J Korean Med Sci.
2016 Jul;31(7):1049-1054. 10.3346/jkms.2016.31.7.1049.
Peri-Transplant Change in AFP Level: a Useful Predictor of Hepatocellular Carcinoma Recurrence Following Liver Transplantation
- Affiliations
-
- 1Department of Surgery, Seoul National University College of Medicine, Seoul, Korea. kwleegs@gmail.com
- 2Department of Surgery, Hallym University College of Medicine, Hwaseong, Korea.
- KMID: 2373722
- DOI: http://doi.org/10.3346/jkms.2016.31.7.1049
Abstract
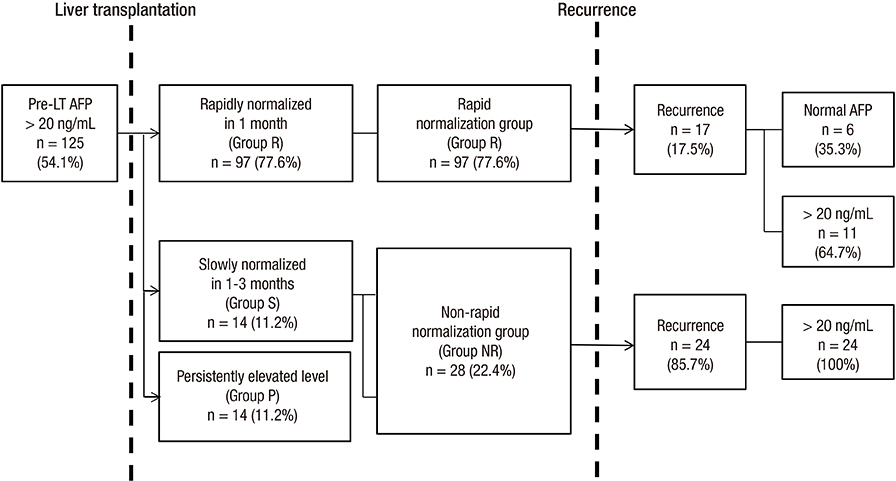
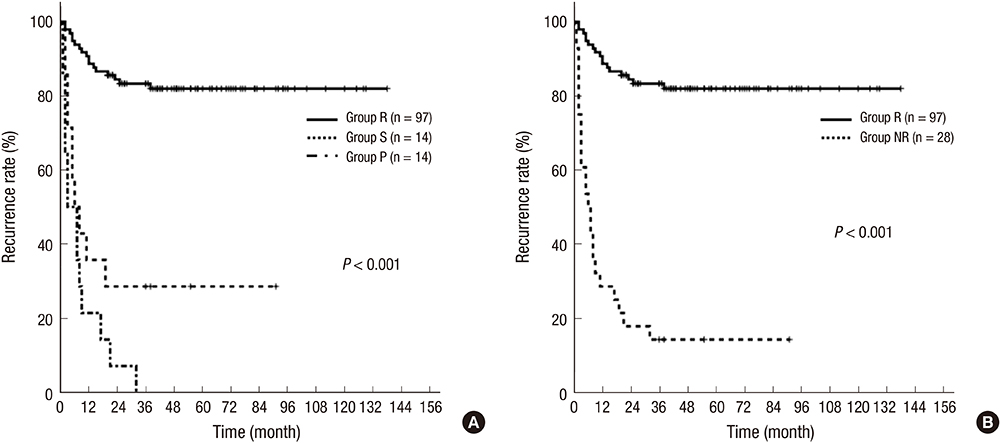
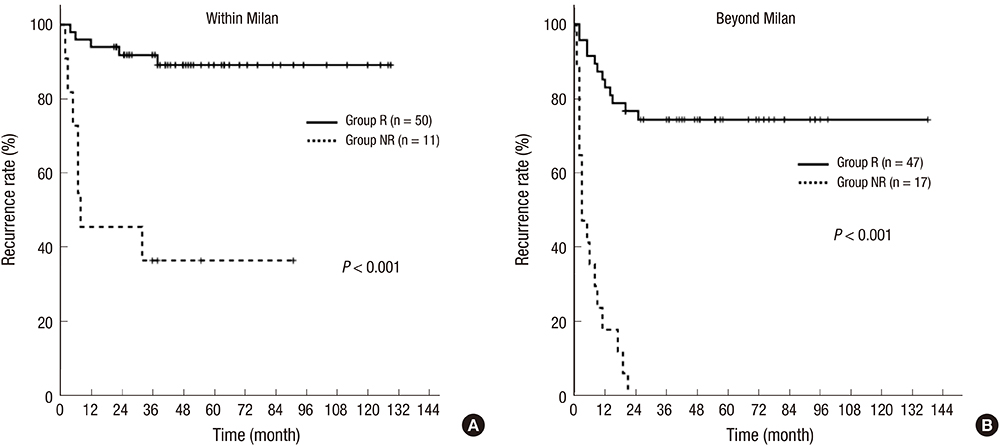
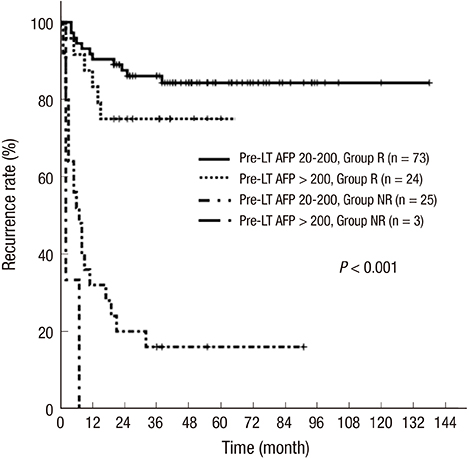
- Pretransplant alpha-fetoprotein (AFP) is a useful tumor marker predicting recurrence of hepatocellular carcinoma (HCC). Little is known, however, about the relationship between changes in AFP concentration and prognosis. This study investigated the clinical significance of change in peri-transplant AFP level as a predictor of HCC recurrence. Data from 125 HCC patients with elevated pretransplant AFP level who underwent liver transplantation (LT) between February 2000 and December 2010 were retrospectively reviewed. Patients with AFP normalization within 1 month after LT were classified into the rapid normalization group (n = 97), with all other patients classified into the non-rapid normalization group (n = 28). Tumor recurrence was observed in 17 of the 97 patients (17.5%) with rapid normalization; of these, 11 patients had high AFP levels and six had normal levels at recurrence. In contrast, tumor recurrence was observed in 24 of the 28 patients (85.7%) without rapid normalization, with all 24 having high AFP levels at recurrence. Multivariate analysis showed that non-rapid normalization (harzard ratio [HR], 4.41, P < 0.001), sex (HR, 3.26, P = 0.03), tumor size (HR, 1.15, P = 0.001), and microvascular invasion (HR, 2.65, P = 0.005) were independent risk factors for recurrence. In conclusion, rapid normalization of post-LT AFP level at 1 month is a useful clinical marker for HCC recurrence. Therefore, an adjuvant strategy and/or intensive screening are needed for patients who do not show rapid normalization.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Biomarkers, Tumor/analysis
Carcinoma, Hepatocellular/blood/mortality/*pathology/therapy
Female
Humans
Kaplan-Meier Estimate
Liver Neoplasms/blood/mortality/*pathology/therapy
*Liver Transplantation
Male
Middle Aged
Multivariate Analysis
Neoplasm Recurrence, Local
Proportional Hazards Models
Retrospective Studies
Risk Factors
Severity of Illness Index
alpha-Fetoproteins/analysis
Biomarkers, Tumor
alpha-Fetoproteins
Figure
Reference
-
1. Debruyne EN, Delanghe JR. Diagnosing and monitoring hepatocellular carcinoma with alpha-fetoprotein: new aspects and applications. Clin Chim Acta. 2008; 395:19–26.2. Trevisani F, D’Intino PE, Morselli-Labate AM, Mazzella G, Accogli E, Caraceni P, Domenicali M, De Notariis S, Roda E, Bernardi M. Serum alpha-fetoprotein for diagnosis of hepatocellular carcinoma in patients with chronic liver disease: influence of HBsAg and anti-HCV status. J Hepatol. 2001; 34:570–575.3. Yao FY, Ferrell L, Bass NM, Watson JJ, Bacchetti P, Venook A, Ascher NL, Roberts JP. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology. 2001; 33:1394–1403.4. Zou WL, Zang YJ, Chen XG, Shen ZY. Risk factors for fatal recurrence of hepatocellular carcinoma and their role in selecting candidates for liver transplantation. Hepatobiliary Pancreat Dis Int. 2008; 7:145–151.5. Wang ZX, Song SH, Teng F, Wang GH, Guo WY, Shi XM, Ma J, Wu YM, Ding GS, Fu ZR. A single-center retrospective analysis of liver transplantation on 255 patients with hepatocellular carcinoma. Clin Transplant. 2010; 24:752–757.6. Toyoda H, Kumada T, Tada T, Niinomi T, Ito T, Kaneoka Y, Maeda A. Prognostic significance of a combination of pre- and post-treatment tumor markers for hepatocellular carcinoma curatively treated with hepatectomy. J Hepatol. 2012; 57:1251–1257.7. Nobuoka D, Kato Y, Gotohda N, Takahashi S, Nakagohri T, Konishi M, Kinoshita T, Nakatsura T. Postoperative serum alpha-fetoprotein level is a useful predictor of recurrence after hepatectomy for hepatocellular carcinoma. Oncol Rep. 2010; 24:521–528.8. Sugawara Y, Tamura S, Makuuchi M. Living donor liver transplantation for hepatocellular carcinoma: Tokyo University series. Dig Dis. 2007; 25:310–312.9. Xu X, Ke QH, Shao ZX, Wu J, Chen J, Zhou L, Zheng SS. The value of serum alpha-fetoprotein in predicting tumor recurrence after liver transplantation for hepatocellular carcinoma. Dig Dis Sci. 2009; 54:385–388.10. Hameed B, Mehta N, Sapisochin G, Roberts JP, Yao FY. Alpha-fetoprotein level > 1000 ng/mL as an exclusion criterion for liver transplantation in patients with hepatocellular carcinoma meeting the Milan criteria. Liver Transpl. 2014; 20:945–951.11. Lee KW, Yi NJ, Suh KS. Section 5. Further expanding the criteria for HCC in living donor liver transplantation: when not to transplant: SNUH experience. Transplantation. 2014; 97:Suppl 8. S20–3.12. Yang SH, Suh KS, Lee HW, Cho EH, Cho JY, Cho YB, Kim IH, Yi NJ, Lee KU. A revised scoring system utilizing serum alphafetoprotein levels to expand candidates for living donor transplantation in hepatocellular carcinoma. Surgery. 2007; 141:598–609.13. Duvoux C, Roudot-Thoraval F, Decaens T, Pessione F, Badran H, Piardi T, Francoz C, Compagnon P, Vanlemmens C, Dumortier J, et al. Liver transplantation for hepatocellular carcinoma: a model including α-fetoprotein improves the performance of Milan criteria. Gastroenterology. 2012; 143:986–994.e3.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Liver Transplantation for Advanced Hepatocellular Carcinoma
- Usefulness of Lens Culinaris Agglutinin-A Reactive Alpha-Fetoprotein for the Diagnosis of Hepatocelluar Carcinoma in Patients with Chronic Liver Disease Who Showed Significant Increment of Serum Alpha-Fetoprotein Level and No Mass Lesion in the Liver on Ultrasonogram
- Can hepatocellular carcinoma recurrence be prevented after liver transplantation?
- Impact of tumor biology on outcomes of radical therapy for hepatocellular carcinoma oligo-recurrence after liver transplantation
- Late hepatocellular carcinoma recurrence after living donor liver transplantation: unmet need