J Gastric Cancer.
2017 Mar;17(1):11-20. 10.5230/jgc.2017.17.e2.
Effect of Acupuncture on Postoperative Ileus after Distal Gastrectomy for Gastric Cancer
- Affiliations
-
- 1Department of Surgery, Catholic University of Daegu School of Medicine, Daegu, Korea. kih2yk@cu.ac.kr
- 2Department of Radiology, Catholic University of Daegu School of Medicine, Daegu, Korea.
- 3Department of Internal Medicine, College of Korean Medicine, Daegu Haany University, Daegu, Korea.
- KMID: 2372578
- DOI: http://doi.org/10.5230/jgc.2017.17.e2
Abstract
- PURPOSE
Acupuncture has recently been accepted as a treatment option for managing postoperative ileus (POI) and various functional gastrointestinal disorders. Therefore, we conducted a prospective randomized study to evaluate the effect of acupuncture on POI and other surgical outcomes in patients who underwent gastric surgery.
MATERIALS AND METHODS
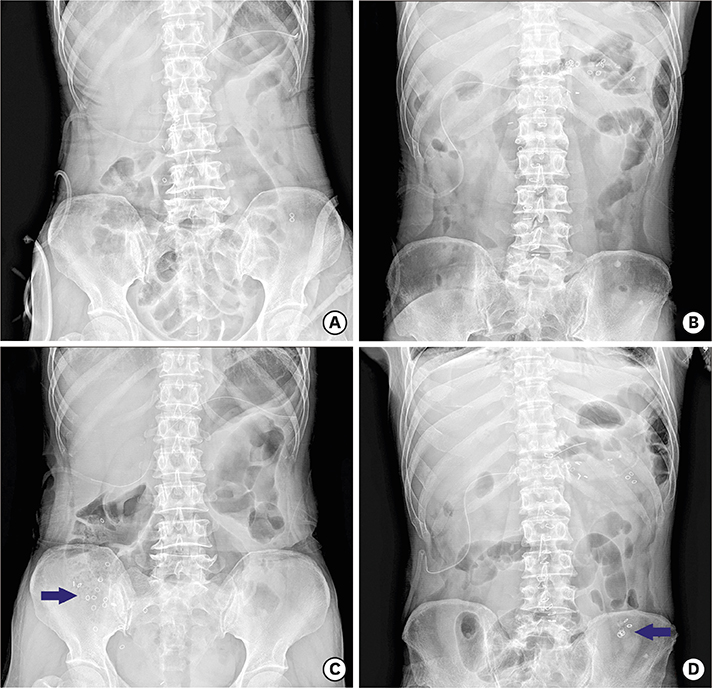
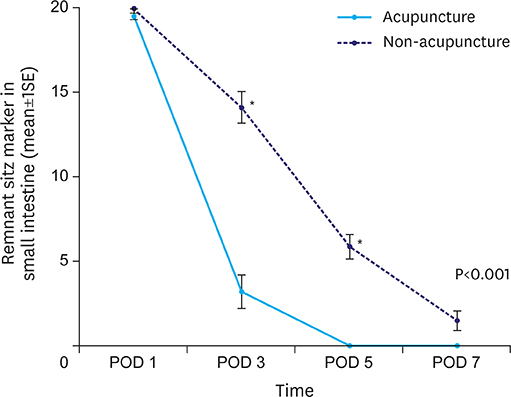
Thirty-six patients who underwent distal gastrectomy for gastric cancer from March to December 2015 were randomly assigned to acupuncture or non-acupuncture (NA) groups at 1:1 ratio. The acupuncture treatment was administered treatment once daily for 5 consecutive days starting at postoperative day 1. The primary outcome measure was the number of remnant sitz markers in the small intestine on abdominal radiograph. The secondary outcome measure was the surgical outcome, including the times to first flatus, first defecation, start of water intake, and start of soft diet, as well as length of hospital stay and laboratory findings.
RESULTS
The acupuncture group had significantly fewer remnant sitz markers in the small intestine on postoperative days 3 and 5 compared to those in the NA group. A significant difference was observed in the numbers of remnant sitz markers in the small intestine with respect to group differences by time (P<0.0001). The acupuncture group showed relatively better surgical outcomes than those in the NA group, but the differences were not statistically significant.
CONCLUSIONS
In this clinical trial, acupuncture promoted the passage of sitz markers, which may reflect the possibility of reducing POI after distal gastrectomy.
MeSH Terms
Figure
Reference
-
1. Luckey A, Livingston E, Taché Y. Mechanisms and treatment of postoperative ileus. Arch Surg. 2003; 138:206–214.2. Townsend CM, Beauchamp RD, Evers BM, Mattox KL, editors. Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 19th ed. Philadelphia (PA): Elsevier Saunders;2012.3. Liu SS, Carpenter RL, Mackey DC, Thirlby RC, Rupp SM, Shine TS, et al. Effects of perioperative analgesic technique on rate of recovery after colon surgery. Anesthesiology. 1995; 83:757–765.4. Holte K, Kehlet H. Postoperative ileus: progress towards effective management. Drugs. 2002; 62:2603–2615.5. Ng SS, Leung WW, Mak TW, Hon SS, Li JC, Wong CY, et al. Electroacupuncture reduces duration of postoperative ileus after laparoscopic surgery for colorectal cancer. Gastroenterology. 2013; 144:307–313.e1.6. Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Ann Intern Med. 2002; 136:374–383.7. White A; Editorial Board of Acupuncture in Medicine. Western medical acupuncture: a definition. Acupunct Med. 2009; 27:33–35.8. Ouyang H, Chen JD. Review article: therapeutic roles of acupuncture in functional gastrointestinal disorders. Aliment Pharmacol Ther. 2004; 20:831–841.9. Takahashi T. Acupuncture for functional gastrointestinal disorders. J Gastroenterol. 2006; 41:408–417.10. Iwa M, Matsushima M, Nakade Y, Pappas TN, Fujimiya M, Takahashi T. Electroacupuncture at ST-36 accelerates colonic motility and transit in freely moving conscious rats. Am J Physiol Gastrointest Liver Physiol. 2006; 290:G285–G292.11. Luo D, Liu S, Xie X, Hou X. Electroacupuncture at acupoint ST-36 promotes contractility of distal colon via a cholinergic pathway in conscious rats. Dig Dis Sci. 2008; 53:689–693.12. Balestrini JL, Tsuchida D, Fukuda H, Pappas TN, Takahashi T. Acupuncture accelerates delayed gastrointestinal transit after abdominal surgery in conscious rats. Scand J Gastroenterol. 2005; 40:734–735.13. Sugai GC, Freire AO, Tabosa A, Yamamura Y, Tufik S, Mello LE. Serotonin involvement in the electroacupuncture- and moxibustion-induced gastric emptying in rats. Physiol Behav. 2004; 82:855–861.14. Tabosa A, Yamamura Y, Forno ER, Mello LE. Effect of the acupoints ST-36 (Zusanli) and SP-6 (Sanyinjiao) on intestinal myoelectric activity of Wistar rats. Braz J Med Biol Res. 2002; 35:731–739.15. Choi M, Jung J, Seo M, Lee K, Nam T, Yang I, et al. Ultrasonographic observation of intestinal mobility of dogs after acupunctural stimulation on acupoints ST-36 and BL-27. J Vet Sci. 2001; 2:221–226.16. Chou JW, Chang YH, Chang CS, Chen GH. The effect of different frequency electrical acu-stimulation on gastric myoelectrical activity in healthy subjects. Hepatogastroenterology. 2003; 50:582–586.17. Chang CS, Ko CW, Wu CY, Chen GH. Effect of electrical stimulation on acupuncture points in diabetic patients with gastric dysrhythmia: a pilot study. Digestion. 2001; 64:184–190.18. Chen LL, Hsu SF, Wang MH, Chen CL, Lin YD, Lai JS. Use of acupressure to improve gastrointestinal motility in women after trans-abdominal hysterectomy. Am J Chin Med. 2003; 31:781–790.19. Liu JX, Zhao Q. Effect of acupuncture on intestinal motion and sero-enzyme activity in perioperation. Zhong Xi Yi Jie He Za Zhi. 1991; 11:156–157. 133–134.20. Wan Q. Auricular-plaster therapy plus acupuncture at zusanli for postoperative recovery of intestinal function. J Tradit Chin Med. 2000; 20:134–135.21. Meng ZQ, Garcia MK, Chiang JS, Peng HT, Shi YQ, Fu J, et al. Electro-acupuncture to prevent prolonged postoperative ileus: a randomized clinical trial. World J Gastroenterol. 2010; 16:104–111.22. Deng G, Wong WD, Guillem J, Chan Y, Affuso T, Yeung KS, et al. A phase II, randomized, controlled trial of acupuncture for reduction of Postcolectomy Ileus. Ann Surg Oncol. 2013; 20:1164–1169.23. Lin JG, Lo MW, Wen YR, Hsieh CL, Tsai SK, Sun WZ. The effect of high and low frequency electroacupuncture in pain after lower abdominal surgery. Pain. 2002; 99:509–514.24. Tan EK, Cornish J, Darzi AW, Tekkis PP. Meta-analysis: Alvimopan vs. placebo in the treatment of post-operative ileus. Aliment Pharmacol Ther. 2007; 25:47–57.25. Bungard TJ, Kale-Pradhan PB. Prokinetic agents for the treatment of postoperative ileus in adults: a review of the literature. Pharmacotherapy. 1999; 19:416–423.26. Maurer AH, Krevsky B. Whole-gut transit scintigraphy in the evaluation of small-bowel and colon transit disorders. Semin Nucl Med. 1995; 25:326–338.27. Maurer AH, Parkman HP. Update on gastrointestinal scintigraphy. Semin Nucl Med. 2006; 36:110–118.28. Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K, et al. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr. 2005; 24:466–477.29. Basse L, Madsen JL, Kehlet H. Normal gastrointestinal transit after colonic resection using epidural analgesia, enforced oral nutrition and laxative. Br J Surg. 2001; 88:1498–1500.30. Zingg U, Miskovic D, Pasternak I, Meyer P, Hamel CT, Metzger U. Effect of bisacodyl on postoperative bowel motility in elective colorectal surgery: a prospective, randomized trial. Int J Colorectal Dis. 2008; 23:1175–1183.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Distal Gastrectomy for Gastric Cancer
- Entirely Laparoscopic Gastrectomy and Colectomy for Remnant Gastric Cancer with Gastric Outlet Obstruction and Transverse Colon Invasion
- Corrigendum: Comparison of Short-Term Postoperative Outcomes in Totally Laparoscopic Distal Gastrectomy Versus Laparoscopy-Assisted Distal Gastrectomy
- Role of Distal Pancreatectomy on the Prognosis of Gastric Cancer Patients Undergoing Total Gastrectomy
- High rates of complications in advanced stage gastric cancer after laparoscopic gastrectomy