Korean J Gastroenterol.
2015 Sep;66(3):144-149. 10.4166/kjg.2015.66.3.144.
Recent Advances in Management of Chronic Pancreatitis
- Affiliations
-
- 1Department of Internal Medicine, Chungbuk National University College of Medicine, Cheongju, Korea. smpark@chungbuk.ac.kr
- KMID: 2373329
- DOI: http://doi.org/10.4166/kjg.2015.66.3.144
Abstract
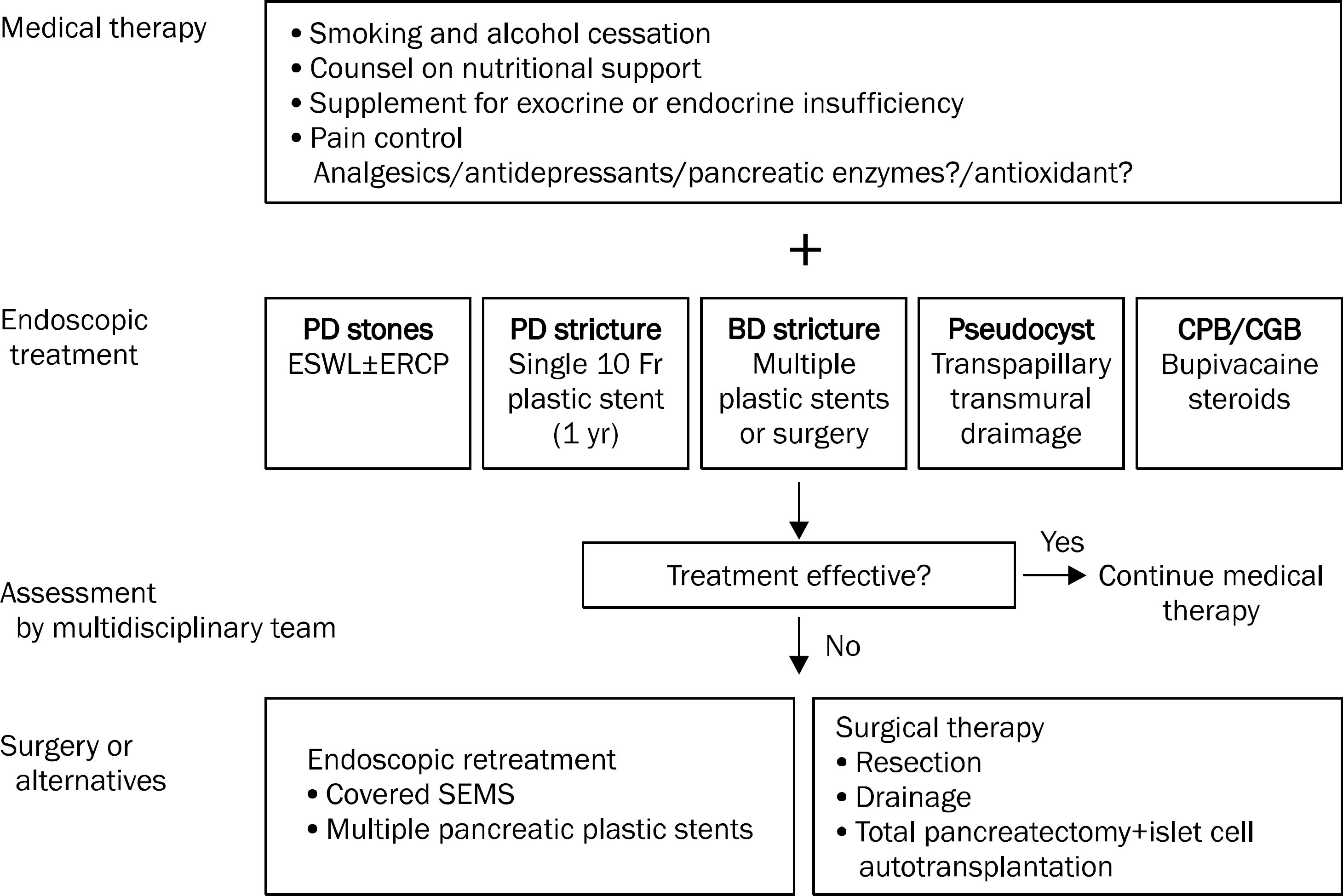
- Treatment for chronic pancreatitis (CP) should be started early to prevent further pancreatic fibrosis and managed with a multidisciplinary approach to prevent complications and to maintain a good quality of life. The management strategies of CP can be divided into medical, endoscopic, and surgical treatment. The role of pancreatic enzymes and antioxidants for pain relief is not clearly defined, but their role in maintaining nutritional support by correcting exocrine insufficiency is well established. Endoscopic treatment is applied for resolution of pancreatic or bile duct strictures, clearance of pancreatic duct stones, and pseudocyst drainage. Endosonography-guided celiac plexus or celiac ganglia block for pain relief are known to be safe procedures but evidence for their effectiveness is still lacking. Surgery is commonly recommended when endoscopic therapy fails or there is suspicion of malignancy. New evidence-based guidelines for the management of CP are needed.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Pancreatitis, Panniculitis, and Polyarthritis Syndrome Simulating Cellulitis and Gouty Arthritis
Ee Jin Kim, Min Soo Park, Hyung-Gon Son, Won Sup Oh, Ki Won Moon, Jin Myung Park, Chang Don Kang, Seungkoo Lee
Korean J Gastroenterol. 2019;74(3):175-182. doi: 10.4166/kjg.2019.74.3.175.
Reference
-
References
1. Olesen SS, Juel J, Graversen C, Kolesnikov Y, Wilder-Smith OH, Drewes AM. Pharmacological pain management in chronic pancreatitis. World J Gastroenterol. 2013; 19:7292–7301.
Article2. Forsmark CE. Management of chronic pancreatitis. Gastroenterology. 2013; 144:1282–1291.
Article3. Adler DG, Lichtenstein D, Baron TH, et al. The role of endoscopy in patients with chronic pancreatitis. Gastrointest Endosc. 2006; 63:933–937.
Article4. Dumonceau JM, Delhaye M, Tringali A, et al. Endoscopic treatment of chronic pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2012; 44:784–800.
Article5. Lieb JG 2nd, Forsmark CE. Review article: pain and chronic pancreatitis. Aliment Pharmacol Ther. 2009; 29:706–719.6. Warshaw AL, Banks PA, Fernández-Del Castillo C. AGA technical review: treatment of pain in chronic pancreatitis. Gastroenterology. 1998; 115:765–776.
Article7. Isaksson G, Ihse I. Pain reduction by an oral pancreatic enzyme preparation in chronic pancreatitis. Dig Dis Sci. 1983; 28:97–102.
Article8. Slaff J, Jacobson D, Tillman CR, Curington C, Toskes P. Protease- specific suppression of pancreatic exocrine secretion. Gastroenterology. 1984; 87:44–52.9. Brown A, Hughes M, Tenner S, Banks PA. Does pancreatic enzyme supplementation reduce pain in patients with chronic pancreatitis: a metaanalysis. Am J Gastroenterol. 1997; 92:2032–2035.10. Somogyi L, Toskes PP. Can a metaanalysis that mixes apples with oranges be used to demonstrate that pancreatic enzymes do not decrease abdominal pain in patients with chronic pancreatitis? Am J Gastroenterol. 1998; 93:1396–1398.
Article11. Keller J, Layer P. Human pancreatic exocrine response to nutrients in health and disease. Gut. 2005; 54(Suppl 6):vi1–vi28.
Article12. Löhr JM, Hummel FM, Pirilis KT, Steinkamp G, Körner A, Henniges F. Properties of different pancreatin preparations used in pancreatic exocrine insufficiency. Eur J Gastroenterol Hepatol. 2009; 21:1024–1031.
Article13. Trang T, Chan J, Graham DY. Pancreatic enzyme replacement therapy for pancreatic exocrine insufficiency in the 21(st) century. World J Gastroenterol. 2014; 20:11467–11485.14. Yoo KS. Medical treatment of chronic pancreatitis. Korean J Med. 2012; 83:18–28.
Article15. Bhardwaj P, Garg PK, Maulik SK, Saraya A, Tandon RK, Acharya SK. A randomized controlled trial of antioxidant supplementation for pain relief in patients with chronic pancreatitis. Gastroenterology. 2009; 136:149–159.
Article16. Siriwardena AK, Mason JM, Sheen AJ, Makin AJ, Shah NS. Antioxidant therapy does not reduce pain in patients with chronic pancreatitis: the ANTICIPATE study. Gastroenterology. 2012; 143:655–663.
Article17. Cai GH, Huang J, Zhao Y, et al. Antioxidant therapy for pain relief in patients with chronic pancreatitis: systematic review and metaanalysis. Pain Physician. 2013; 16:521–532.18. Ahmed Ali U, Jens S, Busch OR, et al. Antioxidants for pain in chronic pancreatitis. Cochrane Database Syst Rev. 2014; 8:CD008945.
Article19. Rustagi T, Njei B. Antioxidant therapy for pain reduction in patients with chronic pancreatitis: a systematic review and metaanalysis. Pancreas. 2015; 44:812–818.20. Pezzilli R. Antioxidants are not useful in reducing both pain and inflammation in chronic pancreatitis. Recent Pat Inflamm Allergy Drug Discov. 2014; 8:19–23.
Article21. Vitale GC, Cothron K, Vitale EA, et al. Role of pancreatic duct stenting in the treatment of chronic pancreatitis. Surg Endosc. 2004; 18:1431–1434.
Article22. Eleftherladis N, Dinu F, Delhaye M, et al. Longterm outcome after pancreatic stenting in severe chronic pancreatitis. Endoscopy. 2005; 37:223–230.
Article23. Costamagna G, Bulajic M, Tringali A, et al. Multiple stenting of refractory pancreatic duct strictures in severe chronic pancreatitis: long-term results. Endoscopy. 2006; 38:254–259.
Article24. Park do H, Kim MH, Moon SH, Lee SS, Seo DW, Lee SK. Feasibility and safety of placement of a newly designed, fully covered self-expandable metal stent for refractory benign pancreatic ductal strictures: a pilot study (with video). Gastrointest Endosc. 2008; 68:1182–1189.25. Moon SH, Kim MH, Park do H, et al. Modified fully covered self-ex-pandable metal stents with antimigration features for benign pancreatic-duct strictures in advanced chronic pancreatitis, with a focus on the safety profile and reducing migration. Gastrointest Endosc. 2010; 72:86–91.
Article26. Brauer BC, Chen YK, Fukami N, Shah RJ. Single-operator EUS-guided cholangiopancreatography for difficult pancreaticobiliary access (with video). Gastrointest Endosc. 2009; 70:471–479.
Article27. Inui K, Tazuma S, Yamaguchi T, et al. Treatment of pancreatic stones with extracorporeal shock wave lithotripsy: results of a multicenter survey. Pancreas. 2005; 30:26–30.28. Kozarek RA, Brandabur JJ, Ball TJ, et al. Clinical outcomes in patients who undergo extracorporeal shock wave lithotripsy for chronic calcific pancreatitis. Gastrointest Endosc. 2002; 56:496–500.
Article29. Kim YH, Jang SI, Rhee K, Lee DK. Endoscopic treatment of pancreatic calculi. Clin Endosc. 2014; 47:227–235.
Article30. Sherman S, Lehman GA, Hawes RH, et al. Pancreatic ductal stones: frequency of successful endoscopic removal and improvement in symptoms. Gastrointest Endosc. 1991; 37:511–517.
Article31. Brand B, Kahl M, Sidhu S, et al. Prospective evaluation of morphology, function, and quality of life after extracorporeal shockwave lithotripsy and endoscopic treatment of chronic calcific pancreatitis. Am J Gastroenterol. 2000; 95:3428–3438.
Article32. Jacobson BC, Baron TH, Adler DG, et al. American Society for Gastrointestinal Endoscopy. ASGE guideline: the role of endoscopy in the diagnosis and the management of cystic lesions and inflammatory fluid collections of the pancreas. Gastrointest Endosc. 2005; 61:363–370.
Article33. Rosso E, Alexakis N, Ghaneh P, et al. Pancreatic pseudocyst in chronic pancreatitis: endoscopic and surgical treatment. Dig Surg. 2003; 20:397–406.
Article34. Binmoeller KF, Seifert H, Walter A, Soehendra N. Transpapillary and transmural drainage of pancreatic pseudocysts. Gastrointest Endosc. 1995; 42:219–224.
Article35. Beckingham IJ, Krige JE, Bornman PC, Terblanche J. Endoscopic management of pancreatic pseudocysts. Br J Surg. 1997; 84:1638–1645.
Article36. Balachandra S, Siriwardena AK. Systematic appraisal of the management of the major vascular complications of pancreatitis. Am J Surg. 2005; 190:489–495.
Article37. Lawrence C, Howell DA, Stefan AM, et al. Disconnected pancreatic tail syndrome: potential for endoscopic therapy and results of long-term follow-up. Gastrointest Endosc. 2008; 67:673–679.
Article38. Banerjee S, Shen B, Baron HT, et al. Asge Standards of Practice Committee. Antibiotic prophylaxis for GI endoscopy. Gastrointest Endosc. 2008; 67:791–798.
Article39. Frey CF, Suzuki M, Isaji S. Treatment of chronic pancreatitis complicated by obstruction of the common bile duct or duodenum. World J Surg. 1990; 14:59–69.
Article40. Pozsár J, Sahin P, László F, Forró G, Topa L. Medium-term results of endoscopic treatment of common bile duct strictures in chronic calcifying pancreatitis with increasing numbers of stents. J Clin Gastroenterol. 2004; 38:118–123.
Article41. Siiki A, Helminen M, Sand J, Laukkarinen J. Covered self-expanding metal stents may be preferable to plastic stents in the treatment of chronic pancreatitis-related biliary strictures: a systematic review comparing 2 methods of stent therapy in benign biliary strictures. J Clin Gastroenterol. 2014; 48:635–643.42. Kaufman M, Singh G, Das S, et al. Efficacy of endoscopic ultrasound-guided celiac plexus block and celiac plexus neurolysis for managing abdominal pain associated with chronic pancreatitis and pancreatic cancer. J Clin Gastroenterol. 2010; 44:127–134.
Article43. Gress F, Schmitt C, Sherman S, Ciaccia D, Ikenberry S, Lehman G. Endoscopic ultrasound-guided celiac plexus block for managing abdominal pain associated with chronic pancreatitis: a prospective single center experience. Am J Gastroenterol. 2001; 96:409–416.
Article44. Santosh D, Lakhtakia S, Gupta R, et al. Clinical trial: a randomized trial comparing fluoroscopy guided percutaneous technique vs. endoscopic ultrasound guided technique of coeliac plexus block for treatment of pain in chronic pancreatitis. Aliment Pharmacol Ther. 2009; 29:979–984.
Article45. Doi S, Yasuda I, Kawakami H, et al. Endoscopic ultrasound-guided celiac ganglia neurolysis vs. celiac plexus neurolysis: a randomized multicenter trial. Endoscopy. 2013; 45:362–369.
Article46. Choi D. Surgical treatment of chronic pancreatitis. Korean J Med. 2012; 83:40–49.
Article47. Cahen DL, Gouma DJ, Nio Y, et al. Endoscopic versus surgical drainage of the pancreatic duct in chronic pancreatitis. N Engl J Med. 2007; 356:676–684.
Article48. Cahen DL, Gouma DJ, Laramée P, et al. Longterm outcomes of endoscopic vs surgical drainage of the pancreatic duct in patients with chronic pancreatitis. Gastroenterology. 2011; 141:1690–1695.
Article49. Hirota M, Asakura T, Kanno A, et al. Long-period pancreatic stenting for painful chronic calcified pancreatitis required higher medical costs and frequent hospitalizations compared with surgery. Pancreas. 2011; 40:946–950.
Article50. Laramée P, Wonderling D, Cahen DL, et al. Trial-based cost-effectiveness analysis comparing surgical and endoscopic drainage in patients with obstructive chronic pancreatitis. BMJ Open. 2013; 3:e003676.
Article51. Witkowski P, Savari O, Matthews JB. Islet autotransplantation and total pancreatectomy. Adv Surg. 2014; 48:223–233.
Article52. Ahmed Ali U, Issa Y, Bruno MJ, et al. Dutch Pancreatitis Study Group. Early surgery versus optimal current step-up practice for chronic pancreatitis (ESCAPE): design and rationale of a randomized trial. BMC Gastroenterol. 2013; 13:49.
Article