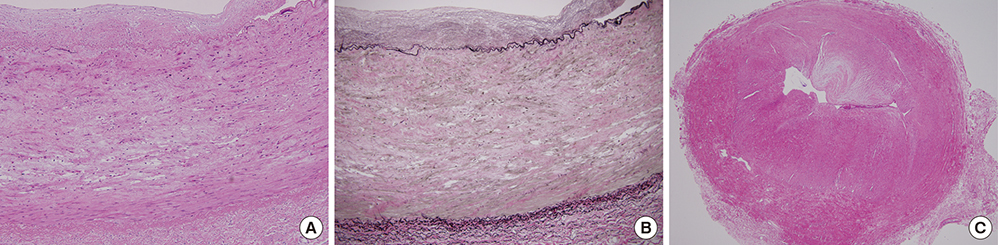
Figure
Reference
-
1. Caroli A, Manini S, Antiga L, Passera K, Ene-Iordache B, Rota S, Remuzzi G, Bode A, Leermakers J, van de Vosse FN, et al. Validation of a patient-specific hemodynamic computational model for surgical planning of vascular access in hemodialysis patients. Kidney Int. 2013; 84:1237–1245.2. Sidawy AN, Spergel LM, Besarab A, Allon M, Jennings WC, Padberg FT Jr, Murad MH, Montori VM, O'Hare AM, Calligaro KD, et al. The Society for Vascular Surgery: clinical practice guidelines for the surgical placement and maintenance of arteriovenous hemodialysis access. J Vasc Surg. 2008; 48:2S–25S.3. Long B, Brichart N, Lermusiaux P, Turmel-Rodrigues L, Artru B, Boutin JM, Pengloan J, Bertrand P, Bruyère F. Management of perianastomotic stenosis of direct wrist autogenous radial-cephalic arteriovenous accesses for dialysis. J Vasc Surg. 2011; 53:108–114.4. Rooijens PP, Tordoir JH, Stijnen T, Burgmans JP. Smet de AA, Yo TI. Radiocephalic wrist arteriovenous fistula for hemodialysis: meta-analysis indicates a high primary failure rate. Eur J Vasc Endovasc Surg. 2004; 28:583–589.5. Roy-Chaudhury P, Sukhatme VP, Cheung AK. Hemodialysis vascular access dysfunction: a cellular and molecular viewpoint. J Am Soc Nephrol. 2006; 17:1112–1127.6. Clark EG, Barsuk JH. Temporary hemodialysis catheters: recent advances. Kidney Int. 2014; 86:888–895.7. Benedetto B, Lipkowitz G, Madden R, Kurbanov A, Hull D, Miller M, Bow L. Use of cryopreserved cadaveric vein allograft for hemodialysis access precludes kidney transplantation because of allosensitization. J Vasc Surg. 2001; 34:139–142.8. Kim HO, Kim J, Jin HL. Evaluation of domestic cryostorage blood bags. Korean J Blood Transfus. 2006; 17:48–53.9. Pegg DE, Wusteman MC, Boylan S. Fractures in cryopreserved elastic arteries. Cryobiology. 1997; 34:183–192.10. Lee T, Barker J, Allon M. Comparison of survival of upper arm arteriovenous fistulas and grafts after failed forearm fistula. J Am Soc Nephrol. 2007; 18:1936–1941.11. Asif A, Cherla G, Merrill D, Cipleu CD, Briones P, Pennell P. Conversion of tunneled hemodialysis catheter-consigned patients to arteriovenous fistula. Kidney Int. 2005; 67:2399–2406.12. Szilagyi DE, McDonald RT, Smith RF, Whitcomb JG, Whitcomb JG. Biologic fate of human arterial homografts. AMA Arch Surg. 1957; 75:506–527.13. Allaire E, Guettier C, Bruneval P, Plissonnier D, Michel JB. Cell-free arterial grafts: morphologic characteristics of aortic isografts, allografts, and xenografts in rats. J Vasc Surg. 1994; 19:446–456.14. Schmitz-Rixen T, Megerman J, Colvin RB, Williams AM, Abbott WM. Immunosuppressive treatment of aortic allografts. J Vasc Surg. 1988; 7:82–92.15. Bia D, Pessana F, Armentano R, Pérez H, Graf S, Zócalo Y, Saldías M, Perez N, Alvarez O, Silva W, et al. Cryopreservation procedure does not modify human carotid homografts mechanical properties: an isobaric and dynamic analysis. Cell Tissue Bank. 2006; 7:183–194.16. Kieffer E, Gomes D, Chiche L, Fléron MH, Koskas F, Bahnini A. Allograft replacement for infrarenal aortic graft infection: early and late results in 179 patients. J Vasc Surg. 2004; 39:1009–1017.17. Madden RL, Lipkowitz GS, Browne BJ, Kurbanov A. A comparison of cryopreserved vein allografts and prosthetic grafts for hemodialysis access. Ann Vasc Surg. 2005; 19:686–691.18. Kakkos SK, Andrzejewski T, Haddad JA, Haddad GK, Reddy DJ, Nypaver TJ, Scully MM, Schmid DL. Equivalent secondary patency rates of upper extremity Vectra Vascular Access Grafts and transposed brachial-basilic fistulas with aggressive access surveillance and endovascular treatment. J Vasc Surg. 2008; 47:407–414.19. Walker PJ, Mitchell RS, McFadden PM, James DR, Mehigan JT. Early experience with cryopreserved saphenous vein allografts as a conduit for complex limb-salvage procedures. J Vasc Surg. 1993; 18:561–569.20. Zehr BP, Niblick CJ, Downey H, Ladowski JS. Limb salvage with CryoVein cadaver saphenous vein allografts used for peripheral arterial bypass: role of blood compatibility. Ann Vasc Surg. 2011; 25:177–181.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Use of cryopreserved cadaveric arterial allograft as a vascular conduit for peripheral arterial graft infection
- Flow Cytometric Analysis of Endothelial Cell Viability in Arterial Allograft
- Comparison of Patency and Viability in Fresh and Cryopreserved Arterialand Venous Allograft Conduits in Dogs
- Flow Measurement in the Vascular Access Conduit: an Ex Vivo Experimental Model
- Flow Measurement in the Hemodialysis Vascular Conduit for Surveillance of Internal Arteriovenous Fistula: A Trend Analysis