Korean J Gastroenterol.
2015 Jun;65(6):375-378. 10.4166/kjg.2015.65.6.375.
A Case of Lead Poisoning with Drug-induced Liver Injury after Ingestion of Herbal Medicine
- Affiliations
-
- 1Department of Internal Medicine, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. neakker@gmail.com
- KMID: 2373241
- DOI: http://doi.org/10.4166/kjg.2015.65.6.375
Abstract
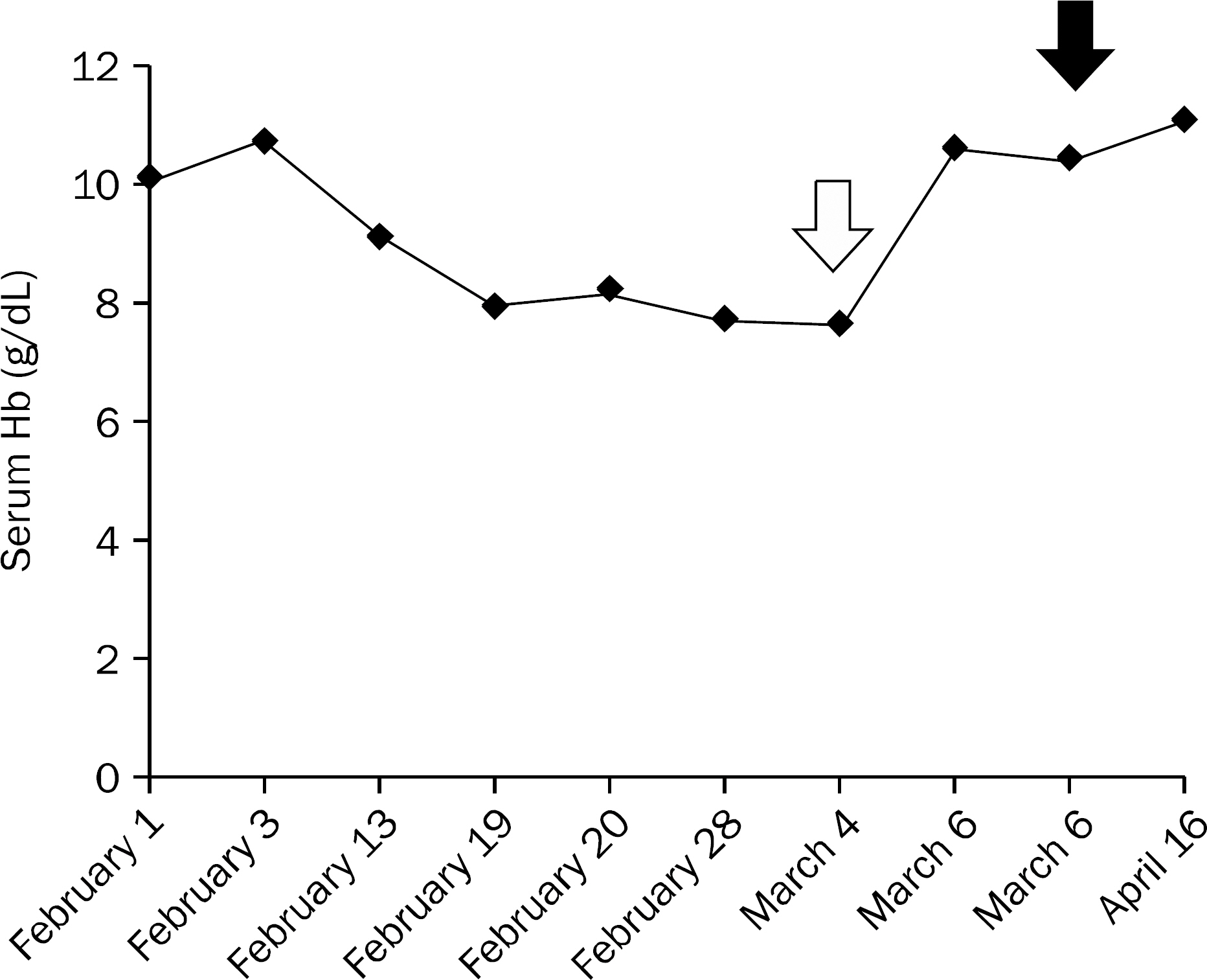
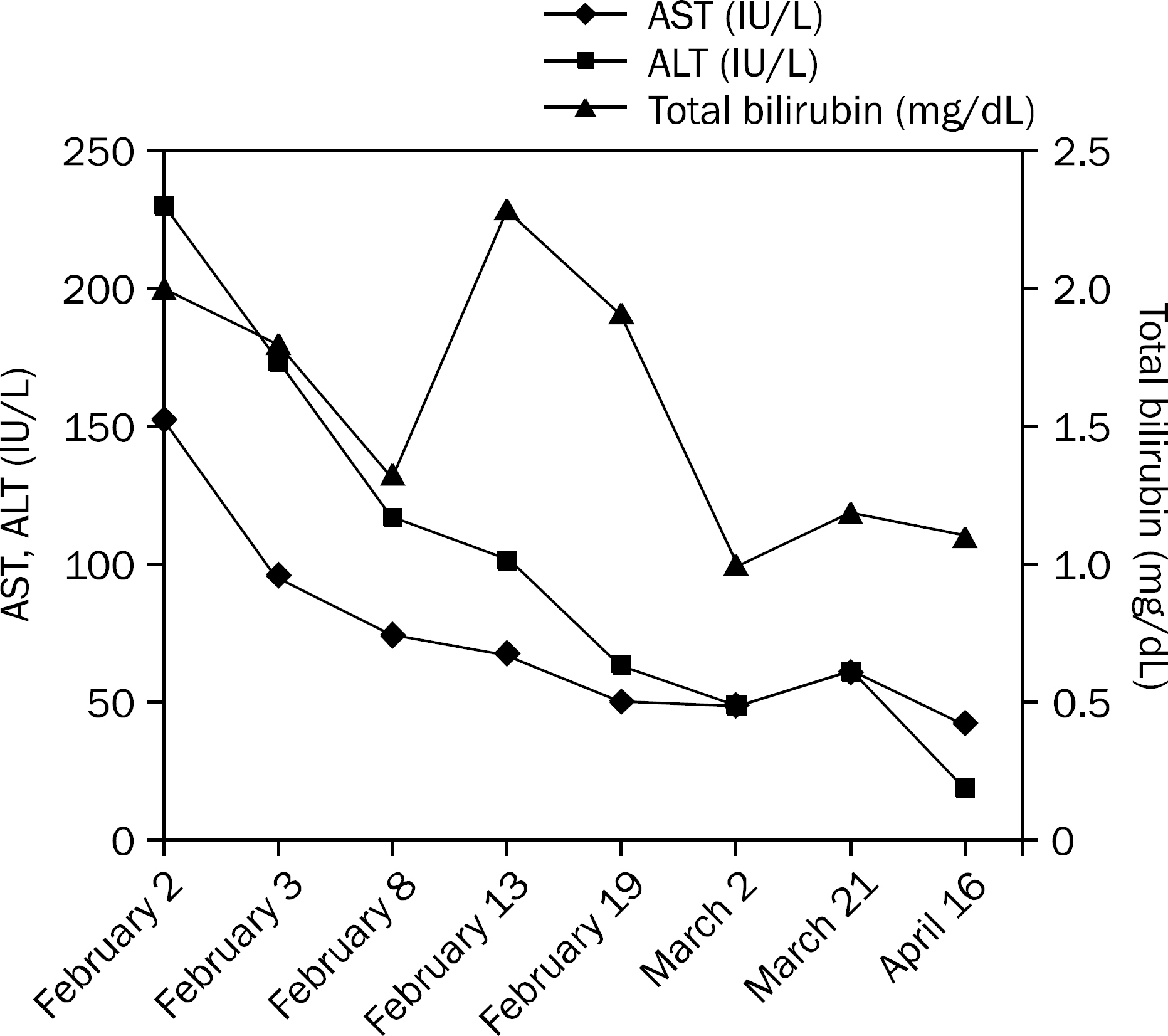
- A 61-year-old male patient was admitted because of unexplained abdominal pain and anemia. His past medical history was unremarkable except for having taken herbal medicine to treat facial palsy two months ago. The result of health examination performed about a month ago showed increased serum aspartate and alanine aminotransferase level, and he was diagnosed with toxic hepatitis by herbal medicine. When the patient presented to the outpatient department three weeks ago, follow-up liver function test results showed improvement but he complained of abdominal pain. Despite extensive blood chemistry tests and computed tomography, the cause of pain could not be found. After much deliberation, serum lead level and herbal medicines analysis was performed based on the fact that he took herbal medicine two months ago, and he could finally be diagnosed with lead poisoning. Since the serum lead level was high enough to be indicated for lead chelating therapy, conservative management was given. When a patient with toxic hepatitis due to herbal medication presents with abdominal pain, the possibility of lead poisoning should always be taken into consideration.
Keyword
MeSH Terms
-
Acute Disease
Alanine Transaminase/analysis
Aspartate Aminotransferases/analysis
Chemical and Drug Induced Liver Injury/*diagnosis
Hemoglobins/analysis
Humans
Lead/analysis
*Lead Poisoning
Liver/enzymology/metabolism
Liver Function Tests
Male
Middle Aged
Plants, Medicinal/chemistry
Alanine Transaminase
Aspartate Aminotransferases
Hemoglobins
Lead
Figure
Reference
-
References
1. Lee YJ. A case study on the effect of chelation therapy with di-mercaptosuccinic acid (DMSA) for lead poisoning in an adult. Korean J Occup Environ Med. 2010; 22:69–76.
Article2. Fung HT, Fung CW, Kam CW. Lead poisoning after ingestion of home-made Chinese medicines. Emerg Med (Fremantle). 2003; 15:518–520.
Article3. Navarro VJ, Barnhart H, Bonkovsky HL, et al. Liver injury from herbals and dietary supplements in the U.S. Drug-Induced Liver Injury Network. Hepatology. 2014; 60:1399–1408.
Article4. Kim JY, Kim JH, Kim HW, et al. A review of lead poisoning cases reported for recent 30 years in Korea. Korean J Med. 2004; 66:617–624.5. Park JU, Oh SW, Kim SH, Kim YH, Park RJ, Moon JD. A study on the association between blood lead levels and habitual tobacco and alcohol use in koreans with no occupational lead exposure. Korean J Occup Environ Med. 2008; 20:165–173.
Article6. Fowler BA, Nordberg GF, Nordberg M, Friberg L. Handbook on the toxicology of metals. London: Academic Press;2011.7. Anderson NR, Gama R, Kapadia S. Herbal remedy poisoning presenting with acute abdomen and raised urine porphyrins. Ann Clin Biochem. 2001; 38:408–410.
Article8. Hill GJ, Hill S. Lead poisoning due to hai ge fen. JAMA. 1995; 273:24–25.
Article9. Lord GM, Tagore R, Cook T, Gower P, Pusey CD. Nephropathy caused by Chinese herbs in the UK. Lancet. 1999; 354:481–482.
Article10. Pagliuca A, Mufti GJ, Baldwin D, Lestas AN, Wallis RM, Bellin-gham AJ. Lead poisoning: clinical, biochemical, and haematological aspects of a recent outbreak. J Clin Pathol. 1990; 43:277–281.
Article11. Oh SW, Lee HJ, Chae HJ, Lee SK, Moon JD, Cho D. A case of lead poisoning after ingestion of herb pills. Korean J Occup Environ Med. 2007; 19:231–237.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Drug Induced Liver Disease Caused by Ingestion of Dyctamnus dasycarpus
- A Case of Acute Pancreatitis and Acute Hepatitis Caused by Ingestion of Ceramium kondoi
- Applicability of Two Clinical Scales for Causality Assessment in Acute Liver Injury Caused by Herbal Medicines or Health Tonics
- A Case of Lead Poisoning by Ingesting Herbal Pills Tainted by Lead during the Manufacturing Process
- Severe but reversible acute kidney injury resulting from Amanita punctata poisoning