Korean J Gastroenterol.
2015 Feb;65(2):90-98. 10.4166/kjg.2015.65.2.90.
Additional Polyp Detection Rate Using Colonoscopic Retroflexion in Right Colon
- Affiliations
-
- 1Department of Internal Medicine, Jeju National University School of Medicine, Jeju, Korea. Kimhup@jejunu.ac.kr
- KMID: 2373189
- DOI: http://doi.org/10.4166/kjg.2015.65.2.90
Abstract
- BACKGROUND/AIMS
There have been several studies showing that retroflexion (RF) in the right colon (RC) could reduce the polyp miss rate of proximal colon during colonoscopy. This study was conducted to evaluate the additional benefit of RF technique in the RC.
METHODS
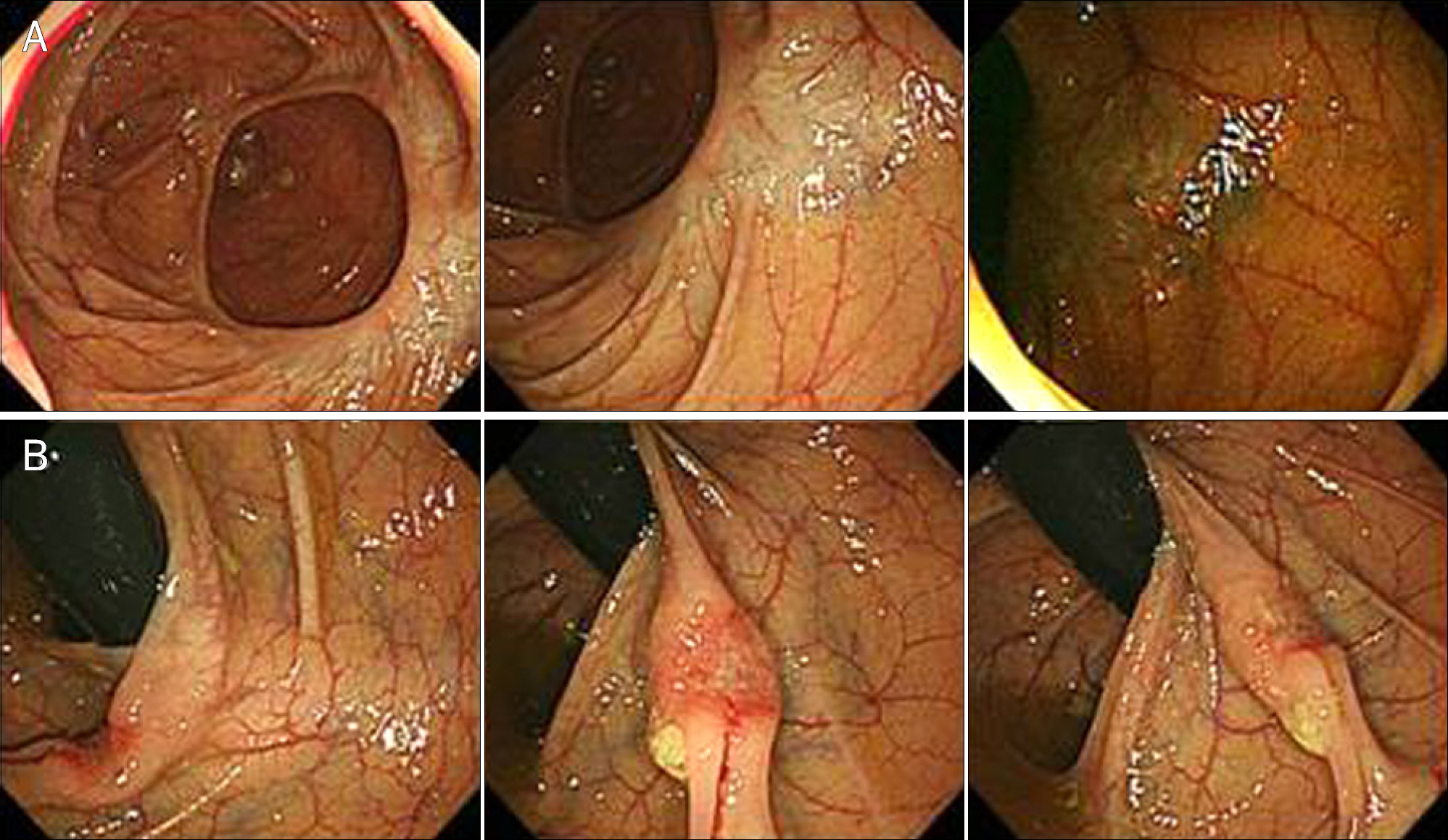
Patients who underwent colonoscopy from May 2008 to April 2011 were enrolled in the study. Data were obtained by retrospectively reviewing the medical records. RF was attempted in every patients undergoing colonoscopy since May 2008 except in cases of small RC vault, co-morbidity, severe diverticulosis, failed RF despite two trials, complaints of severe abdominal pain, or time burden. At first, RC was examined under direct vision. It was then examined by RF to detect missed polyps during the initial observation. Finally, the RC was re-examined with direct view.
RESULTS
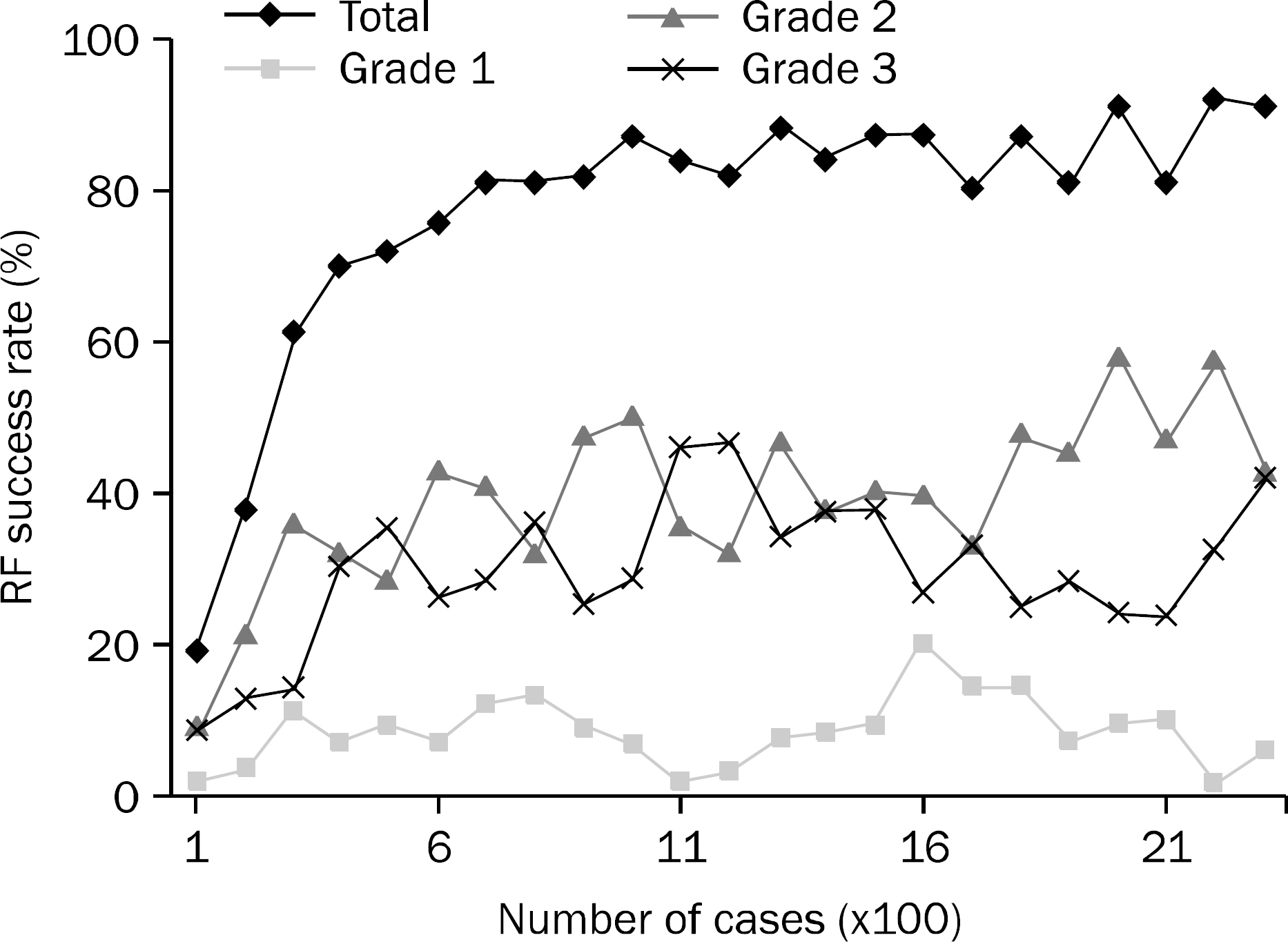
The cumulative RF success rate in the RC was 78.84% (1,805 of 2,319). The RF success rate increased with the number of cases (50% at 160 cases, 70% at 400 cases, and reached near 90% over 1,000 cases). Few polyps (4.88%) were detected only with RF and the additional adenoma detection rate was 3.32%. The additional polyp/adenoma detection rates were higher in the old age group (p<0.01). There were no RF associated perforation or severe complication.
CONCLUSIONS
Using RF examination, additional 4.88% of polyps could be detected in the RC. This technique could be a useful and safe method to detect hidden polyp during colonoscopy.
MeSH Terms
Figure
Reference
-
References
1. The Korea Central Cancer Registry, National Cancer Center. Annual report of cancer statistics in Korea in 2011. Sejong: Ministry of Health and Welfare;2013.2. Lieberman DA, Weiss DG, Bond JH, Ahnen DJ, Garewal H, Chejfec G. Veterans Affairs Cooperative Study Group 380. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. N Engl J Med. 2000; 343:162–168.
Article3. Lakoff J, Paszat LF, Saskin R, Rabeneck L. Risk of developing proximal versus distal colorectal cancer after a negative colonoscopy: a population-based study. Clin Gastroenterol Hepatol. 2008; 6:1117–1121. quiz 1064.
Article4. Brenner H, Hoffmeister M, Arndt V, Stegmaier C, Altenhofen L, Haug U. Protection from right- and left-sided colorectal neoplasms after colonoscopy: population-based study. J Natl Cancer Inst. 2010; 102:89–95.
Article5. Singh H, Nugent Z, Demers AA, Kliewer EV, Mahmud SM, Bernstein CN. The reduction in colorectal cancer mortality after colonoscopy varies by site of the cancer. Gastroenterology. 2010; 139:1128–1137.
Article6. Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009; 150:1–8.
Article7. Singh H, Nugent Z, Mahmud SM, Demers AA, Bernstein CN. Predictors of colorectal cancer after negative colonoscopy: a population-based study. Am J Gastroenterol. 2010; 105:663–673. quiz 674.
Article8. Bressler B, Paszat LF, Chen Z, Rothwell DM, Vinden C, Rabeneck L. Rates of new or missed colorectal cancers after colonoscopy and their risk factors: a population-based analysis. Gastroenterology. 2007; 132:96–102.
Article9. Soetikno RM, Kaltenbach T, Rouse RV, et al. Prevalence of non-polypoid (flat and depressed) colorectal neoplasms in asymptomatic and symptomatic adults. JAMA. 2008; 299:1027–1035.
Article10. Heresbach D, Barrioz T, Lapalus MG, et al. Miss rate for colorectal neoplastic polyps: a prospective multicenter study of back-to-back video colonoscopies. Endoscopy. 2008; 40:284–290.
Article11. Rondagh EJ, Bouwens MW, Riedl RG, et al. Endoscopic appear-ance of proximal colorectal neoplasms and potential implications for colonoscopy in cancer prevention. Gastrointest Endosc. 2012; 75:1218–1225.
Article12. Kahi CJ, Hewett DG, Norton DL, Eckert GJ, Rex DK. Prevalence and variable detection of proximal colon serrated polyps during screening colonoscopy. Clin Gastroenterol Hepatol. 2011; 9:42–46.
Article13. Farrar WD, Sawhney MS, Nelson DB, Lederle FA, Bond JH. Colorectal cancers found after a complete colonoscopy. Clin Gastroenterol Hepatol. 2006; 4:1259–1264.
Article14. Hetzel JT, Huang CS, Coukos JA, et al. Variation in the detection of serrated polyps in an average risk colorectal cancer screening cohort. Am J Gastroenterol. 2010; 105:2656–2664.
Article15. Rex DK, Khashab M. Colonoscopic polypectomy in retroflexion. Gastrointest Endosc. 2006; 63:144–148.
Article16. Hewett DG, Rex DK. Miss rate of right-sided colon examination during colonoscopy defined by retroflexion: an observational study. Gastrointest Endosc. 2011; 74:246–252.
Article17. Bretagne JF, Hamonic S, Piette C, et al. Variations between endoscopists in rates of detection of colorectal neoplasia and their impact on a regional screening program based on colonoscopy after fecal occult blood testing. Gastrointest Endosc. 2010; 71:335–341.
Article18. Chen SC, Rex DK. Endoscopist can be more powerful than age and male gender in predicting adenoma detection at colonoscopy. Am J Gastroenterol. 2007; 102:856–861.
Article19. Chan MY, Cohen H, Spiegel BM. Fewer polyps detected by colonoscopy as the day progresses at a Veteran's Administration teaching hospital. Clin Gastroenterol Hepatol. 2009; 7:1217–1223. quiz 1143.
Article20. Pickhardt PJ, Choi JR, Hwang I, et al. Computed tomographic vir-tual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. N Engl J Med. 2003; 349:2191–2200.
Article21. Pickhardt PJ, Nugent PA, Mysliwiec PA, Choi JR, Schindler WR. Location of adenomas missed by optical colonoscopy. Ann Intern Med. 2004; 141:352–359.
Article22. Froehlich F, Wietlisbach V, Gonvers JJ, Burnand B, Vader JP. Impact of colonic cleansing on quality and diagnostic yield of colonoscopy: the European Panel of Appropriateness of Gastrointestinal Endoscopy European multicenter study. Gastrointest Endosc. 2005; 61:378–384.
Article23. East JE, Saunders BP, Burling D, Boone D, Halligan S, Taylor SA. Surface visualization at CT colonography simulated colonoscopy: effect of varying field of view and retrograde view. Am J Gastroenterol. 2007; 102:2529–2535.
Article24. Dik VK, Moons LM, Siersema PD. Endoscopic innovations to in-crease the adenoma detection rate during colonoscopy. World J Gastroenterol. 2014; 20:2200–2211.
Article25. Gralnek IM, Carr-Locke DL, Segol O, et al. Comparison of standard forward-viewing mode versus ultrawide-viewing mode of a novel colonoscopy platform: a prospective, multicenter study in the detection of simulated polyps in an in vitro colon model (with video). Gastrointest Endosc. 2013; 77:472–479.
Article26. Ng SC, Tsoi KK, Hirai HW, et al. The efficacy of cap-assisted colonoscopy in polyp detection and cecal intubation: a meta-analysis of randomized controlled trials. Am J Gastroenterol. 2012; 107:1165–1173.
Article27. Waye JD, Heigh RI, Fleischer DE, et al. A retrograde-viewing device improves detection of adenomas in the colon: a prospective efficacy evaluation (with videos). Gastrointest Endosc. 2010; 71:551–556.
Article28. DeMarco DC, Odstrcil E, Lara LF, et al. Impact of experience with a retrograde-viewing device on adenoma detection rates and withdrawal times during colonoscopy: the Third Eye Retroscope study group. Gastrointest Endosc. 2010; 71:542–550.
Article29. Cutler AF, Pop A. Fifteen years later: colonoscopic retroflexion revisited. Am J Gastroenterol. 1999; 94:1537–1538.
Article30. Grobe JL, Kozarek RA, Sanowski RA. Colonoscopic retroflexion in the evaluation of rectal disease. Am J Gastroenterol. 1982; 77:856–858.31. Hanson JM, Atkin WS, Cunliffe WJ, et al. Rectal retroflexion: an essential part of lower gastrointestinal endoscopic examination. Dis Colon Rectum. 2001; 44:1706–1708.32. Varadarajulu S, Ramsey WH. Utility of retroflexion in lower gastrointestinal endoscopy. J Clin Gastroenterol. 2001; 32:235–237.
Article33. Harrison M, Singh N, Rex DK. Impact of proximal colon retroflexion on adenoma miss rates. Am J Gastroenterol. 2004; 99:519–522.
Article34. Pishvaian AC, Al-Kawas FH. Retroflexion in the colon: a useful and safe technique in the evaluation and resection of sessile polyps during colonoscopy. Am J Gastroenterol. 2006; 101:1479–1483.
Article35. Kessler WR, Rex DK. Impact of bending section length on insertion and retroflexion properties of pediatric and adult colonoscopes. Am J Gastroenterol. 2005; 100:1290–1295.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is Retroflexion Helpful in Detecting Adenomas in the Right Colon?: A Single Center Interim Analysis
- The Colonoscopic Withdrawal Time is Correlated with the Rate of Detecting Polyps When Performing Colonoscopy
- Colorectal Polyps : Endoscopic Diagnosis and Polypectomy
- The Recurrence Rate of Colon Polyp after Polypectomy and the Interval of Surveillance Colonoscopy: Predictors of Early Development of Advanced Polyp
- Risk Factors for Incomplete Polyp Resection during Colonoscopic Polypectomy